Catheter-Based Treatment of Hepatic Neoplasms
Darren W. Postoak
DEFINITION
Catheter-based treatment of hepatic neoplasms is a percutaneous, minimally invasive, image-guided therapy in which the anticancer regimen is delivered to the arterial supply of the tumor. The most common therapies are transarterial chemoembolization (TACE) and radioembolization using yttrium 90 (90Y).
DIFFERENTIAL DIAGNOSIS
Differential diagnosis of the different types of hepatic neoplasms is made by using tissue biopsies, tumor markers, and imaging characteristics. Dynamic computed tomography (CT)/magnetic resonance imaging (MRI) demonstrating intense arterial uptake followed by venous or delayed phase “washout” of contrast is considered to be diagnostic of hepatocellular carcinoma (HCC).1
TACE and radioembolization are usually performed in patients with liver-dominant disease. These tumors may be primary liver malignancies or metastatic disease where the liver is the dominant site of the disease.
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history should be obtained prior to treatment including a past medical history, medications, and allergies. Prior therapy should be evaluated, especially if radioembolization is being considered and the patient has previously had external beam radiation to the liver.
Performance status (ECOG [Eastern Conference Oncology Group] or Karnofsky) must be evaluated. Patients with poor performance status may not be suitable candidates for intraarterial therapy.
Arterial pulse examination is needed for planning of the arterial access site. Typically, the puncture site is the common femoral artery, but this may need to be adjusted if the patient has severe iliofemoral atherosclerotic disease.
IMAGING AND OTHER DIAGNOSTIC STUDIES
All patients should have a preprocedural multiphase CT or MRI examination. A positron emission tomography/CT may be helpful in some instances.
Imaging should be evaluated for tumor number, tumor volume, and portal vein invasion/thrombosis. The vascular anatomy should be evaluated for vascular disease and anatomic variants as this may change the treatment plan.
Laboratory evaluation should include a complete blood count, coagulation profile, creatinine, albumin, and liver function studies.
Exclusionary criteria include immediate life-threatening extrahepatic disease, tumor volume greater than 50% to 70%, uncorrectable flow to the gastrointestinal (GI) tract, and significant hepatopulmonary shunting.
SURGICAL MANAGEMENT
Preoperative Planning
Patients need to be well hydrated, typically with 150 to 300 mL per hour of normal saline prior to and during the procedure.
Preprocedure medications may include antiemetics and steroids.
Antibiotics are administered as needed. This is important in patients without an intact sphincter of Oddi due to sphincterotomy, biliary stent or catheter placement, and surgical biliary-enteric anastomosis. The regimen is 2 weeks in total, beginning 2 days prior to the embolization procedure.2,3
Radioembolization is a multistep procedure with a need for arterial embolization of vessels leading to the GI tract and a simulation of the procedural injection prior to the actual injection of90Y particles. This will be discussed in more depth in the “Techniques” section.
Proton pump inhibitors are started about 2 weeks prior to radioembolization.
Octreotide pretreatment is indicated in patients with metastatic carcinoid to help prevent a carcinoid crisis. Typically, 250 µg is administered intravenously about 1 hour prior to the procedure.
Positioning
The patient is placed supine with both groins prepped and draped (FIG 1). If there are iliac arterial occlusions or other technical problems, then brachial artery access is the next choice with the left arm being preferred. For brachial access, the arm is extended 45 to 90 degrees away from the body.
TECHNIQUES
TRANSARTERIAL CHEMOEMBOLIZATION
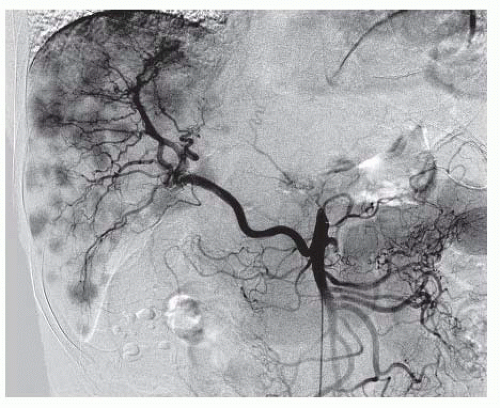
Superior Mesenteric Arteriogram with Venous Phase Imaging
A 4- or 5-Fr catheter is used to selectively catheterize the superior mesenteric artery (SMA). The arterial phase (FIG 2) is inspected for anatomic variants such as a replaced right hepatic artery (FIG 3) or other anatomic variants. The potential for “parasitized” blood flow recruited from the SMA to the liver must also be assessed.
