Churg-Strauss Syndrome
Surya V. Seshan, MD
Key Facts
Terminology
Synonyms: Allergic granulomatosis and angiitis
Etiology/Pathogenesis
Triggers: Allergens, vaccines, drugs
T-helper cell and eosinophil activation
Clinical Issues
Occurs in any age, mostly 40-60 years
Asthma, eosinophilia, granulomatous inflammation
Positive MPO-ANCA (40-70%)
Typically relapsing disease (35-74%)
High renal incidence in ANCA(+) cases
Rapid renal failure, mild renal impairment, hematuria
Remission after initial treatment (90%)
Cyclophosphamide in steroid-resistant or relapsing disease
Microscopic Pathology
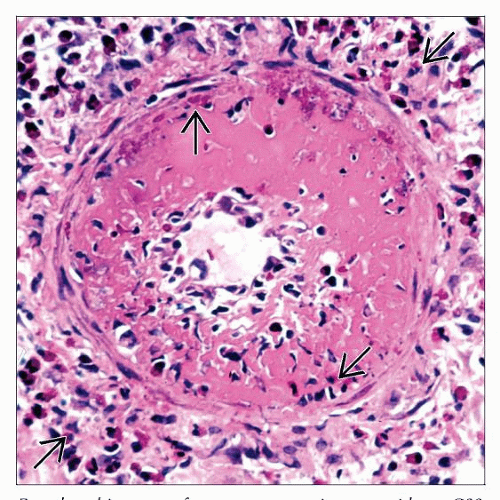
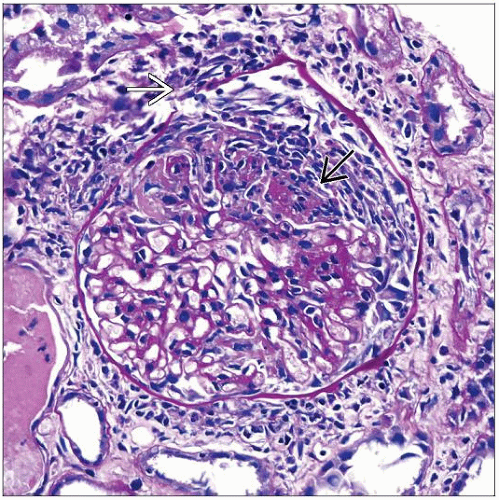
Acute, subacute, &/or chronic crescentic GN, pauci-immune
Occasional isolated eosinophilic interstitial nephritis
Small vessel vasculitis, fibrinoid necrotizing and granulomatous types
Ancillary Tests
Negative IF and nonspecific EM
No immune deposits
Top Differential Diagnoses
Granulomatosis with polyangiitis (Wegener) with renal involvement
Drug-induced vasculitis
Systemic parasitic infestation
TERMINOLOGY
Abbreviations
Churg-Strauss syndrome (CSS)
Synonyms
Allergic granulomatosis and angiitis
Defined by autopsy study in 1951 by Churg and Strauss
Definitions
American College of Rheumatology (ACR) criteria differentiate various forms of vasculitides once diagnosis of vasculitis is made
CSS diagnosis requires 4 of 6 following features
Asthma
Eosinophilia > 10%
Extravascular eosinophil infiltration
Pulmonary infiltrates
Paranasal sinus changes
Peripheral neuropathy
Chapel Hill Consensus Conference (pathology)
Criteria are diagnostic and generally exclude other forms of systemic vasculitides
Eosinophil-rich inflammatory infiltrate and granulomatous inflammation involving respiratory tract
Eosinophil-rich necrotizing vasculitis affecting small to medium-sized vessels
Associated with asthma and peripheral eosinophilia
Classified with antineutrophilic cytoplasmic antibody (ANCA) diseases
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Trigger agents: Allergens, vaccinations, or drugs
Genetic
Associated with HLA-DRB4 gene, risk factor
Pathogenesis
Primarily cell-mediated tissue and vascular injury
CD4(+) T cells secrete interferon-gamma (Th-1 cytokine), promoting granulomatous inflammation
Eosinophil activation via IL-4, IL-5, and IL-13 secretion and CD95-CD95L pathway
Tissue damage by eosinophils due to release of cytotoxic eosinophilic cationic and major basic protein
Eotaxin-3 from endothelial cells chemotactic for eosinophils
ANCA probably contributes to pathogenesis
ANCA titers correlate with disease activity
CLINICAL ISSUES
Epidemiology
Incidence
Rare: 3-11/1,000,000 worldwide
16-27% have renal involvement from 3 large series
Lesser frequency and milder disease than other small vessel vasculitides involving kidney
Age
Peak age: 40-60 years; mean: ˜ 48 years
Younger adults may also be affected
Gender
No gender predilection
Ethnicity
No ethnic predisposition
Presentation
Multisystemic disease
4 phases
Allergic
Constitutional symptoms
Asthma
Rhinitis
Eosinophilic
Vasculitic
Skin purpuric rash
Peripheral neuropathy
Cerebral vessels
Lung
Kidney
Post vasculitic
Sequelae related to major organ damage and hypertension
Renal disease
Higher incidence in ANCA(+) cases
Progressive renal insufficiency
Acute renal failure (less frequent)
Hematuria (mild to severe)
Subnephrotic proteinuria, usually < 1.0 g/d
Asymptomatic (isolated) urinary abnormalities
Obstructive uropathy caused by ureteral stenosis
Laboratory Tests
Anemia, leukocytosis
Peripheral eosinophilia (10-20%)
May be lower or normal in patients previously treated with steroids for asthma
Elevated erythrocyte sedimentation rate
ANCA (40-70% positive)
Mainly p-ANCA (antimyeloperoxidase antibodies [MPO]); rarely c-ANCA or atypical
Rheumatoid factor (25% positive)
Elevated serum IgE levels and immune complexes containing IgE
Treatment
Drugs
Immunosuppressive therapy used to treat severe, multisystemic disease manifestations, particularly vasculitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree