Chest Pain
LEARNING OBJECTIVES
In 2006, chest pain and symptoms related to myocardial ischemia were responsible for almost 10% of the 120 million visits to emergency rooms. In the U.S. chest pain and the diseases associated with chest pain are commonly dealt with by pharmacists in almost all practice settings. Approximately, 15 million prescriptions for statins are filled by pharmacists every month, not to mention the larger number of prescriptions for other drugs used to treat angina and causative diseases. National guidelines recommend that most patients discharged after myocardial infarction be placed on as many as four to five medications in addition to their pre-hospital medication regimen. At every visit, pharmacists involved in the management of patients with diabetes, dyslipidemia, and essential hypertension screen patients for symptoms of angina pectoris as a complication of those diseases. Similarly, pharmacists involved in anticoagulation clinics screen for symptoms of pulmonary embolism, a complication of deep vein thrombosis. Therefore, it is important for the pharmacist to understand the various causes of chest pain.
• ETIOLOGY
Not all chest pain is cardiac in nature. In addition to angina, pulmonary embolism, pleurisy, pericarditis, esophagitis, various musculoskeletal causes, and hyperventilation may present with symptoms of chest pain. The most common serious cause of chest pain is atherosclerotic heart disease or coronary artery disease. The specific pathological process of how cholesterol-laden plaques build up in the coronary arteries and eventually cause a myocardial infarction is discussed in more detail in the Chapter 19 on dyslipidemia. Atherosclerotic strokes are discussed in the Chapter 13 on headaches. The most common initial symptom of coronary artery disease is angina pectoris. However, the disease can also present either as a ventricular dysrhythmia that causes sudden death or as a myocardial infarction. Plaque buildup begins as young adults slowly increase the occlusion of the coronary arteries. Once a coronary artery reaches 75% occlusion, patients may begin to have symptoms of angina at times of increased myocardial oxygen demand due to exercise, strong emotions, and cold temperatures. Local tissue hypoxia in cardiac muscle creates the classical cardiac pain seen in angina. Occlusions above 90% may lead to chronic hypoxia and symptoms even at rest. Patients with significant plaque deposition are at risk for a myocardial infarction. As part of the process of plaque deposition and eventual occlusion of the artery lumen, an inflammatory process is created between the plaques and the intima of the artery. For unclear reasons, that inflammation eventually causes the plaque to rupture, exposing the intimal wall to platelets, which begin adhering to the rupture area and quickly aggregating to form a clot. Clot formation may result in 100% occlusion. This lack of oxygen causes the cardiac muscle distal to the clot to die, leading to a myocardial infarction and its complications.
• DIAGNOSIS
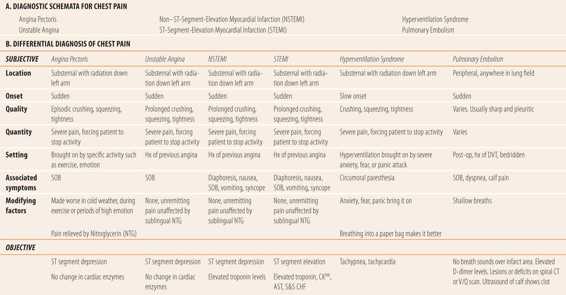
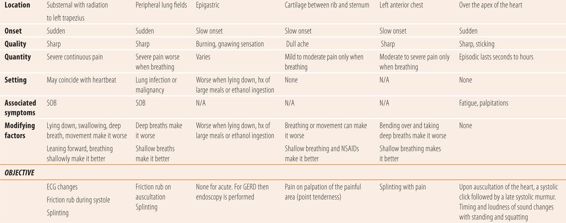
Diagnosis of the exact cause of chest pain requires a careful history of the nature of the pain, circumstances surrounding its onset, physical examination, as well as multiple diagnostic examinations, such as electrocardiogram (ECG) or spiral computerized tomography (Table 9.1). In addition, a variety of blood tests, such as troponin I and D-dimer, may be used to discover the likely cause.
| TABLE 9.1 | Chest Pain |
• CORONARY ARTERY DISEASE
Coronary artery disease (CAD) consists of a sequence of symptoms usually indicating progressively worsening atherosclerosis and narrowing of the coronary artery. Angina pectoris (the chest pain of CAD) has the smallest amount of obstruction of the coronary lumen. The presence of angina means that the patient is at serious risk of atherosclerotic plaque rupturing and causing a clot and more complete lumen occlusion as occurs in a myocardial infarction. Myocardial infarction, which can lead to fatal complications, such as dysrhythmias, congestive heart failure (CHF), and cardiogenic shock, is one of the leading causes of death worldwide. Chest pain of CAD is classically described as a crushing, squeezing, or tightness, “like there is an elephant on my chest,” and is usually located beneath the sternum (substernal). Pain may radiate to the left arm, jaw, shoulder, and back. Angina may be confused with indigestion, or other causes such as panic disorders especially in women, who are more likely than men to have other sensations/symptoms, e.g., burning or stinging sensations. Also, women may perceive other symptoms, e.g., heart flutter, SOB, and lightheadedness as anxiety, whereas men usually perceive them as chest pain.
Angina Pectoris (Ischemic Heart Disease)
Pain occurs when cardiac muscle oxygen demand exceeds its supply. The fixed decrease in the lumen of the coronary arteries prevents on-demand increases in the supply of oxygen. This is the definition of ischemia. There are three primary causes of angina. First, myocardial oxygen demand increases with increased cardiac workload. Things that increase workload and cause the pain of angina include hypertension (pumping against high peripheral resistance), physical activity or exercise, which increases the heart rate, increased intravascular volume (heart is forced to work harder), and CHF. Second, because epinephrine and norepinephrine increase the force and rate of contraction, anything that causes the release or mimics catecholamines will increase myocardial oxygen demand. So emotions such as anger or fear, cold temperatures, hypoglycemic episodes, CHF, and drugs that stimulate the adrenergic branch of the autonomic nervous system such as cocaine, nicotine, decongestants, and sympathomimetic bronchodilators such as albuterol will cause angina. Finally, diseases that create overall hypoxemia such as cigarette smoking, asthma, and COPD can make the patient more susceptible to angina pain.
Angina pain goes away when the cause for increased myocardial oxygen demand is removed or corrected, e.g., stopping physical activity, calming down, or using nitroglycerin to decrease cardiac workload by decreasing venous return to the heart by dilation of peripheral veins in the legs.
In addition to the history suggestive of angina, stress ECGs will show classical ST-segment depression as the affected area of the heart muscle becomes ischemic with increased cardiac workload. Also, CT coronary artery angiography can pinpoint the specific location of the lesion(s). Myocardial perfusion imaging at rest, with technetium or thallium, can also be used to identify ischemic areas.
Acute Coronary Syndrome
Acute coronary syndrome (ACS) is one of three conditions: unstable angina (UA), an immediate harbinger of one of two types of myocardial infarctions; non–ST-segment-elevation myocardial infarction (NSTEMI); and ST-segment-elevation myocardial infarction (STEMI). In all three syndromes, thrombosis of a coronary artery has begun and chest pain continues at rest or lasts 20 to 30 minutes and does not stop when the inciting cause is discontinued or does not stop with the use of sublingual nitroglycerin (NTG). ACS is a medical emergency and if the diagnosis is confirmed for any of the three syndromes, then immediate and intensive interventions are required to prevent serious myocardial damage and death. Diagnosis of ACS depends on clinical presentation, the presence or absence of serum biomarkers, and an abnormal ECG.
While most patients present with classical angina-like chest pain, as many as 20% to 30% of patients present with atypical symptoms and may complain of different kinds of chest pain or no chest pain at all. Women, the elderly, and patients with diabetes more commonly present with atypical symptoms. In patients with risk factors (smoking, hypertension, dyslipidemia, males >55 years of age, family history of CAD, and diabetes), care must be taken not to assume that absence of classical angina like pain eliminates the potential for ACS or angina pectoris.
The three cardiac biomarkers currently used to evaluate ACS are substances that are released into the blood stream when cardiac muscle is damaged. Troponin I and T are regulatory proteins associated with cardiac muscle contraction. Currently, high-sensitivity serum troponin I and T are the most specific and accurate in diagnosis of myocardial infarction. Levels begin to rise 3 to 12 hours after infarction, peaking at 24 hours. Any other type of damage to cardiac muscles, e.g., contusion, myocarditis, or catheter ablation, as well as impaired renal function may also lead to troponin elevations. Myoglobin is a low molecular weight muscle protein found in cardiac and skeletal muscle. Serum levels are detected from 1 to 4 hours after cardiac muscle damage and peak 6 to 7 hours later, making it the earliest marker to be affected. Any kind of muscle injury, trauma, and renal impairment can also elevate myoglobin levels. Finally, the MB fraction of creatine kinase (CKMB), an enzyme involved in the transfer of high-energy phosphate groups is specific for cardiac muscle. The pattern of release is similar to troponin. Because of the kinetics of their release, CKMB and troponin I and T should be reevaluated 6 to 12 hours after the original levels were drawn.
ECG changes are important in distinguishing between the three entities that comprise ACS. In UA and NSTEMI, the findings are typical of ischemic ST depression or T-wave inversion. Because there is little or no scarring, Q waves are formed so the ECG returns to normal within weeks after the insult. STEMI on the other hand shows acute ST-segment elevation, usually followed by a depressed Q wave, which develops hours later and remains as evidence of a past myocardial infarction. Old terminology used to refer to NSTEMI as non–Q-wave myocardial infarction and STEMI as a Q-wave myocardial infarction.
Unstable Angina
Patients with UA usually have a history of stable angina pectoris with a recent history of acceleration in frequency, or persistence of angina, or angina that is induced by less activity than usual. The pain of UA is similar to angina, but it persists or is unresponsive to usual sublingual NTG. ECG findings range from normal to either ST-segment depression or T-wave inversion. Serum troponin I and T, creatine kinase, MB fragment (CKMB), and serum myoglobin levels are normal.
NSTEMI
NSTEMI is a form of heart attack. Patients who tell you they had a “mild” heart attack probably are referring to NSTEMI. Patients with NSTEMI have enough occlusion to cause heart muscle damage, which releases cardiac biomarkers (serum troponin I/T, CKMB, and myoglobin), but not enough damage to permanently alter ECG findings.
STEMI
STEMI is the classical form of myocardial infarction with increased levels of cardiac biomarkers and marked changes in the ECG, primarily ST-segment elevation. Previously known as Q-wave myocardial infarction because the amount of muscle mass damaged by the infarction is enough to create significant scar tissue that causes a negative deflection of the Q wave. They may take several days to develop and are an indicator of a previous myocardial infarction. STEMIs can be regularly accompanied by other symptoms such as nausea, vomiting, diaphoresis, and SOB.
• OTHER CARDIAC CAUSES OF CHEST PAIN
The heart can be the origin of other causes of chest pain.
Pericarditis
Pericarditis is an inflammation of the lining or sac surrounding the heart. It can be caused by a variety of infectious agents, e.g., bacteria, fungi, and viruses, autoimmune disorders, renal failure, and trauma. The pain is generally described as sharp with radiation to the left trapezius area. Swallowing, lying down, and deep breathing make it worse, while shallow breathing and leaning forward make it better. Uremic pericarditis typically presents with little or no pain. Objective findings may include fever if infectious, or evidence of trauma to the chest. Auscultation of the heart may reveal a pericardial friction rub in 60% to 85% of patients, usually associated with systole and the movement of the heart against the inflamed pericardium. Echocardiogram can be used to detect pericardial effusion.
Mitral Valve Prolapse
Seen in 5% of the population with women having twice the incidence of men, mitral valve prolapse (MVP) is asymptomatic in most patients. Abnormal growth of valve tissue causes a portion of the valve to “flop back” into the atrium. Pain associated with MVP is generally described as sharp and sticking, lasting from seconds to hours and located at the apex of the heart. Auscultation of the heart reveals a midsystolic click, followed by a late systolic murmur. Timing of the click, length of murmur, and occasional loudness change from supine to standing or squatting or during a valsalva maneuver, can be diagnostic.
• RESPIRATORY CAUSES OF CHEST PAIN
Pulmonary Embolism
A pulmonary embolism (PE) is an infarct of the lung due to the release of a venous blood clot from the periphery that makes its way into the pulmonary arteriolar system, usually due to a deep vein thrombosis (DVT) in the calf or leg. Infarct size is determined by the size of the pulmonary vessel occluded by the clot. Large infarcts can be fatal. The onset of chest pain is sudden and is described as a sharp pleuritic type pain associated with dyspnea. Patients may also have calf pain and/or swelling.
Objectively, the patient may have both tachypnea and tachycardia depending on the size of the infarct. Palpation of the calf may be painful and a Homan sign is positive in about 25% of patients with thrombophlebitis, an inflammation of the veins that leads to clot formation. Stasis and trauma are the two leading causes of DVT. DVT development is so common that hospitalized patients, patients going to surgery, and those with cancer are either fitted with mechanical devices that increase venous return from the lower extremities or are placed on injectable anticoagulants such as enoxaparin to prevent them.
There are several diagnostic tests that are used for PE and DVT. To detect the presence of a DVT, an ultrasound of the calf is used. Spiral CT scans of the lungs is the test of choice for PE. Also, occasionally, a V/Q scan (lung scan) that identifies perfusion defects through scintilography. Finally, D-dimer levels, a fibrin fragment that stays in the blood stream for several days after a thrombotic event, are elevated. Levels < 500 μg/L can help rule out PE as a cause of chest pain.
Pleurisy
Pleurisy is chest pain associated with inflammation of the pleural lining of the lungs. Bacterial pneumonia, TB, PE, and malignancy are possible causes. Chest pain is described as sharp and is made worse when taking a deep breath (pleuritic pain) and is usually located laterally at the periphery of the lung fields. Sometimes pleurisy with pneumonia may be described as a right upper quadrant abdominal pain. Objective findings on auscultation may include a friction rub over the inflamed area and findings typical of pneumonia (crackles, absence of breath sounds over consolidated areas).
Hyperventilation Syndrome
Patients present with a crushing, squeezing substernal chest pain that may radiate down the left arm. It is caused by fear or panic induced hyperventilation, which blows off too much carbon dioxide, leading to chest tightness or pain. Many patients also present with circumoral paresthesias (numbness and tingling). Breathing into a paper bag relieves the chest pain by increasing carbon dioxide blood levels.
• MUSCULOSKELETAL CAUSES OF CHEST PAIN
Chest pain due to musculoskeletal causes is very common. Any chest pain that can be reproduced by palpation of the location of the pain or by movement of the upper extremities is likely musculoskeletal in origin. So both history and physical examination are important in establishing a musculoskeletal cause.
Trauma/Rib Fracture
Trauma to the chest and ribs is a common cause of chest pain. A careful history for even minor trauma or muscle overuse is important. Do not overlook hard coughing due to a respiratory infection, which can occasionally induce a rib fracture. Physical examination can help rule out trauma-related chest pain. First, observe the thorax for trauma (hematomas, bruises, lacerations, etc.). Next, have the patient point to the location. Palpate that area for tenderness, as well as other areas of the chest. Next, flex each arm horizontally by lifting the elbow and pulling it across the chest. Next, have the patient look up at the ceiling while you pull both arms backward. If a rib fracture is suspected, do the compression test by pushing the sternum toward the spine, while supporting the patients back with the other hand. Replication of the pain by these maneuvers confirms traumatic causes. Thoracic x-ray can demonstrate fractures.
Chest Wall Twinge Syndrome (Precordial Catch)
Patients complain of a sharp pain or “catch” lasting 30 seconds to 3 minutes usually located on the left anterior chest, which is worse with deep breathing and better with shallow breathing. It can be located elsewhere on the chest and some report onset while bending over at the waist. The cause is unknown but is thought to be due to intercostal muscle spasm.
Costochondritis
Costochondritis, an inflammation of the cartilage between the rib end and the sternum, is another common cause of chest pain. Costochondritis presents with a dull pain near the sternum, which can be made worse by respiratory motion and shoulder or arm movement. Palpation over rib cartilage near the sternum, where the patient has indicated the pain’s location replicates the pain.
• GASTROINTESTINAL CAUSES OF CHEST PAIN
Esophagitis, Acute or Chronic (GERD)
Esophagitis is the most common cause of chest pain seen in the emergency room. Patients present with a history of recent overindulgence of food and ethanol or intermittent pain when lying down. While the pain is usually described as “heartburn” (a gnawing, burning-like pain), it can present in other forms. A “GI cocktail” may be given to confirm esophagitis as a cause after ECG and biomarker tests are negative. GI cocktails are usually a combination of liquid antacid and viscous lidocaine occasionally with a liquid anticholinergic. However, the literature indicates the combination is no better than liquid antacid alone.
• KEY REFERENCES
1. Kontos MC, Diercks DB, Kirk JD. Emergency department and office-based evaluation of patients with chest pain. Mayo Clin Proc. 2010;85:284-299.
2. Steurer J, Held, U, Schmid D, et al. Clinical value of diagnostic instruments for ruling out acute coronary syndrome in patients with chest pain: a systematic review. Emerg Med J. 2010;27:896-902.
3. Kosowsky JM. Approach to the ED patient with “low risk” chest pain. Emerg Med Clin North Am. 2011;29:721-727.
4. Fichet DH, Theroux P, Brophy JM, et al. Assessment and management of acute coronary syndromes: a Canadian perspective on current guideline–recommended treatment—Part 1: non-ST-segment elevation ACS. Can J Cardiol. 2011;27:S387-S402.
5. Fichet DH, Theroux P, Brophy JM, et al. Assessment and management of acute coronary syndromes: a Canadian perspective on current guideline–recommended treatment—Part 2: ST-segment elevation myocardial infarction. Can J Cardiol. 2011;27:S402-S412.
6. Amsterdam EA, Kirk JD, Bluemke DA, et al. Testing of low risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122:1756-1776.
7. Yiadom MY. Acute coronary syndrome clinical presentations and diagnostic approaches in the emergency department. Emerg Med Clin North Am. 2011;29:689-697.
8. Arslanian-Engoren C, Engoen M. Physioligical and anatomical bases for sex differences in pain and nausea as presenting symptoms of acute coronary syndromes. Heart Lung. 2010;39:386-393.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



