Cat Scratch Disease
Irina Margaritescu, MD, DipRCPath
Bruce R. Smoller, MD
Key Facts
Etiology/Pathogenesis
Domestic cats represent natural reservoir and vectors
Cat scratch disease (CSD) is caused by Bartonella henselae (B. henselae), and bacillary angiomatosis (BA) is caused by both B. henselae and Bartonella quintana
Clinical Issues
History of recent exposure to cats (scratch, bite, lick)
Papules or pustules appear at inoculation site in 3-12 days
Regional lymphadenopathy usually occurs after 10-30 days
Immunocompromised patients develop bacillary angiomatosis, bacillary peliosis, or relapsing fever with bacteriemia
Microscopic Pathology
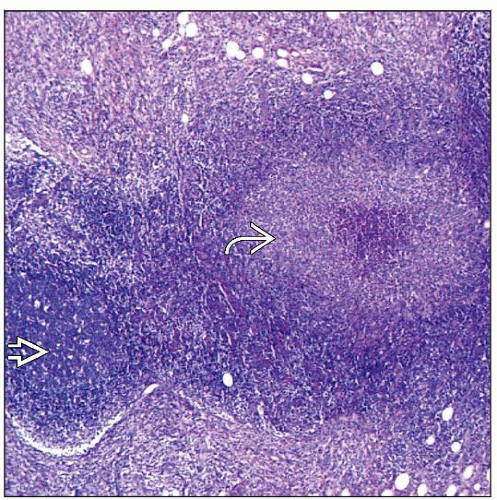
Cutaneous lesions of CSD show zone of necrosis, fibrin, neutrophils, and nuclear debris in dermis surrounded by mantle of macrophages, lymphocytes, and plasma cells
Cutaneous lesions of BA are characterized by vascular proliferation in lobular pattern
Accompanied by lymphocytes, histiocytes, neutrophils, and nuclear dust of neutrophils and clumps of granular purplish material (masses of bacteria) in immediate vicinity of some vessels
Ancillary Tests
Organisms demonstrated by Warthin-Starry stain and immunohistochemistry
TERMINOLOGY
Abbreviations
Cat scratch disease (CSD)
Synonyms
CSD: Cat scratch fever, regional granulomatous lymphadenitis
Bacillary angiomatosis (BA): Epithelioid angiomatosis
Definitions
CSD: Self-limiting infectious disease characterized by subacute, regional lymphadenitis, usually following scratch or bite of cat
BA: Infectious disease that appears in immunocompromised patients following scratch or bite of cat, characterized by vasoproliferative lesions usually, but not exclusively, seen in skin
ETIOLOGY/PATHOGENESIS
Environmental Exposure
Natural reservoir and vectors are domestic cats, especially kittens and stray cats
Occasional cases of CSD associated with dog and monkey bites have been reported
Infectious Agents
Bartonella henselae (formerly Rochalimaea henselae)
Causative agent of CSD, BA, and endocarditis
Small, pleomorphic, intracellular, slow-growing, weakly gram-negative bacillus
Houston-1 and Marseille (genotype II) identified as main genogroups
Bartonella quintana
Causative agent of both trench fever and BA
Less frequently associated with BA than B. henselae
Bartonella clarridgeiae rarely associated with CSD cases
Pathogenesis
Only genus that infects human erythrocytes and triggers pathological angiogenesis in vascular bed
Highly adapted pathogens that infect and persist in erythrocytes and endothelial cells of host circulatory system through various mechanisms
Induction of pathological angiogenesis, with concomitant production of pseudoneoplastic lesions in human vasculature (i.e., BA and bacillary peliosis)
Use of adhesins for endothelial cells
Incorporation of lipopolysaccharides with low endotoxic potency in outer membrane (antagonistic to host’s innate immune response)
Colonization of secondary foci at considerable distances from primary site of infection, with preference for highly vascularized tissues like heart valves, liver and spleen, or cooler areas of body, such as vascular beds of skin
Response to infection depending on immune status of infected host
