8 The lymph vascular system is a network of drainage vessels for returning excess extravascular fluid, the lymph, to the blood circulatory system and for transporting lymph to the lymph nodes for immunological screening (see Ch. 11). The lymphatic system has no central pump but there is an intrinsic pumping system effected by contractile smooth muscle fibres in the lymph vessel walls, combined with a valve system preventing backflow. The whole circulatory system has a common basic structure: • An inner lining, the tunica intima, comprising a single layer of extremely flattened epithelial cells called endothelial cells supported by a basement membrane and delicate collagenous tissue. • An intermediate predominantly muscular layer, the tunica media. • An outer supporting tissue layer called the tunica adventitia. FIG. 8.1 Heart: left ventricular wall FIG. 8.2 Heart: epicardium (visceral pericardium) FIG. 8.3 Myocardium FIG. 8.4 Endocardium FIG. 8.5 The conducting system of the heart FIG. 8.6 Heart FIG. 8.7 Heart valve FIG. 8.8 Heart valve
Circulatory system
Introduction
The Heart

H&E (LP)
This low-power micrograph shows the three basic layers of the heart wall, in this case the left ventricle.
The tunica intima equivalent of the heart is the endocardium E, normally a thin layer in a ventricle. This is lined by a single layer of flattened endothelial cells, as is the case elsewhere in the circulatory system.
The tunica media equivalent is the myocardium M, made up of cardiac-type muscle (see Ch. 6). In the left ventricle, this layer is very prominent due to its role in pumping oxygenated blood throughout the systemic circulation, but it is less thick in the right ventricle and in the atria which operate at much lower pressures. Note the origins of the papillary muscles PM, extensions of the myocardium which protrude into the left ventricular cavity and provide attachment points of the chordae tendinae which tether the cusps of the atrio-ventricular valves.
The equivalent of the tunica adventitia is the epicardium or visceral pericardium P, usually a thin layer (as here) but, in some areas, containing adipose tissue (see Fig. 8.2a). The coronary arteries run within the epicardial fat.
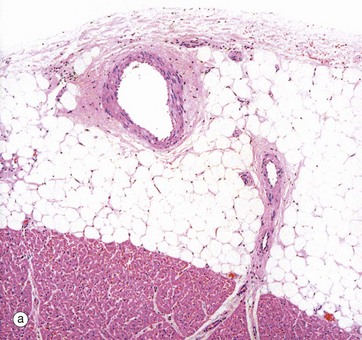
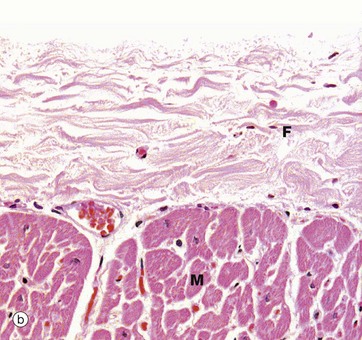
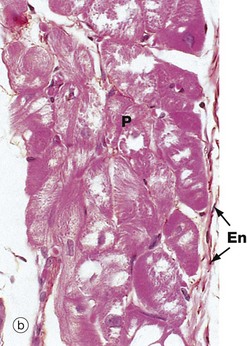
(a) H&E (MP) (b) H&E (HP)
The constant layer of the epicardium is a dense sheet of fibrocollagenous tissue F which also contains elastic fibres. On its outer surface, there is a flat monolayer of mesothelial cells Me (not clearly seen here). These cells are responsible for secretion of lubricating fluid. Micrograph (a) shows an area where the epicardium contains a large branch of the coronary artery CA, with a smaller branch penetrating the myocardium M. Note that in areas containing artery branches, there is a variable layer of adipose tissue A. Micrograph (b) shows the appearance of the epicardium over most of the heart surface, where the fibrocollagenous layer F lies directly on the myocardium M without intervening adipose tissue.
