6
Cholinergic Pharmacology
Chapter 6 Cholinergic Pharmacology is a combination of Chapter 9 Muscarinic Receptor Agonists and Antagonists Chapter 10 Anticholinesterase Agents, and Chapter 11 Agents Acting at the Neuromuscular Junction and Autonomic Ganglia in Goodman and Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. An understanding of the material in these chapters will be helpful in following the material presented in this chapter. In addition to the material presented here the above chapters in the 12th Edition include:
• A complete discussion of the properties and subtypes of muscarinic receptors
• The pharmacological effects of acetylcholine (ACh)
• A detailed discussion of the pharmacological effects of atropine, a muscarinic receptor antagonist
• A discussion of the toxicology of drugs with antimuscarinic properties
• A review of the structure of acetylcholinesterase (AChE)
• A discussion of the mechanism of AChE
• A description of the nicotinic acetylcholine receptor
• A description of the actions of neuromuscular blocking agents on various organ systems
• A discussion of the pathophysiology and treatment of malignant hyperthermia
• A discussion of ganglionic transmission
• A description of the pharmacological actions of nicotine
LEARNING OBJECTIVES
 Understand cholinergic pharmacology, including the different types and subtypes of cholinergic receptors expressed in the central nervous system (CNS), autonomic nervous system (ANS), and neuromuscular junction.
Understand cholinergic pharmacology, including the different types and subtypes of cholinergic receptors expressed in the central nervous system (CNS), autonomic nervous system (ANS), and neuromuscular junction.
 Know the mechanisms of synthesis, storage, release, and destruction of ACh in the CNS, parasympathetic and sympathetic ganglia, parasympathetic nerve fibers, and the neuromuscular junction.
Know the mechanisms of synthesis, storage, release, and destruction of ACh in the CNS, parasympathetic and sympathetic ganglia, parasympathetic nerve fibers, and the neuromuscular junction.
 Know the uses and toxicities of muscarinic receptor agonists and antagonists.
Know the uses and toxicities of muscarinic receptor agonists and antagonists.
 Know the uses and toxicities of drugs and agents that inhibit AChE.
Know the uses and toxicities of drugs and agents that inhibit AChE.
 Describe the uses and toxicities of drugs that block neuromuscular transmission.
Describe the uses and toxicities of drugs that block neuromuscular transmission.
DRUGS (OR AGENTS) INCLUDED IN THIS CHAPTER
Acetylcholine (MIOCHOL-E)
Aldicarb (TEMIK)—Insecticide
Ambenonium chloride (MYTELASE)
Atracurium (TACRIUM, others)
Atropine
Benztropine mesylate (COGENTIN, others); see Chapter 13
Bethanechol (URECHOLINE)
Carbachol (MIOSTAT, ISOPTOCARBACHOL)
Carbaryl (SEVIN)—Insecticide
Cevimeline (EVOXAC)
Chlorpyrifos (DURSBAN, LORSBAN)—Insecticide
Cisatracurium (NIMBEX)
Cyclopentolate hydrochloride (CYCLOGYL, others)
Dantrolene (DANTRIUM, others)
Darifenacin (ENABLEX)
Diazinon (SPECTRICIDE, others)—Insecticide
Dicyclomine hydrochloride (BENTYL, others)
Donepezil (ARICEPT)
Doxacurium
Edrophonium
Fesoterodine (TOVIAZ)
Flavoxate (Urispas)
Galantamine (REMINYL)
Glycopyrrolate (ROBINUL, others)
Homatropine hydrobromide (ISOPTO HOMATROPRINE)
Ipratropium (ATROVENT, others)
Malathion (CHEMATHION, MALA-SPRAY)—Insecticide
Mecamylamine (INVERSINE)
Methacholine (PROVOCHOLINE)
Methscopolamine bromide (PAMINE)
Mivacurium (Not available in the United States)
Neostigmine bromide (PROSTIGMIN-oral)
Neostigmine methylsulfate (PROSTIGMIN-parenteral)
Nicotine gum or lozenge (NICOTINE POLACRILEX, NICORETTE, COMMIT, THRIVE, others)
Nicotine nasal spray or vapor inhaler (NICOTROL)
Nicotine transdermal patch (HABITROL, others)
Onabotulinum toxin A (BOTOX)
Oxybutynin (DITROPAN, others; OXYTROL-transdermal; GELNIQUE-gel)
Pancuronium
Physostigmine salicylate (ANTILIRIUM)
Pilocarpine (ISOPTO CARPINE)
Pilocarpine hydrochloride (SALAGEN, others)
Pipecuronium
Pralidoxime (2-PAM; PROTOPAM CHLORIDE)
Propoxur (BAYGON)—Insecticide
Pyridostigmine bromide (MESTINON-oral; REGINOL, MESTINON-parenteral)
Rimabotulinum toxin B (MYOBLOC)
Rivastigmine (EXELON)
Rocuronium (ZEMURON, others)
Sarin—Nerve gas
Scopolamine (TRANSDERM SCOP)
Solifenacin (VESICARE)
Soman—Nerve gas
Succinylcholine (ANECTINE, QUELICIN)
Tabun—Nerve gas
Tacrine (COGNEX)
Tiotropium (SPIRIVA)
Tolterodine (DETROL)
Trihexyphenidyl hydrochloride (ARTANE, others); see Chapter 13
Trimethaphan
Tropicamide (MYDRIACYL, others)
Trospium chloride (SANCTURA)
Varenicline (CHANTIX)
Vecuronium (NORCURON, others)
MECHANISM OF ACTION MUSCARINIC AGONISTS AND ANTAGONISTS
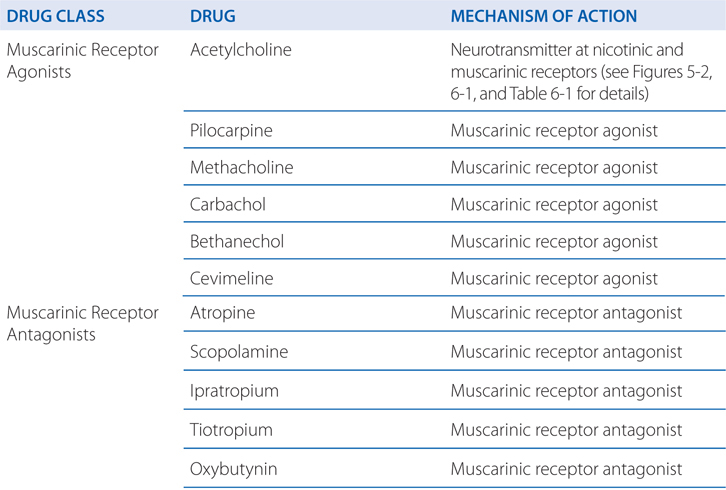
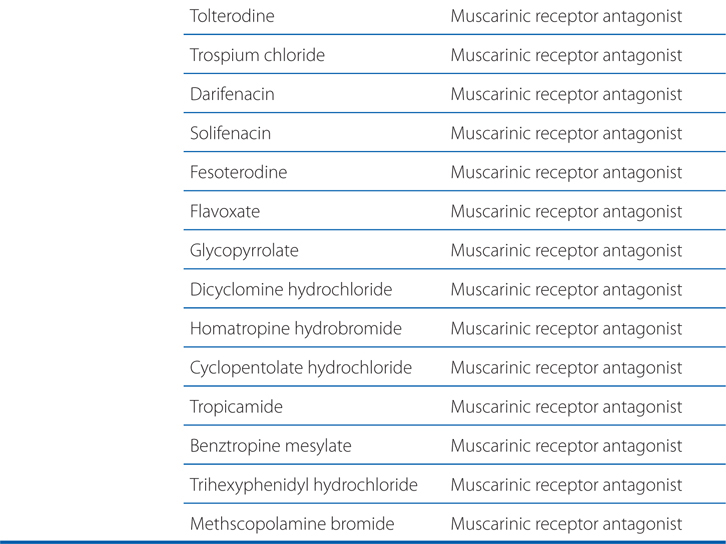
TABLE 6-1 Characteristics of Subtypes of Nicotinic Acetylcholine Receptors (nAChRs)
A 65-year-old man with urinary retention and inadequate emptying of the bladder is being treated with bethanechol.
a. Why is he treated with this drug?
Bethanechol is a muscarinic receptor agonist. Parasympathetic stimulation causes detrusor muscle contraction, increased voiding pressure, and ureteral peristalsis (see Tables 5-1, 6-2, and 6-3). Bethanechol has utility in treating urinary retention and inadequate emptying of the bladder when organic obstruction is absent, as in postoperative retention, diabetic autonomic neuropathy, and certain types of neurogenic bladder.
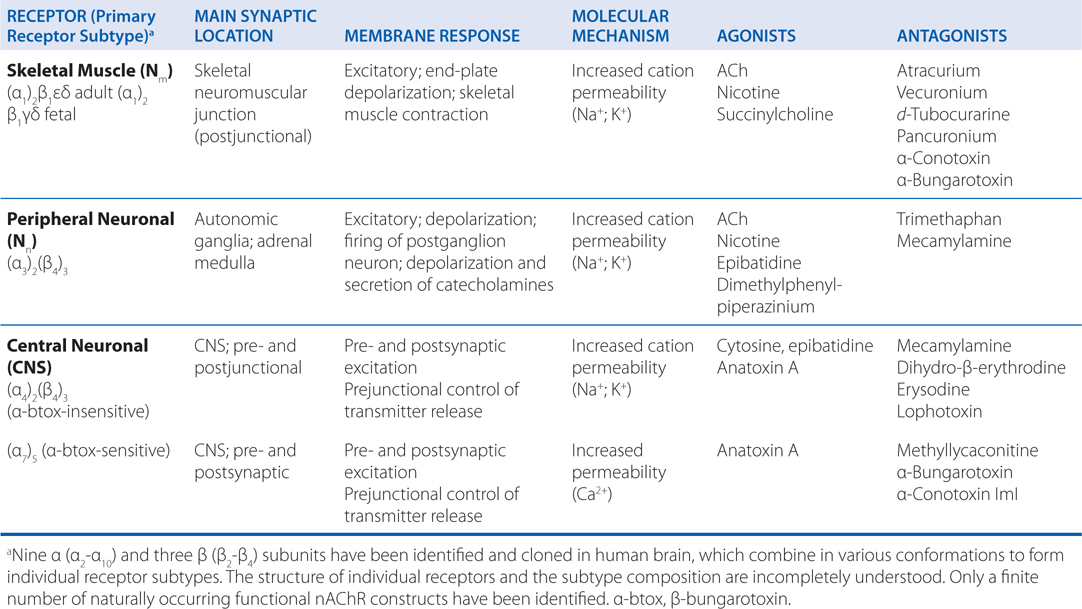
TABLE 6-2 Characteristics of Muscarinic Acetylcholine Receptor Subtypes (mAChRs)
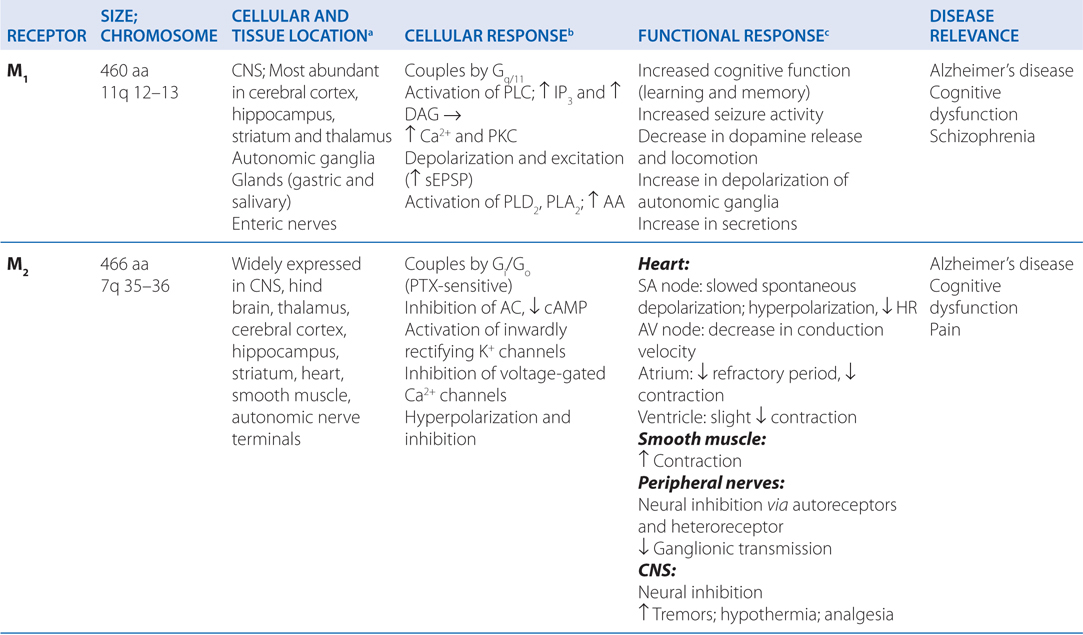
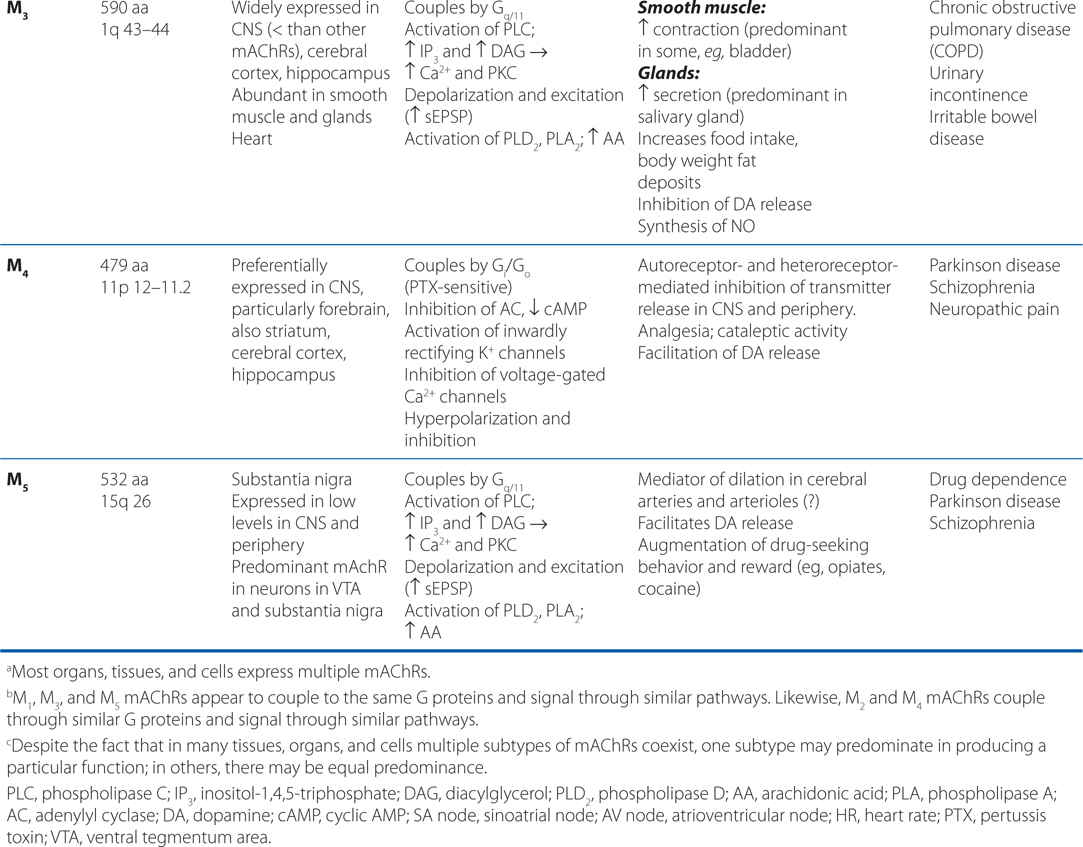
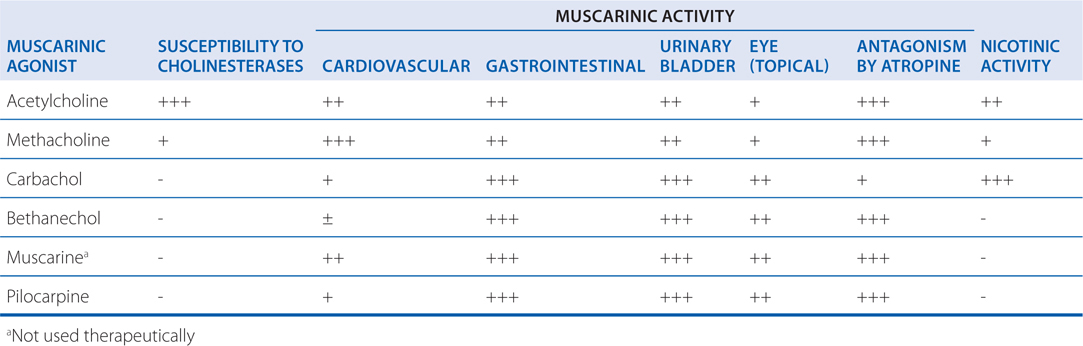
TABLE 6-3 Some Pharmacological Properties of Choline Esters and Natural Alkaloids
b. What side effects should he be aware of while taking bethanechol?