Granulomatous and suppurative response in immunocompetent individuals
Vasoproliferative response in immunocompromised persons
CLINICAL ISSUES
Epidemiology
Incidence
At least 9.3 per 100,000 population for CSD
Greater in regions with higher temperature and humidity
Incidence peaks in fall and winter months
Age
CSD affects persons in all age groups, but most are < 21 years (60-80%)
BA affects children very rarely
Gender
CSD and BA more common in males
Presentation
History of recent exposure to cats (scratch, bite, lick)
1 or more cutaneous papules or pustules may appear at inoculation site in 3-12 days
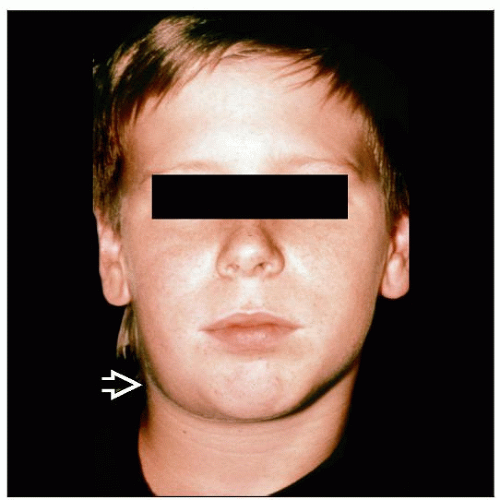
Regional lymphadenopathy (most remarkable manifestation) usually occurs after 10-30 days
Cervical, axillary, or epitrochlear nodes typically involved
Usually mild constitutional symptoms including malaise, anorexia, nausea, fatigue, headache, and low-grade fever
Atypical presentation in up to 10% of cases
Encephalopathy, neuroretinitis, prolonged fever, arthritis, synovitis, atypical pneumonitis, and endocarditis
Granulomatous conjunctivitis and ipsilateral preauricular lymphadenitis (Parinaud oculoglandular syndrome) caused by conjunctival inoculation
Visceral involvement with hepatitis/splenitis
Skin manifestation including nonspecific rashes, erythema nodosum, and leukocytoclastic vasculitis
Immunocompromised patients may develop BA, bacillary peliosis, or persistent or relapsing fever with bacteremia
BA
Vasculoproliferative disease that primarily involves skin but can involve other organs
Numerous brown to violaceous tumors of skin and subcutaneous tissues
Lesions very similar to verruga peruana, the chronic form of Carrión disease (Oroya fever)
Laboratory Tests
Diagnosis of both CSD and BA strongly suggested by history and physical findings
Laboratory findings
Occasionally, mildly elevated white blood cell count, elevated or diminished platelet count, and elevated erythrocyte sedimentation rate in CSD
Anemia, leukopenia, CD4(+) cell count < 200/µL in patients with BA and HIV
Treatment
Options, risks, complications
Most cases of CSD require only supportive and symptomatic care
Management of mild to moderate infections in immunocompetent patients consists of reassurance, adequate follow-up, and analgesics for pain
Antibiotic treatment (azithromycin, erythromycin, doxycycline, or gentamicin) is necessary for severe infections, particularly when lymph nodes are severely affected and when organs other than lymph nodes have become involved
Immunocompromised patients tend to develop more severe Bartonella infections and may require prolonged antibiotic treatment
Avoidance of unnecessary manipulation, including incision and drainage of lymph nodes, is advisable as this may leave scars without hastening recovery
Surgical approaches
Occasionally, lymph node aspiration is indicated for symptomatic relief of tender, fluctuant nodes
Excision of lymph nodes is not justified therapeutically although it may occasionally be indicated for histology
Prognosis
Infections usually resolve without sequelae in 1-6 months in 90% of immunocompetent patients
Immunocompromised patients may develop severe, disseminated disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree