Chronic Myelomonocytic Leukemia
David Czuchlewski, MD
Key Facts
Terminology
Chronic myelomonocytic leukemia (CMML) is a myelodysplastic/myeloproliferative neoplasm
Specific diagnostic criteria for CMML (WHO 2008)
Persistent peripheral blood monocytosis > 1 × 109/L
No Philadelphia chromosome or BCR-ABL1 fusion
No rearrangement of PDGFRA or PDGFRB
< 20% blasts (including blast equivalents) in blood and bone marrow
Dysplasia in 1 or more myeloid lineage
If dysplasia is absent or minimal, CMML may still be diagnosed if clonal cytogenetic or molecular abnormality present or if monocytosis has persisted for at least 3 months and other causes of monocytosis are excluded
CMML may be further subcategorized based on blast percentage
Etiology/Pathogenesis
Cytogenetic abnormalities are detected in up to 40% of cases, but none are specific for CMML
Clinical Issues
Approximately 15-30% of cases progress to AML
Microscopic Pathology
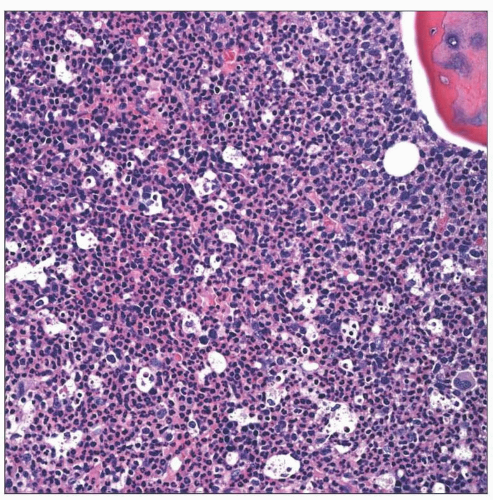
Minority of cases show nodular collections of plasmacytoid dendritic cells
Diagnostic Checklist
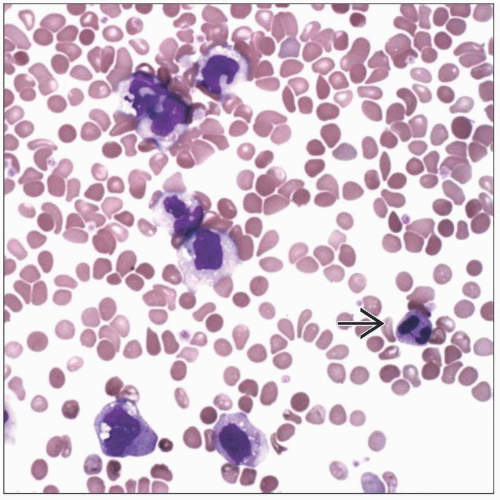
Cytochemical assessment of nonspecific esterase is a rapid and efficient means of documenting monocytic proliferation
TERMINOLOGY
Definitions
Chronic myelomonocytic leukemia (CMML) is a myelodysplastic/myeloproliferative neoplasm
Like other entities in this “overlap” category, it combines features of both myelodysplastic syndrome and myeloproliferative neoplasia
Specific diagnostic criteria for CMML (WHO 2008)
Persistent peripheral blood monocytosis > 1 × 109/L
No Philadelphia chromosome or BCR-ABL1 fusion gene
No rearrangement of PDGFRA or PDGFRB
These should be specifically excluded in cases with eosinophilia
< 20% blasts in blood and bone marrow
Blasts in this case include myeloblasts and blast equivalents (monoblasts and promonocytes)
Dysplasia in 1 or more myeloid lineages
If dysplasia is absent or minimal, CMML may still be diagnosed if clonal cytogenetic or molecular abnormality is present or if monocytosis has persisted for at least 3 months and other causes of monocytosis are excluded
CMML may be further subcategorized based on blast percentage (including equivalents)
CMML-1
< 5% in peripheral blood and < 10% in bone marrow
CMML-2
Between 5-19% in peripheral blood or 10-19% in bone marrow
CMML-2 is also diagnosed when Auer rods are identified, regardless of blast percentage
ETIOLOGY/PATHOGENESIS
Heterogeneity of CMML
Cases range from those with predominant myelodysplastic features to those with more myeloproliferative findings
Given this heterogeneity, it is not surprising that pathognomonic genetic abnormalities have not been identified
Cytogenetic abnormalities are detected in up to 40% of cases, but none are specific for CMML
Common changes include
Trisomy 8
Monosomy 7/del(7q)
Abnormalities of 12p
RAS mutations are identified in up to 40% of cases
Other frequently mutated genes include TET2, CBL, and RUNX1
JAK2 V617F mutations have been reported in some cases, but this change is neither strongly associated with nor characteristic of CMML
CLINICAL ISSUES
Site
In addition to peripheral blood and bone marrow involvement, tissue-based leukemic infiltrates may occur