Clostridium Difficile
Laura W. Lamps, MD
Key Facts
Terminology
Infection by Clostridium difficile, most common nosocomial GI infection
Causes colitis, most often pseudomembranous colitis
Etiology/Pathogenesis
Usually associated with recent antibiotic use, most commonly oral antibiotics
Elderly, debilitated, hospitalized patients also at increased risk
Clinical Issues
Typical symptoms
Diarrhea, initially watery but variably bloody
Fever
Leukocytosis
Abdominal pain
Recurrence common despite successful therapy
Patients with fulminant disease may have signs of acute abdomen but lack diarrhea
Incidence of severe or life-threatening infection is increasing
Macroscopic Features
Yellow-white exudates or pseudomembranes
Distribution: Entire colon or segmental/patchy
Microscopic Pathology
Ballooned or dilated glands
Intercrypt necrosis
Degenerating surface or glandular epithelial cells
Pseudomembranous exudate
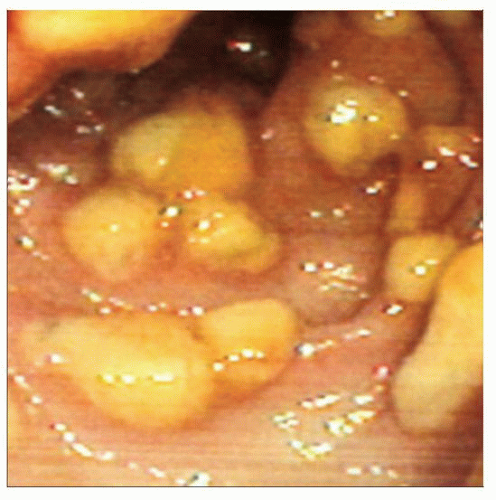 Endoscopic photograph shows characteristic pseudomembranes in a C. difficile infection. (Courtesy W. Webb, MD.) |
TERMINOLOGY
Abbreviations
Clostridium difficile (C. difficile)
Synonyms
Pseudomembranous colitis
Definitions
Infection by Clostridium difficile, potent toxigenic bacteria
Produces 2 toxins: Toxin A and toxin B
Causes colitis, most often pseudomembranous colitis
ETIOLOGY/PATHOGENESIS
Recent Prior Antibiotic Exposure
Usually orally administered antibiotics
Bacteria cannot infect in presence of normal gut flora
Most common nosocomial GI pathogen
Other Risk Factors
Elderly patients
Severe comorbid illness/admission to ICU
Inflammatory bowel disease
Indwelling nasogastric tubes
GI procedures
Antacids
Long hospitalization
CLINICAL ISSUES
Presentation
Diarrhea
Ranging from mild to severe
Initially watery
Variably bloody
Fever
Leukocytosis
Abdominal pain
Symptoms can occur weeks after stopping antibiotics
Complications
Toxic megacolon
Perforation
Reactive polyarthritis
Variant presentations
May be superimposed on IBD
Rare patients are asymptomatic
Patients with fulminant disease may have signs of acute abdomen but lack diarrhea
Treatment
Antibiotics, supportive care
Fulminant cases may require surgery
Prognosis
Recurrence common
Up to 50% of cases recur despite successful therapy
Incidence of severe or life-threatening infection is increasing
Epidemic strain of C. difficile, BI/NAP1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



