Chemical Nerve Agents
Daniel C. Keyes
INTRODUCTION
Terrorism has become a reality of life in many parts of the world. News reports frequently remind us of those individuals and groups who are intent on injuring and killing noncombatants in the name of a cause, for personal satisfaction, or for power. The March 1995 sarin nerve agent attack on the Tokyo subway system resulted in a heightened level of concern in the United States for such an attack on domestic soil. Since the attacks on the World Trade Center in 1993 and September 2001, the United States has entered into a new era of awareness of the terrorism threat.
Although there are a variety of potential weapons for terrorism, only a few are currently thought to be likely for use in a nonmilitary setting. Dr. Alexei Yablokov, an expert on nuclear security and former science advisor to President Boris Yeltsin, testified before the National Security House Subcommittee in 1997 about the existence of “nuclear suitcase bombs” in the former Soviet Union and the lack of knowledge of their current location (1). Each suitcase is attributed a 1-kiloton nuclear weapon. It is assumed that nuclear weapons might be difficult for a terrorist group to bring into the United States and detonate. Radioactive materials could, however, be incorporated into an explosive device and thus constitute a greater threat.
Chemical and biological agents are considered much more likely to be used and thus are considered to be highly significant threats by the U.S. Federal Bureau of Investigation. Both of these have now been used in a nonmilitary setting with significant consequences. It is now considered a question of when, not if a terrorist using chemical weapons will strike in many countries.
HISTORY OF BIOLOGICAL AND CHEMICAL WARFARE
Nonconventional weapons have been used throughout history. The Greeks used animal corpses to pollute the water wells used by the enemy. In the Middle Ages, invading armies catapulted bodies laden with plague and other diseases against besieged populations (2). The United States, Britain, and France have all used blankets laden with smallpox to infect Native Americans. In World War I, biological and chemical weapons became important tools of the continental armies. At Ypres, Belgium, the Germans instituted the first use of chemical agents in warfare. In April 1915, they released 168 tons of chlorine gas along enemy lines. Five miles of Allied lines were opened, but the Germans did not expect such a result, and they did not take advantage of the success. They later implemented mustard gas also. There were approximately 1 million chemical casualties in World War I, with approximately 5% of those being fatalities.
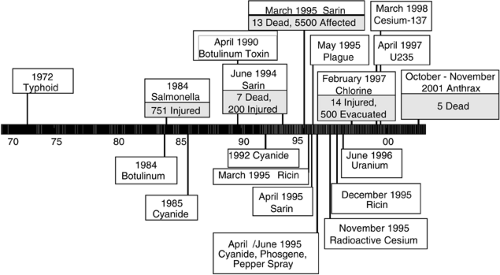
The number of terrorist acts and attempts have been increasing since the 1970s. Many of these have involved the use of explosive devices; however, there have been several notable attempts to use chemical and biological agents (Fig. 1-1). In 1972, a group called the Order of the Rising Sun was found to have 30 to 40 kg of typhoid bacteria cultures with which they intended to attack the water supplies of Chicago, St. Louis, and other cities in the Midwest. In 1984 the Bhagwan cult located in a small town in Oregon, sprayed salmonella onto restaurant salad bars in an attempt to influence local elections. In that event, 45 victims were admitted to area hospitals, and 751 people became ill. No fatalities were reported. These two events were more isolated in nature.
In the early 1980s, a man named Chizuo Matsumoto changed his name to Asahara and established the Aum Association of Mountain Wizards. After a trip to meet the Dalai Lama, he decided to establish a world religion and changed the name of his organization to Aum “Supreme Truth” or Aum Shinrikyo. This organization grew to a membership of 20,000 members and an estimated wealth of $1 billion. The group became increasingly authoritative, requiring absolute submission to its leader, Asahara. The group carried out assassinations of opponents and developed facilities to manufacture nerve agents and biological terrorist weapons.
In June 1994, the group attempted to assassinate three judges in Matsumoto, Japan. The assassination team released sarin nerve agent in the residential community where the judges lived. The attack involved a truck with a special device to release sarin. Although the judges were not killed, seven people died, and 280 were injured.
On March 20, 1995, Aum Shinrikyo launched a chemical attack on the Tokyo subway (3). They put dilute sarin nerve agent into lunch boxes and other containers disguised as lunch bags. The terrorists used umbrellas with sharpened points to puncture the containers during the morning rush hour on three subway lines. This tragic event caused 11 deaths and approximately 5,500 injuries among the commuters and emergency responders (4). The nearest acute care facility, St. Luke’s International Hospital, saw 641 of the victims. Approximately 85% of the victims bypassed the emergency medical system and presented directly to hospitals without decontamination. Fortunately, the weekly grand rounds were taking place at St. Luke’s hospital and a large part of the medical staff was present when patients began arriving (5).