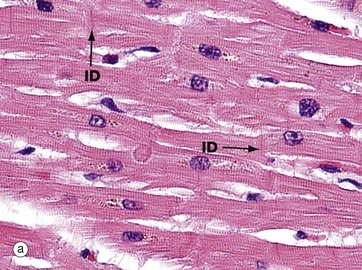
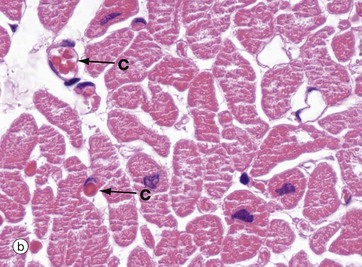
(a) H&E, LS (HP) (b) H&E, TS (HP)
In longitudinal section (a), cardiac muscle fibres form an interconnecting network, joined to each other by intercalated discs ID. These specialised intercellular junctions provide both mechanical and electrophysiological coupling, allowing the cardiac myocytes to act as a functional syncytium. The cells possess central nuclei and regular cytoplasmic cross-striations. The intercalated discs and cross-striations can be clearly seen using special methods such as the immunohistochemical technique for α-B crystallin and in thin resin sections stained with toluidine blue (see Fig. 6.24).
In transverse section in micrograph (b), the extensive and intimate capillary network C between the myocardial fibres is easily seen. The vessels in this section are distended with red blood cells (see also Fig. 6.21). This high level of vascularity is a reflection of the high and constant oxygen demand of the myocardium, particularly in the left ventricle which is shown in these two pictures.
Further structural details of the cardiac muscle of the myocardium are given in Ch. 6.
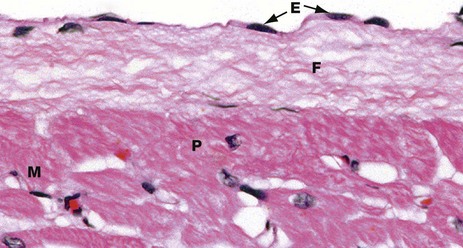
H&E (HP)
The endocardium has a surface layer of flattened endothelial cells E. The endothelium is supported by a layer of fibrous connective tissue F containing variable amounts of elastic tissue. This merges into the collagen fibres surrounding adjacent cardiac muscle cells M, as well as the larger Purkinje fibres P (see Fig. 8.6).
The endocardium shown here is from the wall of the left ventricle. The endocardium of the atria is much thicker than this and includes more elastic fibres.
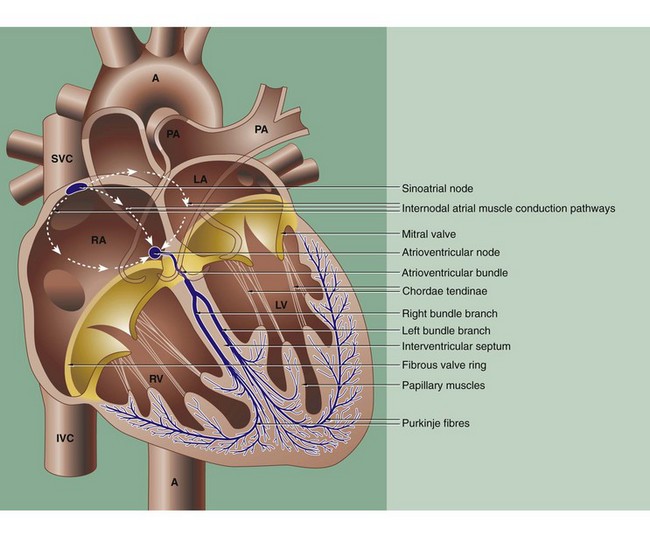
The coordinated contraction of the heart is largely effected by a specialised conducting system of modified cardiac muscle fibres. The initial impulse originates spontaneously in the sino-atrial node, situated in the right atrial wall near the entry of the superior vena cava SVC. The impulse rate is controlled by the autonomic nervous system.
The impulse passes through the muscle of the atria RA and LA, causing them to contract, and reaches the atrioventricular node in the medial wall of the right atrium just above the tricuspid valve ring at the base of the interatrial septum. Both the sinoatrial and atrioventricular nodes are irregular meshworks of very small specialised myocardial fibres, with electrochemical stimuli being transmitted via gap junctions. The nodal fibres are embedded in collagenous fibrous tissue which contains blood vessels and many autonomic nerve fibres.