The venous phase (FIG 4) is inspected to evaluate patency of the portal vein and to evaluate for hepatofugal flow. TACE can be performed in cirrhotic patients with hepatofugal portal flow, but a smaller volume of liver should be embolized each time.
Celiac and Common Hepatic Arteriograms
The 4- or 5-Fr catheter is used to selectively catheterize these vessels. The arteriograms (FIG 5) are evaluated for anatomic variants such as a replaced or accessory left hepatic artery arising from a gastrohepatic trunk (FIG 6) and phrenic arteries, which may arise at the origin of the celiac.
If the celiac artery is occluded, the occlusion can often be crossed and possibly stented to allow access or the procedure may be performed from the superior mesenteric artery in a retrograde approach via the pancreaticoduodenal arcade (FIG 7).
Evaluate where the arterial supply to the tumors is arising. Try to limit embolization of branches that do not supply the tumors.
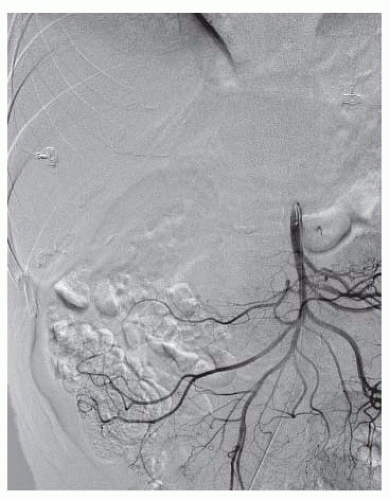 FIG 2 • A superior mesenteric arteriogram is obtained to evaluate for anatomic variants. The patient is positioned to visualize the portal vein during the venous phase of the exam. |
Advancement of the Catheter to Point of Embolization
Commonly, this will be performed using a coaxial microcatheter.
Advance the catheter as selectively as possible; however, a lobar embolization may be required if the tumors are scattered throughout the liver.
In patients with intact gallbladders, evaluate where the cystic artery originates (FIG 8). Ideally, embolization should be performed distal to the cystic artery. Treatment proximal to the cystic artery can cause a chemical cholecystitis with a more severe postembolization syndrome.
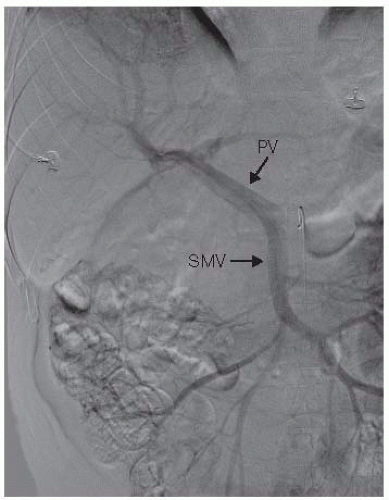
FIG 4 • Venous phase following a superior mesenteric arteriogram demonstrates patency of the superior mesenteric and portal veins (same patient as FIG 2). PV, portal vein; SMV, superior mesenteric vein.
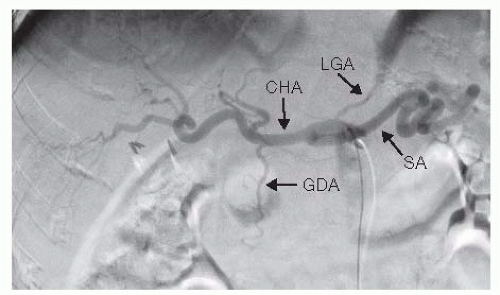
FIG 5 • Celiac arteriogram demonstrating typical celiac and hepatic arterial anatomy. LGA, left gastric artery; SA, splenic artery; GDA, gastroduodenal artery; CHA, common hepatic artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access