(1)
Canberra, ACT, Australia
Summary
Current diagnostic terminology used to describe pulpal and peri-radicular states is presented with an attempt to provide minimum confusion for the practitioner. In order to carry out proper endodontic treatment, a complete diagnosis must include both a pulpal and peri-apical diagnosis for each tooth evaluated.
Clinical Relevance
Modern endodontics is not only interested in treatment modalities of pulpal extirpation procedures aimed at treating diseased pulps. More so, in recent times, the advent of ‘regeneration’ procedures holds the belief that conservative procedures aimed at preserving pulpal vitality or healing of diseased pulps may be possible. Without the correct diagnosis, the correct treatment cannot be prescribed. Clinical terminology in regard to diagnosis is based on assumptions by correlating signs and symptoms and radiographic findings often confusing with presumed histopathological status. The clinician is presented with simple diagnostic terminology based on clinical findings underpinning the progressive nature of pulpal disease, which ensures the most appropriate treatment strategy is selected. Traditional histopathological based diagnostic terminology should be disregarded for this purpose.
3.1 Diagnostic Terms for Pulpal and Peri-radicular Health and Disease States
Many different classification systems have been proposed to describe the various states of pulpal health and disease based on either histopathological findings or clinical findings. The majority of classifications advocated are a combination of the two [1–9]. Even when the ‘gold standard’ of histological findings was correlated with pulpal clinical signs and symptoms, no direct correlation could be made, further proving this fallacy [10–12]. The clinician should be aware that we are only able to indicate the probable pulpal status of any tooth based on both clinical and radiographic findings [13–15]. Often our treatment decisions based on presumed diagnosis are only proven once treatment has been initiated. It is therefore of paramount importance that we correctly diagnose the pulpal status along the continuum of health and disease with as much confidence as possible. A starting point on this road to success is identifying and understanding correct terminology when attempting to address the endodontic health of any given tooth and eliminating terminology related to histopathology that cannot be attained in the clinical situation [16–24] (see Tables 3.1 and 3.2).
Table 3.1
Comprehensive clinical diagnostic system
Clinically normal pulp | Vital, asymptomatic healthy pulp |
Reversible pulpitis Acute Chronic | Presence of mild inflammation where the pulp is capable of healing |
Irreversible pulpitis Acute Chronic | Presence of more degenerative processes within the pulp whereby the pulp is not capable of healing |
Pulp necrosis Necrobiosis (partial necrosis) Complete pulp necrosis Sterile Infected | The end result of irreversible pulpitis. Subsequent bacterial invasion will lead to an infected pulpal necrosis |
Pulpless tooth | Previously initiated treatment (pulpotomy, pulpectomy) |
Degenerative changes Atrophy Pulp canal calcification Partial Complete Hyperplasia Internal resorption Surface Inflammatory Replacement | Pulp atrophy or fibrosis is a degenerative change that is not clinically discernable PCC sometimes referred to as pulp canal obliteration or calcific metamorphosis Pulp polyp Pathological state of the pulp where multinucleate giant cells begin to remove the dentinal walls of the pulp space |
Previous root canal treatment No signs of infection Infected Technical standard Adequate Inadequate Other problems Perforation, missed canals, fractured instrument | Previously treated teeth |
Table 3.2
Comprehensive radiographic diagnostic system
Normal peri-radicular tissues | Teeth with normal peri-radicular tissues that will not be abnormally sensitive to percussion or palpation testing |
Acute apical periodontitis Symptomatic apical periodontitis | Inflammation usually of the apical periodontium producing clinical symptoms including painful response to biting and percussion (mechanical allodynia) |
Acute apical abscess Acute alveolar abscess Dentoalveolar abscess Phoenix abscess | An inflammatory reaction to pulpal infection and necrosis characterised by rapid onset, spontaneous pain, tenderness of the tooth to pressure, pus formation and swelling of the associated tissues |
Chronic apical periodontitis Asymptomatic apical periodontitis | Inflammation and destruction of apical periodontium that is of pulpal origin, appears as a peri-radicular radiolucent area and does not produce clinical symptoms |
Acute exacerbation of chronic apical periodontitis | Inflammation and destruction of apical periodontium that is of pulpal origin, appears as a peri-radicular radiolucent area that produces clinical symptoms |
Chronic apical periodontitis with suppuration | An inflammatory reaction to pulpal infection and necrosis characterised by gradual onset, little or no discomfort and the intermittent discharge of pus through an associated sinus |
Condensing osteitis | A diffuse radiopaque lesion believed to represent a bony reaction to low-grade inflammatory stimulus, usually seen at the apex of a tooth in which there is long-standing pulp pathosis |
3.2 Clinically Normal Pulp
This is equivalent in meaning to a vital, asymptomatic or healthy pulp (Fig. 3.1).
Fig. 3.1
Clinical photographs and radiographic examination used when determining the probable pulp status of a tooth. Following history taking and chief complaint, a thorough examination is performed including (a) percussion, (b) palpation, (c) thermal sensitivity testing and (d) pulp electrical vitality testing. Radiographic examination should include a long cone parallel image of the tooth in question showing the entire tooth and anatomy beyond the root apices. (e) Shows tooth 16 which was determined to be normal after careful examination. Degenerative changes can be seen in the coronal pulp chamber but they do not indicate whether the tooth is healthy or unhealthy
Teeth with a normal pulp and peri-radicular tissues demonstrate no signs or symptoms to suggest any disease is present. Depending on the age of the tooth, there may or may not be evidence of pulp calcification and pulpal fibrosis. The pulp will generally respond to cold or electric stimuli, and the response will not linger for more than a few seconds. Percussion, palpation and bite tests elicit no pain and the radiographic appearance is normal. A suitable control tooth must be selected for comparison, and pulpal testing should include both thermal and electrical testing to determine the most probable pulpal diagnosis.
3.3 Reversible Pulpitis
This refers to a pulp that has mild inflammation due to pulpal irritation that is capable of healing and returning to a clinically normal pulp if appropriate treatment therapy is performed. Reversible pulpitis is a result of caries, trauma, defective or new restorations, mechanical pulp exposures, tooth brush abrasion, cracked tooth syndrome or recent subgingival scaling and curettage. The pain is characterised as mild to severe elicited by stimuli (e.g. thermal, biting, sweet or sour stimuli) (Fig. 3.2 and 3.3).
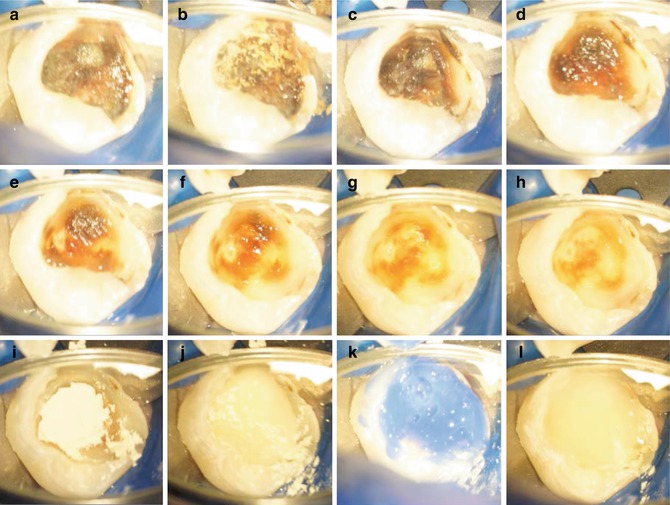
Fig. 3.2
Clinical radiographs demonstrating reversible pulpitis. A 15-year-old patient presented with gross caries in tooth 36 (a). The patient was asymptomatic other than occasional sharp pain with the tooth on eating. Radiographic findings confirmed deep caries overlying the pulp chamber with no obvious peri-apical changes. (b) Final post-operative radiograph demonstrating deep restoration using MTA as an indirect pulp capping agent, glass ionomer cement and composite resin restoration
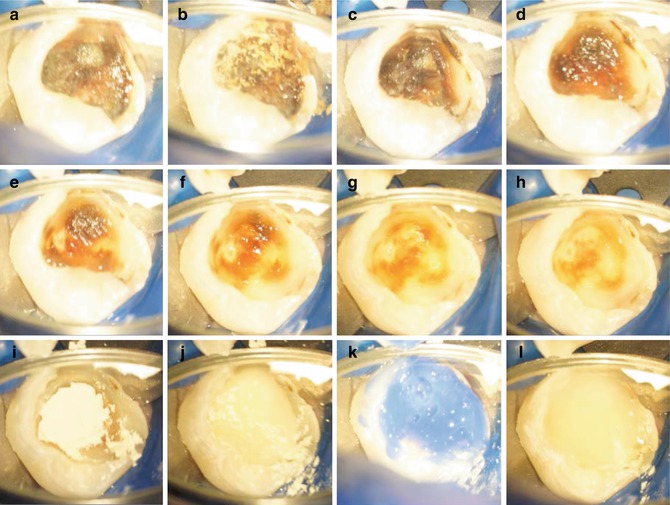
Fig. 3.3
Clinical photographs demonstrating indirect pulp capping procedure using MTA. Note (a–h) caries removal leaving in situ stained dentine overlying pulp, (i) MTA placement, (j) GIC base, (k) acid etching and (l) placement of composite resin restoration
The pain will resolve after a few seconds once the stimulus has been removed and there is no history of spontaneous pain. There will be no response to percussion or palpation, and the radiographic appearance is generally normal. Reversible pulpitis must be distinguished from dentine sensitivity whose aetiology is due to exposed root dentine.
3.4 Irreversible Pulpitis
A pulpal condition is usually caused by deep dental caries or restorations, previous pulp capping procedure, crack or any other pulpal irritant. Spontaneous pain may occur or be precipitated by thermal or other stimuli. The pain may last for several minutes to several hours described as a sharp or dull exaggerated painful response that lingers after the stimulus has been removed. The nature of the pain depends on the type of nerve fibre responding to the inflammation within the pulp (either A delta fibres that mediate sharp pain or C fibres responsible for dull throbbing pain). This disease entity implies that the pulpal state will not heal and if left untreated will result in pulpal necrosis followed by apical periodontitis.
The tooth may or may not be sensitive to percussion and the radiographic appearance may be unremarkable other than the aetiology (deep restoration) (Fig. 3.4).