From the atrioventricular node, the impulse is passed along a specialised bundle of conducting fibres, the atrioventricular bundle (of His), which initially divides into right and left bundle branches that then (halfway down the interventricular septum) become Purkinje fibres which run immediately beneath the endocardium before penetrating the myocardium (see Figs 8.4 and 8.6).
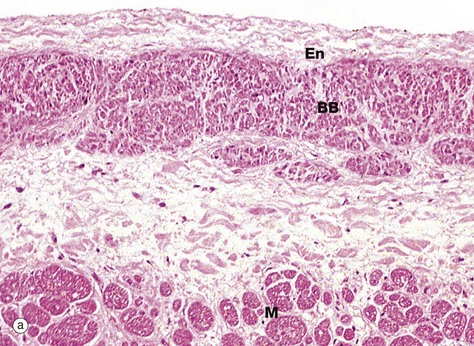
(a) Bundle branch, H&E (MP) (b) Purkinje fibres, H&E (HP)
Micrograph (a) shows the left branch bundle of conducting fibres BB running in the interventricular septum, just beneath the endocardium En lining the left ventricular cavity. At this level, the conducting fibres are separated from the myocardial fibres M of the septum by a layer of fibrous tissue. The conducting fibres are specialised cardiac muscle fibres and contain comparatively few myofibrils, which are mainly located beneath the cell membrane, but abundant glycogen granules and mitochondria. This makes these fibres paler staining than normal myocardial fibres by most stains.
Micrograph (b) shows the distal extension of the branch bundle, with the Purkinje fibres P beneath the thin endocardium En. These fibres are larger than cardiac muscle fibres and have a pale-staining central area with most of the red-staining myofibrils around the periphery of the cell. Unlike myocardial fibres, Purkinje and other conducting fibres have no T tubule system and connect with each other by desmosomes and gap junctions, rather than intercalated discs.
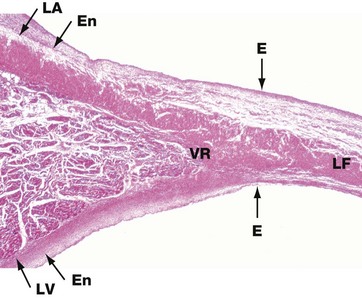
H&E (LP)
The heart valves consist of leaflets of fibroelastic tissue. The surfaces are covered by a thin layer of endothelium E which is continuous with that lining the heart chambers and great vessels. This low-power micrograph shows the left atrioventricular valve (the mitral valve), arising at the junction of the walls of the left atrium LA and left ventricle LV.
The fibroelastic layer of the endocardium En condenses to form the valve ring VR, and from this arises the central fibroelastic sheet of the valve, the lamina fibrosa LF.
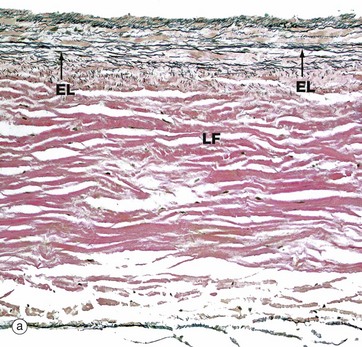
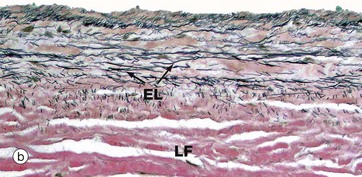
(a) Elastic van Gieson (LP) (b) Elastic van Gieson (MP)
The valves are sheets of fibroelastic tissue covered on both sides by endocardium. There is a dense central plate of collagen (the lamina fibrosa LF) containing scattered elastic fibres (black in this stain) as shown in micrograph (a) at low magnification. In the left atrioventricular valves (as here), there is a distinct elastic lamina (EL) towards the atrial surface in micrograph (b) and the collagen (red staining here) is particularly prominent on the ventricular surface where the chordae tendinae are attached.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
