Table 30-1. Topical Antimicrobials

Patient counseling
■ Wait at least 1 hour before applying any other topical acne medication.
■ Avoid contact with eyes, mouth, nose, and other mucous membranes.
■ Although improvement is generally expected within 4 weeks, some patients do not respond for 8–12 weeks.
Adverse effects
■ More common: Dry or scaly skin, irritation, itching
■ Less common: Stinging sensation, peeling, redness
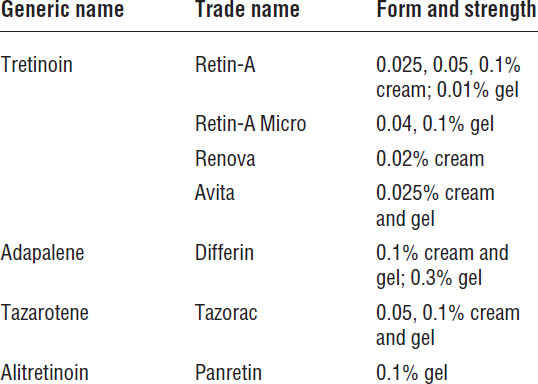
Retinoids
See Table 30-2 for information about retinoids.
Mechanism of action
■ Retinoids are chemically related to vitamin A.
■ Retinoids normalize follicular keratinization, heal comedones, decrease sebum production, and decrease inflammatory lesions.
Patient counseling
■ Do not use astringents, drying agents, abrasive scrubs, or harsh soaps concurrently, and use mild soap only once or twice daily.
■ Apply every other night to adjust to drying effect for the first 2 weeks.
■ Apply nightly after 2 weeks.
■ Expect that it may take up to 2–3 months for skin to improve.
■ Use sunblock on face before sun exposure because of increased sensitivity.
Adverse drug effects
■ These agents may irritate skin and cause redness, dryness, and scaling.
■ Tazarotene is the most irritating retinoid.
■ Adapalene appears to be least irritating and is preferred for sensitive skin.
Azelaic acid 20%
Trade names are Azelex and Finacea.
Mechanism of action
Azelaic acid 20% suppresses growth of P. acnes. It improves inflammatory and noninflammatory lesions. It normalizes keratinization, leading to an anticomedonal effect.
Patient counseling
■ If sensitivity develops, discontinue use.
■ Keep away from mouth, eyes, and mucous membranes.
■ Other topical medications must be used at different times during the day.
Adverse drug effects
■ Temporary dryness and skin irritation (pruritus and burning) may occur on initiation of therapy.
■ Hypopigmentation may occur (caution in dark-skinned individuals).
Topical Dapsone 5%
Trade name is Aczone.
Mechanism of action
Dapsone has anti-inflammatory and antimicrobial properties and can be used to reduce the number of acne lesions in patients over 12 years old. May consider in patients unable to tolerate other topical acne medications.
Patient counseling
■ If sensitivity develops, discontinue use.
■ Keep away from mouth, eyes, and mucous membranes.
Adverse drug effects
■ Peeling, dryness and erythema
■ Phototoxicity
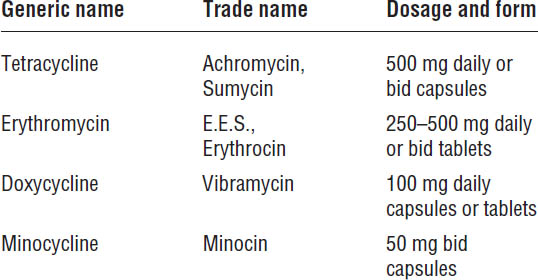
Systemic Therapy
Antimicrobials
Antimicrobials are useful for type II (papular) acne and type III (pustular) acne.
Dosing
See Table 30-3 for information about dosage. After 6–8 weeks, dosage may be increased if necessary. If the first antibiotic was ineffective after increasing the dosage, a second antibiotic is prescribed.
After 6 months to 1 year of therapy, the antibiotic dose may be tapered if continued at all.
Mechanism of action
Antimicrobials suppress growth of P. acnes in sebaceous ducts. These agents possibly have a direct anticomedonal effect.
Patient counseling, adverse drug effects, and drug interactions
See Chapter 34 on anti-infective agents.
Isotretinoin
Isotretinoin is available in 10, 20, 30, and 40 mg capsules. Trade names are Accutane, Amnesteem, and Claravis.
Isotretinoin is for patients with severe, nodulocystic, draining acne who have not responded to systemic antibiotic therapy or who have required more than 3 years of systemic antibiotic therapy.
This agent is over 90% effective in producing an acne-free state for years following a 4- to 5-month course of therapy. Originally held in reserve for severe cases of nodulocystic acne, isotretinoin may also be indicated as first-line treatment for severe acne that results in scarring.
Table 30-3. Oral Antimicrobials
iPLEDGE program
The U.S. Food and Drug Administration (FDA) approved an enhanced risk-management program, designed to minimize fetal exposure to isotretinoin, known as iPLEDGE. iPLEDGE requires mandatory registration of prescribers, patients, wholesalers, and pharmacies to further the public health goal of eliminating fetal exposure to isotretinoin.
Pharmacies are not able to dispense isotretinoin to people with severe acne who do not enroll in the iPLEDGE program through a health care provider who is also enrolled. After a pharmacy registers for iPLEDGE at www.ipledgeprogram.com, the “Responsible Site Pharmacist” is sent a follow-up mailing, which contains instructions on how to activate the pharmacy.
The iPLEDGE program requires that all patients meet qualification criteria and monthly program requirements. Before the patient receives his or her isotretinoin prescription each month, the prescriber must counsel the patient about the risks of isotretinoin and document it in the iPLEDGE system.
Mechanism of action
Isotretinoin reduces sebum production up to 90%. It decreases production of microcomedones, possibly by decreasing cohesiveness of follicular epithelial cells. It can have an anti-inflammatory effect.
Patient counseling
■ Isotretinoin should be taken with food and is best absorbed with a fatty meal.
■ Patients can take the dose divided twice daily or the entire dose with the evening meal.
■ Effects are gradual, and acne may worsen during the first month of therapy. However, improvement usually begins by the sixth week of therapy.
■ Use lip balm to treat cheilitis and moisturizers to treat dry skin.
Adverse drug effects
Isotretinoin is teratogenic. It is absolutely contraindicated in pregnancy because it causes significant birth defects. Females of childbearing potential must take measures to avoid pregnancy during the course of isotretinoin therapy.
Females should be tested for pregnancy before initiation of therapy and told to use two methods of contraception for at least 1 month prior to initiation of therapy and for 1 month after discontinuation of therapy.
Side effects and toxicity
■ Most common (90–100%):
• Cheilitis (chapped lips)
• Dry mouth
• Dry skin
• Pruritus
■ Common (30–40%):
• Dry nose, leading to nasal crusting and epistaxis
• Dry eyes, leading to conjunctivitis and problems with contact lenses
• Muscular soreness or stiffness
■ Less common (10–25%):
• Headaches
• Hyperlipidemia (primarily elevation of triglycerides, which may lead to attack of pancreatitis)
■ Rare (less than 5%):
• Decreased night vision
• Thinning of hair
• Easily injured skin
• Peeling of palms and soles
• Skin rash and skin infections
■ Very rare (< 1%):
• Acute depression (very rare, but reversible if detected early)
• Pseudotumor cerebri (benign intracranial hypertension with visual disturbances)
■ Treatment of most common side effects:
• Cheilitis: Frequent use of lip balm
• Dry skin: Skin lubrication with moisturizers
• Nosebleeds: Lubrication of the nostrils with petrolatum
• Muscular soreness or stiffness: Use of mild OTC analgesic and anti-inflammatory agents
Monitoring parameters
■ Lipid panel
■ Liver function tests (elevations common during initiation of therapy; usually return to normal during treatment)
■ Complete blood counts
■ Pregnancy testing for women prior to use of drug
Dosing
The dosage is 1 mg/kg once or twice daily with food; however, the patient may start out with 0.5 mg/kg/day for the first month before increasing. Isotretinoin is best absorbed with a fatty meal.
The goal is a total dose of 120–150 mg/kg over 4–5 months. Longer courses of 6–8 months may be required.
Other aspects
Approximately 20% of patients relapse within 1 year, and up to 40% relapse within 3 years after discontinuation of therapy. Repeat therapy for 4–6 months is acceptable and effective.
Oral corticosteroids
Oral corticosteroids are commonly known as “prom pills.” These agents can temporarily suppress acne with a 7- to 10-day course of prednisone 20 mg daily. They are rapidly effective when a brief course is necessary to cause prompt improvement (e.g., important social event such as wedding, prom, and so forth).
Systemic corticosteroids used continuously may actually cause or worsen acne. Topical corticosteroids have no value in the treatment of acne, and high-potency topical corticosteroids will aggravate acne and should never be used on the faces of acne patients.
30-4. Fungal Skin Infections
Tinea are skin infections known as dermatomycoses caused by the fungi Trichophyton, Microsporum, and Epidermophyton.