During this event, the identity of the poison involved was not initially known, and there was a delay in reporting this information to the hospitals. Medical personnel contacted the poison center, but this agency had not been informed of the nature of the toxin. Initially, it was assumed that the victims had been exposed to carbon monoxide or possibly cyanide vapor. A physician from Matsumoto correctly noted from news coverage that this was similar to the incident that had occurred in his city several months previously. He contacted colleagues in Tokyo with the identity of the agent within 2 hours of the subway attack (6).
The Tokyo sarin incident demonstrated a concept commonly discussed by disaster response planners. A great majority of victims presented directly to hospitals without the intervention of hazmat or other Emergency Medical Services (EMS) personnel. A typical time for response and set-up for a hazmat incident is 1 hour. This is the time realistically required because of the sequence of activities that must occur: notification, response, hot-zone and perimeter setup, assembly of decontamination stations, and initiation of victim triage. In most cases, ambulatory victims are not willing to wait so long for treatment or transportation to a medical facility. The most realistic option for an individual on the scene would be to obtain private transportation to the nearest emergency room. As a result of this public self-referral to area hospitals, health facilities must be prepared with decontamination facilities, personal protective equipment (PPE), antidotes, and disaster plans to respond to such an incident; they cannot rely on EMS for these actions.
Physicians are key participants in the response to a chemical agent attack. After a terrorist incident, the great majority of patients present to hospitals without the benefit of decontamination or treatment at the scene by emergency medical system personnel. This means that medical personnel and hospitals must plan to be able to respond to such an incident. The agents that are discussed here include tabun, sarin, soman, and VX.
TABLE 1-1 Physical and Chemical Properties of the Nerve Agents | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
HISTORY OF THE NERVE AGENTS
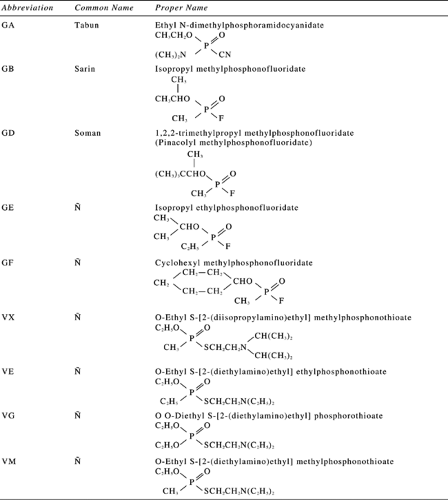
The nerve agents include the German products tabun (GA), sarin (GB), and soman (GD), known as the “volatile agents,” and VX, a “persistent agent.” The biologic and physical properties of these agents and several others are provided in Table 1-1 and Fig. 1-2.
The modern use of nerve agents began in World War II (7). A chemist named Gerhard Schrader was working on the development of organophosphate (OP) insecticides in 1936 when he developed the first nerve agent, tabun. This was followed by SARIN, named for the initials of the scientists involved in its creation (8). The German Ministry of Defense established a large production facility at Dyhernfurth. This facility produced tabun and sarin beginning in 1942 (8). Toward the end of the war, the Soviets captured the Dyhernfurth facility, dismantled it, and moved it to the former Soviet Union where production continued.
THEORETICAL AND SCIENTIFIC BACKGROUND
The nerve agents differ in their potential toxicities (Table 1-1). The LCt50 refers to the dose that kills 50% of unprotected humans expressed as a concentration per cubic meter and with a 1-minute exposure. The first three agents (tabun, sarin, and soman) are considered volatile agents, with characteristics that allow their suspension in air from a properly designed dissemination device. The highly viscous VX has a consistency similar to motor oil.
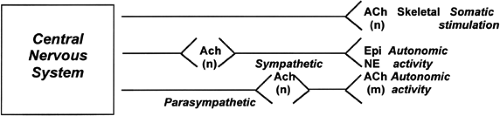
Nerves communicate with each other by secreting chemical neurotransmitters in the synapse (nerve terminal). The neurotransmitter in the cholinergic subset of the autonomic nervous system, and also in autonomic ganglia is acetylcholine (Fig. 1-3). Nerve agents and other organophosphate chemicals inhibit this neurotransmitter and cause an excess of cholinergic symptoms.