The side effects this patient might experience are a predictable consequence of muscarinic receptor stimulation (see Table 5-1), for example, diaphoresis, diarrhea, abdominal cramps, lacrimation, salivation, bradycardia, and bronchial secretion.
c. What are the contraindications to the use of bethanechol?
The important contraindications to using bethanechol are asthma, chronic obstructive pulmonary disease (COPD), urinary or GI tract obstruction, acid-peptic disease, cardiovascular disease accompanied by bradycardia, hypotension, and hyperthyroidism (muscarinic agonists may precipitate atrial fibrillation in hyperthyroid patients).
A 56-year-old man reports to the emergency room after eating mushrooms that he has foraged. He has brought some of the whole, uncooked mushrooms with him.
a. Although his symptoms now, one hour after ingesting the mushrooms, only include mild abdominal pain and diarrhea, what symptoms should one look for?
It is important to identify the specific mushroom, if possible, to be able to be aware of the possible toxicities. Amanita muscaria mushrooms contain muscarine, a potent muscarinic receptor agonist, and symptoms will be related to stimulation of muscarinic receptors (see Table 5-1). Mushrooms of the Psilocybe or Panaeolus species contain psilocybin which will cause short-lasting hallucinations. Mushrooms of the Amanita phalloides or related species contain amatoxins which can cause hepatic and renal failure, and ultimately death.
b. The mushrooms he has with him have been identified as Amanita muscaria. What is the treatment for this type of mushroom poisoning?
Treatment with atropine effectively blocks the effects of muscarinic receptor stimulation. Large doses may be required. If the patient is showing signs of CNS excitation and hallucinations, these symptoms should be treated with a benzodiazepine (see Chapter 9). Atropine often exacerbates the delirium.
A 48-year-old woman is being treated with oxybutynin for low bladder capacity and urinary frequency.
a. What kind of drug is oxybutynin and why is it effective in this patient?
Oxybutynin is a muscarinic receptor antagonist that is indicated for the treatment of overactive bladder (see Table 6-4). This drug lowers intravesicular pressure, increases bladder capacity, and reduces the frequency of contractions by antagonizing parasympathetic control of the bladder (see Tables 5-1 and 6-3).
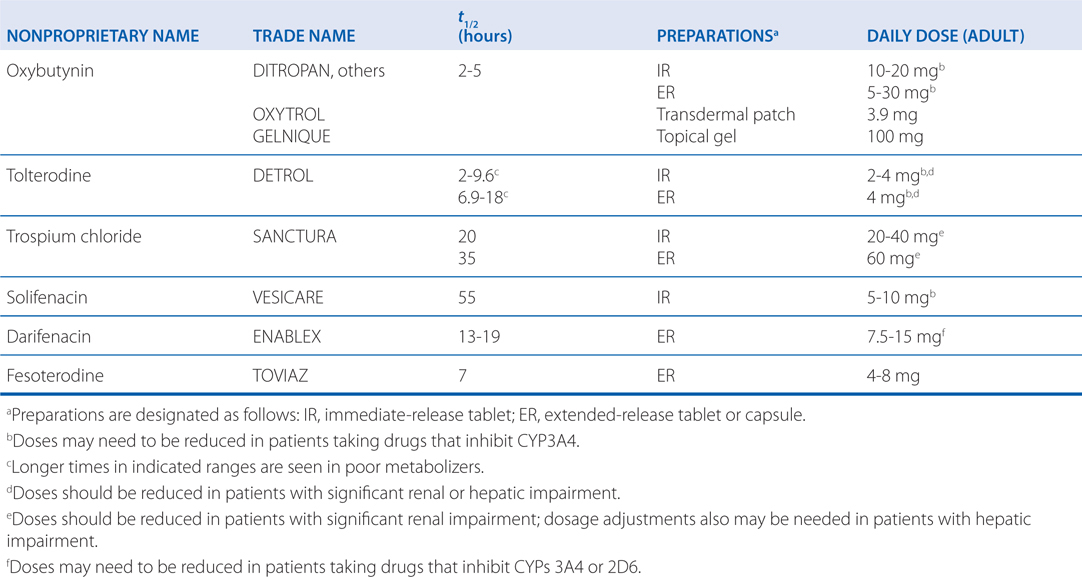
TABLE 6-4 Muscarinic Receptor Antagonists Used in the Treatment of Overactive Urinary Bladder
b. What side effects should she be cautioned about?
The side effects of oxybutynin are a predictable consequence of muscarinic receptor antagonism (see Table 5-1). These effects include xerostomia, blurred vision, constipation, and dyspepsia. CNS-related antimuscarinic effects, including drowsiness, dizziness, and confusion can occur and are particularly problematic in elderly patients. Dry mouth and dry eyes are the most common reasons for discontinuation.
MECHANISMS OF ACTION OF ACETYLCHOLINESTERASE (AChE) INHIBITORS
A 14-year-old boy is brought to the emergency room after drinking a tea made with jimson weed seeds.
a. What is jimson weed and what are the likely symptoms this boy may experience?
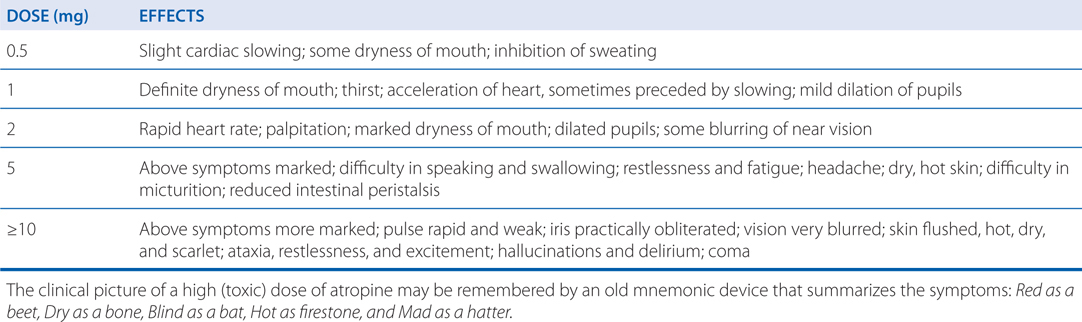
Jimson weed is a common plant that contains atropine and other belladonna alkaloids. The seeds contain high concentrations of these alkaloids and poisoning results from their ingestion. The symptoms of various doses of atropine are shown in Table 6-5 and are predictable as a consequence of muscarinic receptor antagonism.
TABLE 6-5 Effects of Atropine in Relation to Dose
POTENTIAL EFFECTS OF AGENTS THAT INHIBIT AChE
• Stimulation of muscarinic receptor responses at autonomic effector organs
• Stimulation, followed by depression or paralysis, of all autonomic ganglion and skeletal muscle (nicotinic actions)
• Stimulation, with occasional subsequent depression, of cholinergic receptor sites in the CNS
b. If his symptoms are serious and life threatening, what is the appropriate treatment?
Measures to limit absorption of the atropine should be initiated without delay if the poison has been taken orally, as in this case. For symptomatic treatment, slow intravenous injection of physostigmine (an AChE inhibitor) will increase ACh at muscarinic receptors. Physostigmine will rapidly abolish the delirium and coma caused by high doses of atropine, but carries some risk in mild atropine intoxication. Because physostigmine is metabolized rapidly, the patient may again lapse into a coma within 1 to 2 hours and repeated doses may be needed. If marked excitement is present, and more specific treatment is not available, a benzodiazepine (see Chapter 9) is the most appropriate treatment to induce sedation and prevent seizures. Support of respiration and control of hyperthermia may be necessary.
A 23-year-old woman is brought to the emergency room after deliberately ingesting a bottle of organophosphate insecticide.
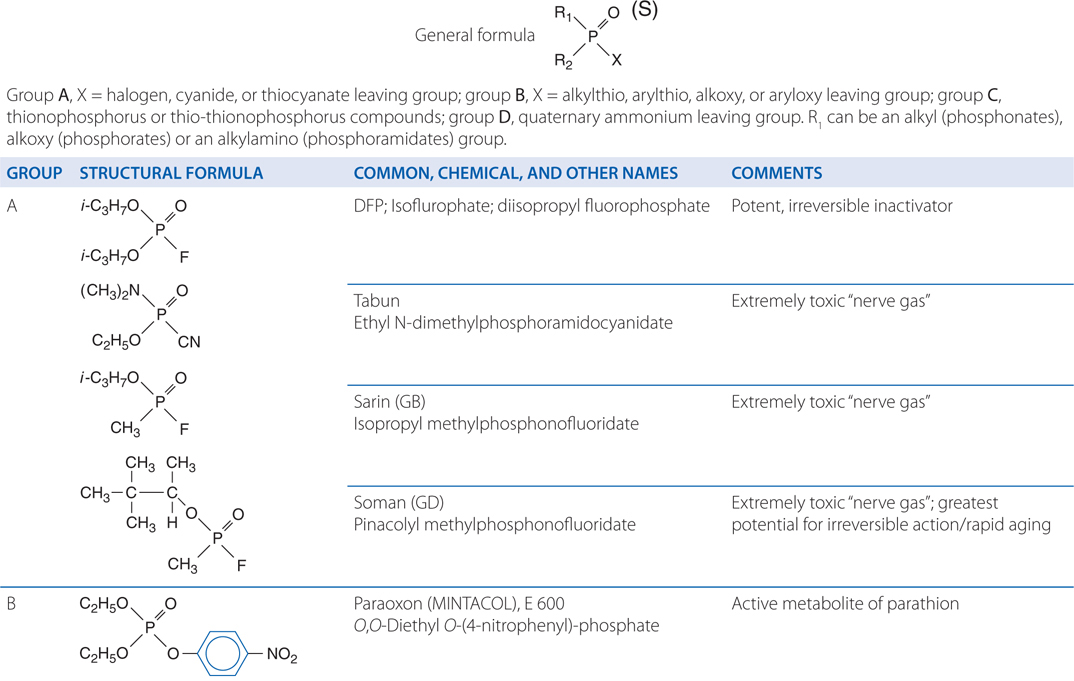
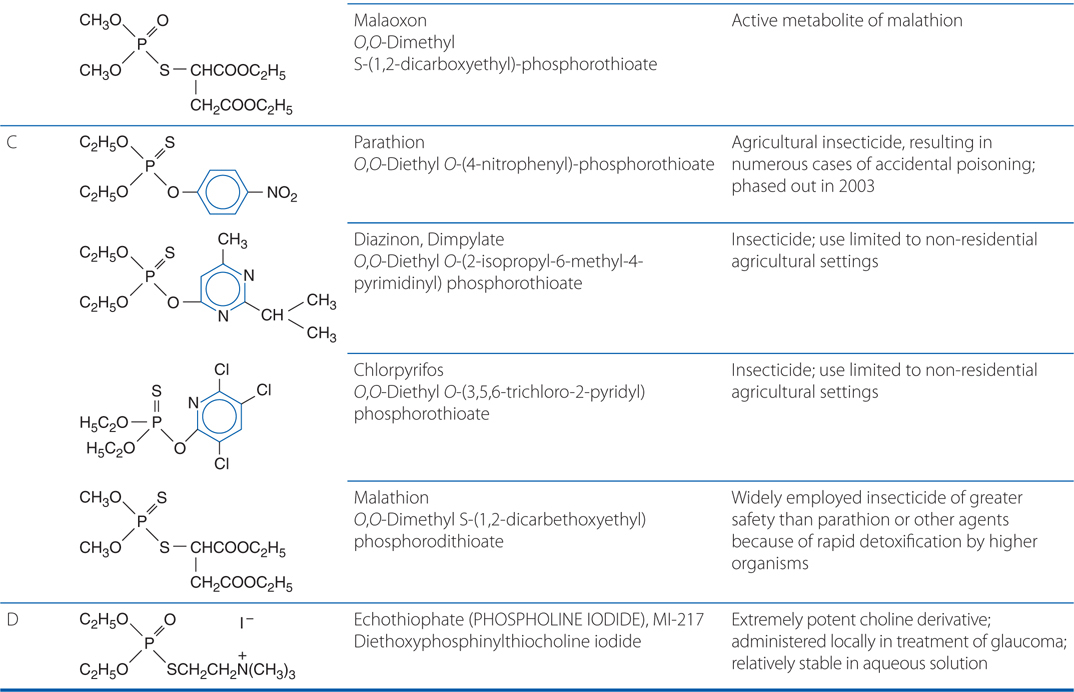
a. Why is it important to identify the specific product this woman ingested?
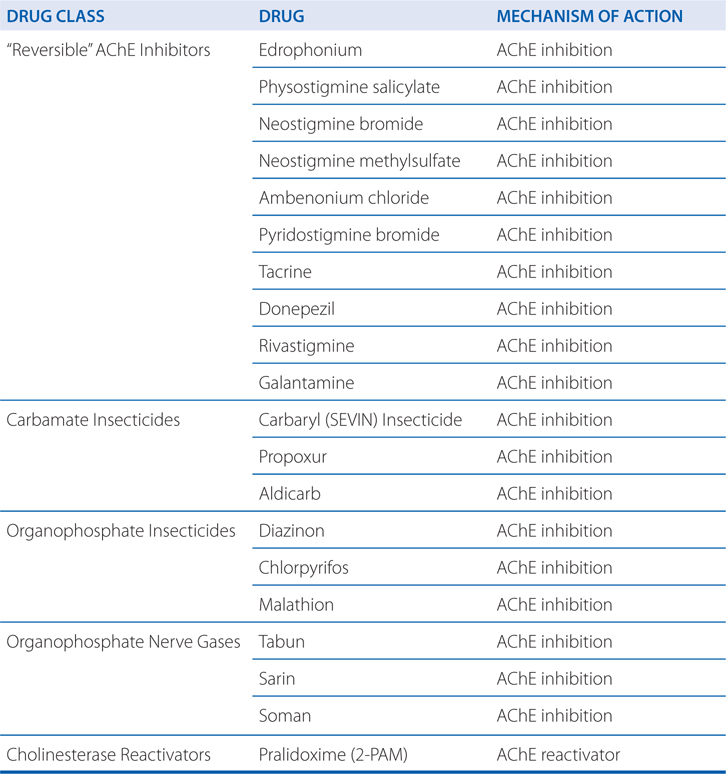
There are two types of insecticides in this class: carbamate insecticides and organophosphate insecticides (see Table 6-6). The carbamate insecticides are “reversible” and inhibit AChE in a fashion identical to other carbamoylating agents (physostigmine and neostigmine), while the organophosphate insecticides inhibit AChE in an irreversible manner by alkylphosphorylation. The organophosphate inhibition of AChE is initially reversible, but “ages” into an enzyme inhibition that is resistant to hydrolysis and reactivation (see Figure 6-2). The symptoms of poisoning from both insecticides resemble each other, but poisoning from an organophosphate insecticide will benefit from the early administration of an AChE reactivator (see below).
TABLE 6-6 Chemical Classification of Representative Organophosphorus Compounds of Particular Pharmacological or Toxicological Interest
b. What symptoms is she likely to experience and what is the timeframe that these symptoms may appear?
The effects of acute intoxication by anticholinesterase (anti-ChE) insecticides are manifested by stimulation of muscarinic and nicotinic receptors (see Table 5-1). In addition, there may be CNS effects except with those agents that have low lipid solubility that cannot cross the blood-brain barrier. The symptoms of poisoning with AChE inhibitors are highlighted in the Side Bar SYMPTOMS OF ACUTE ORGANOPHOSPHATE POISONING.
After the inhalation of vapors or aerosols, systemic effects may occur within minutes, whereas the systemic effects are delayed after GI or percutaneous absorption. The duration of toxic symptoms is determined largely by the properties of the compound: its lipid solubility, whether it must be activated to form the oxon, the stability of the organophosphate-AChE bond, and whether “aging” of the phosphorylated enzyme has occurred. Delayed symptoms appearing after 1 to 4 days and marked by persistent low blood ChE and severe muscle weakness are termed the “intermediate syndrome.”
c. What is the appropriate treatment for this ingestion?
Atropine in sufficient dosage (large doses may be required) effectively antagonizes the effects at muscarinic receptor sites. Atropine is virtually without effect against the peripheral neuromuscular junction (nicotinic) effects.
The nicotinic effects of acute organophosphate poisoning can be reversed by pralidoxime (2-PAM), a cholinesterase reactivator. The mechanism of action of pralidoxime is shown in Figure 6-2. The reactivation of AChE is most pronounced at the skeletal neuromuscular junction. Because pralidoxime has weak anti-ChE activity, it is not recommended for the treatment of overdosage with physostigmine or neostigmine or poisoning with the carbamoylating insecticides such as carbaryl.
SYMPTOMS OF ACUTE ORGANOPHOSPHATE POISONING
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