Classification
■ Tinea pedis (athlete’s foot)
■ Tinea capitis (ringworm of the scalp)
■ Tinea cruris (jock itch)
■ Tinea corporis (ringworm of the skin)
■ Tinea unguium (onychomycosis: fungal infection of toenails and fingernails)
Pathophysiology
The fungi invade dead cells of the stratum corneum of skin, hair, and nails, digesting keratin. Unlike Candida, they cannot exist on unkeratinized mucous membranes.
This condition is more common in immunosuppressed patients.
Treatment Principles and Goals
■ Tinea pedis: Self-treat topically initially; if ineffective, add oral agents.
■ Tinea capitis: Use oral systemic therapy.
■ Tinea cruris: Self-treat topically initially; if ineffective, add oral agents.
■ Tinea corporis: Self-treat topically initially; if ineffective, add oral agents.
■ Tinea unguium: Use oral systemic therapy.
Drug Therapy
OTC treatment
■ Terbinafine 1% (Lamisil AT) cream, gel, and spray (most effective OTC antifungal agent)
■ Miconazole 2% (Micatin, Cruex Spray powder)
■ Clotrimazole 1% (Lotrimin AF lotion, solution, and cream)
■ Tolnaftate 1% (Tinactin, Blis-To-Sol, Ting)
■ Undecylenic acid 10–25% (Desenex)
Prescription treatment
See Table 30-4 for a description of prescription drugs.
Topical treatments
Newer antifungals are initially applied only once daily, and recurrences can be prevented by once- or twice-weekly applications.
Systemic therapy
Occasionally, topical therapy is not effective for tinea pedis, tinea cruris, and tinea corporis, and systemic antifungal therapy is required. Systemic therapy is also required for tinea capitis (ringworm of the scalp) and tinea unguium (fungal infection of the toenails and fingernails). Medications are as follows:
■ Griseofulvin
■ Ketoconazole
■ Fluconazole
■ Itraconazole
■ Terbinafine
See Chapter 34 on anti-infective agents for discussion of systemic antifungals.
Table 30-4. Prescription Topical Antifungals
Generic name | Trade name |
Econazole | Ecoza foam, cream |
Naftifine | Naftin gel, cream |
Ciclopirox | Loprox gel, cream, lotion; Penlac solution |
Butenafine | Mentax cream, Lotrimin Ultra cream |
30-5. Hair Loss (Alopecia)
Male pattern baldness (androgenic alopecia) is the gradual and progressive loss of hair in males as they age.
Clinical Presentation
■ Onset and progression vary greatly.
■ A distinct pattern of progressive hair loss develops in the frontotemporal areas and crown with sparing of the occiput.
■ Hair loss is limited to the scalp.
■ Miniaturization of hair is seen, where normal thick terminal hairs are converted to very fine vellus hairs.
Pathophysiology
Alopecia is primarily due to two factors:
■ Heredity (genetic)
■ Testosterone
Testosterone, which promotes growth of hair in the beard, axillae, pubis, and other parts of the body, does not promote the growth of scalp hair. It contributes to premature hair loss because it is converted by the enzyme 5-α-reductase to dihydrotestosterone, which binds preferentially to receptors in the hair follicles on the scalp and causes them to produce progressively thinner hair until the follicles eventually cease activity altogether.
Treatment Principles and Goals
Although androgenic alopecia has no cure, two drugs are available for its treatment:
■ Minoxidil (Rogaine, available OTC)
■ Finasteride (Propecia, by prescription only)
In alopecia’s early stages, topical minoxidil or oral finasteride may reverse the gradually decreasing diameter of the hair shaft.
Any hair growth stimulation is temporary and lasts only as long as therapy continues. If therapy is discontinued, new hair growth is lost within 1 year.
Early hair loss occurring recently in younger men is more likely to respond to treatment than later hair loss at an older age or when hair loss is not recent.
Alopecia of the crown in males responds better to treatment than does hair loss in the frontotemporal area.
Drug Therapy
Minoxidil
OTC trade names are Rogaine 2% and Rogaine Extra Strength 5%.
Mechanism of action
Minoxidil probably increases cutaneous blood flow directly to hair follicles because of vasodilation. It possibly stimulates resting hair follicles (telogen phase) into active growth (anagen phase). It possibly stimulates hair follicle cells.
Patient counseling
■ Apply 1 mL twice daily (approximately one 60 mL bottle each month).
■ Minoxidil may be applied without shampooing hair.
■ Use at least 4 hours before bedtime to avoid oil on pillows and bed linens.
■ The drug is absorbed over a 4-hour period, so do not swim, shampoo, or walk in rain for 4 hours.
■ Wash hands immediately after application to prevent unwanted absorption.
■ Do not inhale mist because systemic absorption is possible.
■ Do not use on infected, irritated, inflamed, or sunburned skin.
■ Discontinue use immediately and contact your health care provider if chest pain, increased heart rate, faintness, dizziness, or swollen hands or feet occur.
■ Women should avoid 5% strength (which has no better results than 2%); they have greater incidence of increased growth of facial hair with the 5% solution.
■ Generally, treatment takes 4–6 months before any benefit occurs.
■ No effects within 8 months for females and 12 months for males indicate therapeutic failure, and treatment should be discontinued.
■ Patients must continue using minoxidil to maintain new hair growth.
Adverse drug effects
■ Scalp dermatitis is common, producing dryness, pruritus, and flaking or scaling.
■ Hypertrichosis (excessive hair growth) can occur on areas other than scalp (chest, forearms, ear rim, back, face, arms, and so forth).
■ Some women report unwanted facial hair growth when minoxidil is applied to scalp, primarily with the 5% solution.
■ Use may rarely produce systemic side effects (chest pain, increased heart rate, faintness, or dizziness).
■ Use is contraindicated in patients less than 18 years of age.
■ Use is contraindicated in women who are pregnant or breastfeeding.
Finasteride
The trade name of finasteride is Propecia 1 mg. It was originally developed for the treatment of benign prostatic hyperplasia in a 5 mg dose (Proscar). A 1 mg daily dose is approved for males only as prescription treatment for androgenic alopecia.
Over a two-year period, finasteride may halt the progressive hair loss caused by androgenic alopecia.
Mechanism of action
Finasteride inhibits the enzyme 5-α-reductase, which is responsible for the conversion of testosterone to the more powerful dihydrotestosterone—the main androgen responsible for androgenic hair loss.
Patient counseling
■ Take with or without food.
■ Take for at least 3 months to see if the drug is effective.
■ Improvement lasts only as long as treatment continues. New hair will be lost within 1 year of stopping treatment.
Adverse drug effects
■ Gynecomastia (breast enlargement and tenderness) has been reported from 2 weeks to 2 years following initial therapy, but it is usually reversible when therapy is discontinued.
■ Hypersensitivity (skin rash, swelling of lips) has been reported.
■ Decreased libido, erectile dysfunction, and ejaculatory dysfunction occur, which are reversible when the drug is discontinued.
■ Use is contraindicated in females of childbearing age, because of abnormalities of the external genitalia in male fetuses. Finasteride is not effective in postmenopausal females.
30-6. Dry Skin
This condition refers to lack of moisture or sebum in the stratum corneum. It most commonly occurs in the winter (also known as winter rash). It is more commonly present in older adults.
Clinical Presentation
■ Flaking and scaling
■ Xerosis and roughness
■ Pruritus
■ Loss of skin elasticity
Pathophysiology
Dry skin is due to inadequate moisture retention in the stratum corneum, which is caused by the following factors:
■ Decreased sebum production and decreasing moisture-binding capacity of skin in elderly patients
■ Low humidity, which causes the skin to lose water and become dry and hardened
■ Overexposure to sunlight
■ Excessive cleansing and bathing, which removes lipids and other skin components
■ Chronic skin diseases that impair moisture retention of skin (psoriasis, scleroderma, ichthyosis, contact dermatitis)
Treatment Principles and Goals
The goal of treatment is to increase the moisture level of the stratum corneum by increasing cell hydration and binding capacity, which improves skin permeability and restores elasticity.
Drug Therapy
Emollients and moisturizing agents
Emollients and moisturizing agents include petrolatum or mineral oil (Alpha Keri Shower and Bath Moisture Rich Oil). They increase the relative moisture content of the stratum corneum and produce a general soothing effect by reducing frictional heat and perspiration.
Humectants
Humectants include glycerin (e.g., Corn Huskers Lotion), propylene glycol, and phospholipids. They are hygroscopic agents that increase hydration of the stratum corneum.
Keratin-softening agents
Keratin-softening agents include the following:
■ Urea (10–30%) (e.g., Aqua Care, Carmol)
• Improves the skin’s moisture-binding capacity
• Provides keratolytic effect at higher concentrations
• May cause irritation and burning
■ Lactic acid (2–5%) (e.g., LactiCare)
• Increases skin hydration by controlling the rate of keratinization
• Is markedly hygroscopic
■ Allantoin (e.g., Alphosyl, Psorex, Tegrin)
• Relieves dry skin by disrupting keratin structure (less effective than urea)
• Desensitizes many skin-sensitizing drugs as a protectant
Antipruritic agents
Antipruritic agents include the following:
■ Camphor and menthol, which provide a cooling sensation
■ Local anesthetics (e.g., benzocaine, pramoxine)
■ Systemic antihistamines (H1-receptor antagonists), which have limited effectiveness
■ Colloidal oatmeal (e.g., Aveeno)
Caution: Colloidal oatmeal can cause an extremely slippery bathtub.
Hydrocortisone
Hydrocortisone reduces the inflammatory response that accompanies dry skin conditions. Although it does not directly increase skin hydration, it does prevent itching associated with dry skin and inhibits dehydration.
Ointment is better than cream for dry skin. Patients should be counseled as follows:
■ Use sparingly.
■ Do not use for more than 5–7 days for dry skin pruritus.
Astringents
Astringents include aluminum acetate 0.1–0.5% (e.g., Burow’s solution) and Hamamelis water (witch hazel).
Protectants
Zinc oxide is a protectant.
Nondrug Recommendations and Therapy
■ Bathe less frequently.
■ Reduce use of soap to a minimum, and use only where necessary.
■ Lubricate skin immediately after bathing (e.g., apply bath oil after bathing and before drying).
■ Use extrafatted soaps such as Basis.
Combination products to treat dry skin
■ Aveeno Soothing Bath Treatment: Colloidal oatmeal and mineral oil
■ Jergens Ultra Healing Extra Dry Skin Moisturizer: Dimethicone, cetearyl alcohol, petrolatum, and glycerin
■ Keri Original Dry Skin Lotion: Mineral oil, lanolin oil, glyceryl stearate, and propylene glycol
■ Moisturel Lotion: Petrolatum, dimethicone, cetyl alcohol, and glycerin
■ Neutrogena Body Oil: Isopropyl myristate and sesame seed oil
30-7. Dermatitis
Dermatitis is a nonspecific term describing a variety of inflammatory dermatologic conditions characterized by erythema. It is a general term describing any eczematous rash of unknown etiology that cannot be classified among the major endogenous dermatoses. Eczema and dermatitis are often used interchangeably.
Types and Classification
The major classifications or types of dermatitis are as follows:
■ Atopic dermatitis (atopic eczema)
■ Chronic dermatitis (hand dermatitis)
■ Contact dermatitis (irritant and allergic)
Clinical Presentation
Atopic dermatitis (atopic eczema)
Atopic dermatitis occurs primarily in infants and children. It may disappear before adulthood. The cause is unknown but is possibly genetic.
Atopic dermatitis is usually seen on the face, knees, elbows, and neck. It is frequently seen with asthma, allergic rhinitis, and urticaria. Exacerbating factors include soaps, detergents, chemicals, temperature changes, molds, and allergens.
Chronic dermatitis (hand dermatitis or hand eczema)
Chronic dermatitis, also known as eczema, is a stubborn, itchy rash that occurs in certain persons with sensitive or irritable skin. The skin is very dry and easily irritated by overuse of soaps or detergents and by rough clothing.
The condition is exacerbated by very hot or very cold weather. It is probably genetically determined. No permanent cure exists.
The condition usually can be controlled by enhancing skin hydration with emollients and moisturizers and by using hydrocortisone cream to relieve itching.
Contact dermatitis
Irritant contact dermatitis (chemical contact dermatitis)
The condition is caused by exposure to irritating substances producing mechanical or chemical trauma. Examples include soap, solvents, paints, abrasive cleansers, cosmetics, lubricants, antiseptics, cacti, rose hips, thorns, peppers, and tobacco.
Irritant contact dermatitis is not a sensitization, but direct toxicity to skin tissue.
Allergic contact dermatitis
The condition is a process of sensitization with reaction on elicitation. More than 50% of all dermatitis is allergic contact dermatitis.
Examples of reactive elements include benzocaine, zinc pyrithione (ZPT), neomycin, sodium bisulfite, perfumes, many cosmetics, skin lubricants, antiseptic creams, rubber and epoxy glues, poison ivy and oak, and many other common substances.
Treatment Principles and Goals
Treat dermatitis by applying a corticosteroid, according to the following principles:
■ Ointments and creams are more lubricating than solutions, lotions, or gels.
■ Ointments should be recommended if skin is dry.
■ Lotions or gels should be recommended for a weeping, eczematous dermatitis.
■ Lotions, solutions, and gels are easier to use in hairy areas of the body.
■ Apply small amounts of corticosteroid cream or ointment, and massage in gently but thoroughly.
■ Apply the moderate- and high-strength cortisones only once daily.
■ Improvement should begin within 1 week.
■ Avoid excess soap, and keep skin lubricated with moisturizers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