The neurotransmitter acetylcholine becomes attached to acetylcholinesterase (AChE) by weak ionic bonds. At the esteratic site, acetylcholine is cleaved into two simple molecules: acetate and choline. This enzyme has a high turnover number (number of substrate molecules that it catalyzes per unit time). Acetate goes into intermediate metabolism, and choline is taken up presynaptically and recycled by combination with acetyl CoA to make more acetylcholine.
Organophosphorus and carbamate compounds are attracted to this esteratic site of AChE, and, as a result of this attraction, acetylcholine cannot enter. This blocks the cleaving of the neurotransmitter and causes acetylcholine accumulation in the synapse. Carbamates attach to both the anionic and esteratic sites. A portion of the carbamate is immediately cleaved off. The enzyme remains inactive during the time in which the carbamate remains carbamoylated to this esteratic site. This hydrolysis step may take 1 hour in the case of the pharmaceutical agent physostigmine, or several hours in the case of pyridostigmine. Carbamate inactivation of AChE is always reversible.
In contrast to the carbamates, most OPs attach only to the esteratic site of AChE. Nerve agents and organophosphorus insecticides combine with the hydroxyl group of a serine residue, leaving an inactive phosphorylated form of the enzyme. Depending on the size of the alkyl group on the OP molecule, hydrolytic cleavage may take a long time to occur, or it may not occur at all. If this bond becomes permanent, the enzyme remains inactivated definitively. When the AChE enzyme has become permanently inactivated, this is referred to as aging of the enzyme. New enzyme must be synthesized for the synapse to function normally once again. In the case of red blood cells, this period of regeneration corresponds to the life of the cell, or 120 days. A series of antidotes, known as oximes, can reverse the inhibition of the AChE enzyme if given before the permanent bond has formed (known as aging). Examples of these oxime antidotes include pralidoxime and obidoxime. They will be discussed in more detail later.
Wherever AChE excess is found, there are symptoms of cholinergic excess. Acetylcholine is the neurotransmitter at the neuromuscular endplate and for the parasympathetic nervous system. It is also the neurotransmitter at the ganglionic level for the sympathetic and parasympathetic nervous systems. As a result, neurotransmitter excess is manifested in the sympathetic and parasympathetic nervous system. Ganglionic, nicotinic cholinergic excess can result in tachycardia, hypertension, and mydriasis, which may be misleading for the clinician who expects to see the classic cholinergic (muscarinic) findings.
CHARACTERISTICS OF SPECIFIC AGENTS
SARIN
A 52-year-old man was exposed to sarin nerve agent and developed the following signs: cyanosis, seizures, labored respirations, miosis, muscle fasciculations, marked salivation, and rhinorrhea. He was treated with atropine (14 mg in 1 day), pralidoxime chloride (2 g in 150 ml normal saline IV) given three times over the first 2 hours, oxygen, assisted ventilation, and nasogastric suction. The patient recovered within several days after a period of emotional lability but died of an acute myocardial infarction 18 months later (9).
Three adults experienced a sudden onset of rhinorrhea and slight respiratory discomfort, miosis, eye pain, increase in salivation, scattered wheezes, and rhonchi. Symptoms were mild and no treatment was given. The AChE levels were depressed, with full recovery occurring in 20 to 90 days (9,10).
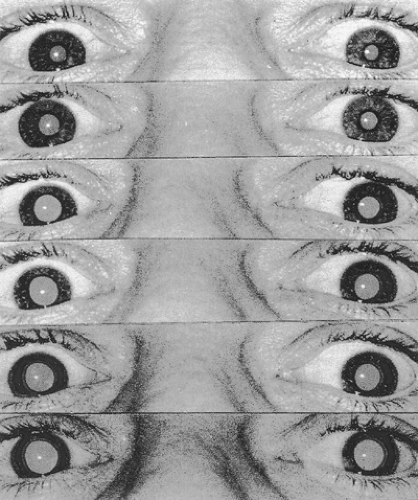
Two adults accidentally exposed to sarin vapor (0.09 mg/m3) exhibited RBC-ChE levels of 19% and 84%, respectively, and developed fixed extremely miotic pupils (11). No other signs or symptoms developed, and neither man required treatment. Recovery to normal cholinesterase activity was gradual over a 90-day period. Pupillary reflexes were not detectable 11 days after exposure. The miotic pupils dilated slowly over a 30- to 45-day period (12). Inhibition of red cell cholinesterase activity appears to be directly related to the dose of sarin. After exposure to sarin at a concentration of 2.73 mg/m3 for 2 minutes, one of two subjects manifested a 23% RBC-ChE inhibition. Contraction of the pupils persisted for 24 hours (13). Workers exposed to sarin three or more times within the previous 6 years developed long-term brain abnormalities reflected in the electroencephalogram (14,15,16).
SOMAN
There are few reported cases of soman poisoning. One such case is reported from over 30 years ago. A 33-year-old male laboratory technician was working with 1 ml of 25% (V/V) soman solution and broke the pipette, splashing a small amount into and around his mouth. “He immediately washed his face and rinsed his mouth with water and was brought to the emergency room … about 5 to 10 minutes after the accident. He complained of impending doom and immediately collapsed. His physical examination revealed him to be comatose with labored respirations and he was slightly cyanotic. He had miosis, which persisted for over 2 months (Fig. 1-4), markedly injected conjunctiva, marked oral and nasal secretions, moderate trismus and nuchal rigidity, prominent muscular fasciculations, and hyperactive deep-tendon reflexes. Except for tachycardia, his heart, lungs, and abdomen were normal” (9).
After a total of 12 mg of atropine as well as pralidoxime, his bronchoconstriction became less severe; however, he could not be intubated because of trismus. He received a tracheostomy and awoke after approximately 30 minutes. His hospital course was described as difficult with persistent fasciculations, nausea, weakness, and restlessness. Although previous publications suggested the possibility of worsening cholinergic symptomatology with the use of phenothiazines, he was given a dose of Phenergan®. He later developed torticollis that responded to diphenhydramine (17,18). A remarkable feature of this case was the requirement of anticholinergic therapy for 5 more weeks (Fig. 1-3). Scopolamine was administered with varying effects during the hospital course. The drug seemed beneficial at the beginning of his medical care but detrimental toward the end (19).
TOXIC DOSE
In experiments conducted some 45 years ago, a sarin dose of 2 mg/kg IV produced no symptoms in human subjects. The red cell cholinesterase (RBC-ChE) was depressed to 28% of control values. No spontaneous recovery was seen. The antidote 2-PAM Cl was administered (2.5 to 25 mg/kg) 1 to 5 hours after sarin exposure, resulting in reactivation of approximately 40% of the RBC-ChE (20,21).
Oral VX administration of 0.004 mg/kg resulted in a few symptoms (diarrhea, transient nausea) within 3 to 4 hours (10). The RBC-ChE was depressed to 70% below normal values in this experiment. Spontaneous recovery occurred in some subjects within 24 to 48 hours. Pralidoxime chloride (5 to 30 mg/kg IV) was administered at 5 to 48 hours after VX. All subjects exhibited reactivation of 70% of the inhibited enzyme. With a VX infusion of 1.5 mg/kg IV, most subjects experienced some lightheadedness and dizziness; some had nausea and vomiting within 1 hour. An increase in heart rate and blood pressure was observed at 3 hours. Erythrocyte cholinesterase was depressed to approximately 20% of normal in subjects with symptoms and to 28% of normal in asymptomatic subjects. Spontaneous recovery of RBC-ChE was observed at 1% per hour over 70 hours. Pralidoxime chloride (2.5 to 25 mg/kg IV) at 0.5 to 24 hours after VX resulted in reactivation of 70% of the inhibited enzyme.
SIGNS, SYMPTOMS, AND LABORATORY: DIAGNOSIS OF AGENT EXPOSURE
The primary diagnosis of exposure to nerve agents is based on the signs and symptoms of victims. The majority of exposed patients present with miosis (small pupils) in the case of the volatile agents. It is interesting that victims of VX exposure usually do not manifest miosis. With any of these agents, the more severely intoxicated patients present with vomiting and seizures. Observation of these effects should provoke the inclusion of nerve agent exposure in the mind of the treating physician. The combination of miosis and muscle fasciculation is considered pathognomonic of organophosphate exposure. If several patients present with the same symptoms, this should cause the physician and hospital staff to consider the possibility of a terrorist attack with these agents. If a chemical attack occurs, one would expect that the majority of victims would arrive within a short period of time (hours) during the same day as the exposure.
The cholinergic symptoms are listed in Table 1-2. It is of special importance to include the important findings of bronchorrhea and bronchoconstriction in one’s effort to remember this toxic syndrome. These are the principal causes of death in organophosphate poisoning. The resolution of pulmonary and bronchial complications constitutes the primary endpoint of treatment. The common mnemonic SLUDGE (salivation, lacrimation, urination, diaphoresis, defecation, GI motility, emesis) leaves out this important endpoint and should not be used for teaching health care providers the characteristics of the cholinergic (muscarinic) toxic syndrome. A better mnemonic for this purpose is DUMBELS (diarrhea, urination, miosis, bronchoconstriction and bronchorrhea, emesis, lacrimation, salivation).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree