Classification of Cystic Diseases
Helen Liapis, MD
Joseph Gaut, MD, PhD
PATHOGENETIC CLASSIFICATION
Definition
Renal diseases characterized predominately by cysts
Cyst: Closed cavity in a previously noncystic structure
Cysts may arise in any part of nephron, but most frequently in tubules
Cysts may be found in renal cortex, medulla, or both
Cysts may be diffuse, focal, unilateral, or bilateral
Bilateral cysts are most commonly hereditary
Cysts can be randomly or uniformly distributed (e.g., along corticomedullary junction)
Sometimes ectasia is present rather than a closed cyst
Cysts arising in glomeruli are called glomerular cysts
Term “polycystic” should only be used for autosomal dominant and autosomal recessive polycystic kidney disease (ADPKD, ARPKD)
Location and shape of renal cysts are important for classification
No universally accepted classification scheme
Features considered
Genetic basis
Cystic anatomic structure (tubule, glomerulus, other)
Distribution of cysts (cortex, medulla)
Categories
Hereditary cystic diseases
Autosomal dominant polycystic kidney disease (ADPKD)
Autosomal recessive polycystic kidney disease (ARPKD)
Medullary cystic kidney disease (MCKD)
Nephronophthisis (NPH)
Tuberous sclerosis (TSC)
von Hippel-Lindau (VHL) disease
Primary glomerulocystic kidney disease (GCKD)
Acquired cystic diseases
Secondary GCKD
Acquired cystic disease (end-stage kidney)
Medullary sponge kidney
Multilocular renal cyst
Simple cortical cyst
Non-nephron renal cystic diseases
Pyelocalyceal diverticula
Perinephric pseudocyst
Lymphangiectasis/lymphangiomatosis
EPIDEMIOLOGY
Incidence
ADPKD: 1 in 500 live births
ARPKD: 1 in 20,000 live births
NPH: 1 in 8,000,000 in USA, 1 in 50,000 in Canada
TSC: 1 in 10,000-15,000 live births
ETIOLOGY/PATHOGENESIS
Histogenesis
Cystogenesis: Process involving aberrant formation or maintenance of a normally noncystic structure
Causes of tubular cysts
Epithelial cell proliferation
Apoptosis and defective clearance of apoptotic cells causing tubular obstruction
Scarring of tubule due to inflammation, injury and fibrosis with consequent obstruction
Expansion of luminal contents by vectorial fluid/solute shift
Electrolyte contents reveal distal or proximal tubular transport function
May begin as an ectatic tubule that later becomes a closed cystic space
Causes of glomerular cysts unclear
May involve scarring of outlet
Failure of normal proximal tubule formation
MACROSCOPIC FINDINGS
Differential Diagnostic Features
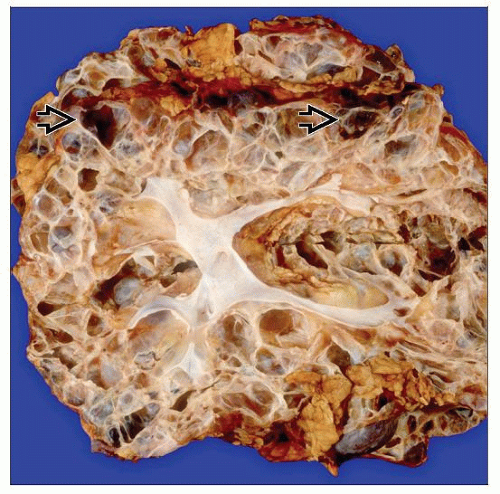
Spherical cysts in bilaterally enlarged kidneys are diagnostic of ADPKD
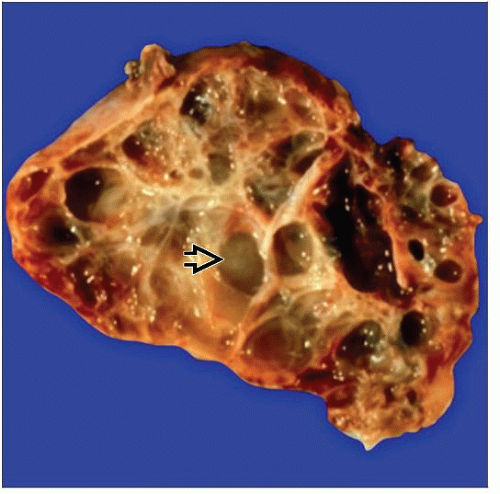
Cylindrical cysts (really ectatic collecting ducts) in enlarged pediatric kidneys are diagnostic of ARPKD
A few small cysts at corticomedullary junction are characteristic of NPH
Isolated cortical cysts, usually unilateral, are nonhereditary, simple cysts seen in elderly patients with no renal disease
MICROSCOPIC FINDINGS
Differential Diagnostic Features
Cysts contain abundant eosinophilic fluid and micropapillary proliferations characteristic of ADPKD
Cylindrical cysts are characteristic of ARPKD
Glomerular cysts affecting > 5% of glomeruli define glomerulocystic kidney disease as being either primary or secondary
Secondary GCKD is more common than primary and presents in children with ADPKD, ARPKD, or TSC
Glomerular cysts are defined as Bowman capsule dilation > 3x normal
Cysts containing renal cell carcinoma are characteristic of hereditary neoplasia syndromes (TSC, von Hippel-Lindau disease) ADPKD, or hemodialysis-induced cysts
Cysts in NPHP/MCDK form are ex vacuo (degenerative); may contain Tamm-Horsfall protein and show tubular basement membrane duplication
Incidental, simple cysts are also degenerative and often lack epithelial lining
HEREDITARY CYSTIC DISEASES
ADPKD
Classic ADPKD in adults
Early onset ADPKD in children