Patient Story
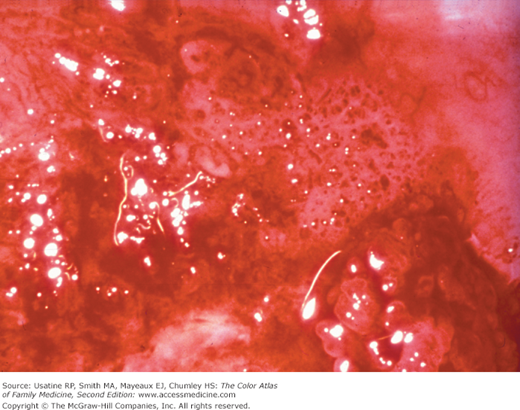
A 51-year-old woman presents with postcoital bleeding. She has not had a period in 3 years, but has started spotting after intercourse. Her last Papanicolaou (Pap) smear was after the birth of her last child 25 years ago and was normal. Other than an occasional mild hot flash, she has no other complaints. On colposcopy she was found to have a densely acetowhite lesion with abnormal vessel near the cervical os (Figure 91-1). Biopsy demonstrated invasive squamous cell carcinoma. The patient then had a radical hysterectomy with pelvic/paraaortic lymphadenectomy. Fortunately her lymph nodes were all negative.
Introduction
Colposcopy is an important visualization technique used to investigate abnormal Pap smears and to direct biopsies for histologic diagnosis of cervical cancer. Because human papillomavirus (HPV) is present in 95% to 100% of all squamous cell cancers (SCCs), the International Agency for Research on Cancer proclaimed cervical cancer to be the first human cancer known to have a single necessary cause.1,2
Epidemiology
- Carcinoma of the cervix is the second most common cancer in women worldwide with an estimated 400,000 to 500,000 cases of cervical cancer diagnosed each year.3,4
- In the United States, an estimated 12,170 new cases and approximately 4220 deaths occur annually, even though more than 50 million Pap smears are performed each year.5
- Half of the cases occur in women never screened and an additional 10% in women not screened within the past 5 years.6
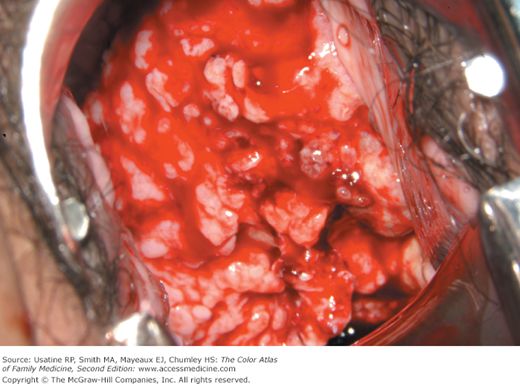
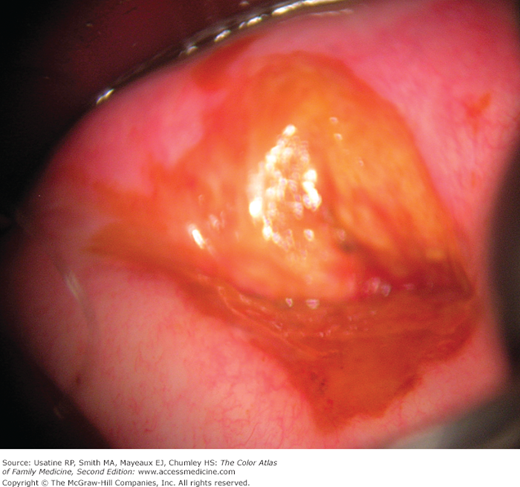
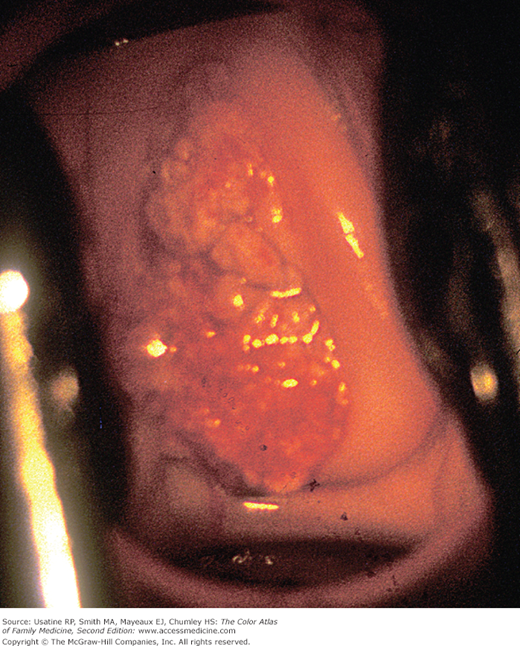
- Ninety-three percent of invasive cervical cancers are SCCs (Figures 91-1, 91-2, 91-3, and 91-4). They almost all contain HPV DNA, and 90% are subtypes 16 or 18, which are most virulent.7
- Approximately 7% of cases are adenocarcinomas but these are on the rise7 (Figure 91-5).
- It is rare to find invasive cancer of the uterine cervix in pregnancy. The incidence varies from 1 to 15 cases per 10,000 pregnancies, and the prognosis is similar to that of nonpregnant patients.8
- The peak prevalence of invasive cervical cancer is 40 to 50 years of age.9
Etiology and Pathophysiology
- Oncogenic HPV serve as initiators, and other factors relating to immune status, such as cigarette smoking, nutrition, or other genital infections, may be promoters.10
- Cervical cancer is unique in that no other human cancer has been shown to have such a clearly identified cause, which are oncogenic strains of HPV.1
Risk Factors
- HPV infection.11
- Nonuse of barrier protection and/or spermicidal gel during sexual intercourse.
- No Pap testing within the last 3 years in low-risk women with a cervix or within 1 year for high-risk women.
- Nonvaccination status for HPV-16 and HPV-18.
- Tobacco smoking.
Diagnosis
- Leukoplakia is typically an elevated, white plaque seen prior to the application of acetic acid. It is caused by a thick keratin layer that obscures the underlying epithelium (Figure 91-1). It always warrants a biopsy.
- Early invasion often is associated with a decline in the acetowhite reaction. Yellow hued color change is also a marker for early or frank invasive lesions (Figure 91-4

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree