ECOG, Eastern Cooperative Oncology Group.Data from Karnosfsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: Macleod CM, ed. Evaluation of Chemotherapeutic Agents. New York: Columbia University Press; 1949:199–205; Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–655.
DIAGNOSIS
Breast Cancer
- Breast cancer develops in approximately 12% of women during their lifetime in the United States.
- A breast lump in a premenopausal woman is less likely to be cancerous than a breast lump in a postmenopausal woman.
- In a younger woman, a mass should be observed for 1 month to identify any cyclic changes that suggest benign disease.
- If the mass is still present, bilateral mammography should be performed. The accuracy of mammography to diagnose cancer in pre- and postmenopausal women is approximately 90%. Nevertheless, a woman with a clinically suspicious lump and negative mammograms should undergo biopsy.
Cancer of Unknown Primary Site
- Approximately 5% of cancer patients present with symptoms of metastatic disease, but no primary tumor site is identifiable on physical examination, routine laboratory studies, or chest radiography.
- The histopathologic cell type and the site of the metastasis should direct a search for the primary lesion.
- Immunohistochemical stains may identify specific tissue antigens that help define the origin of the tumor and guide subsequent therapy.
- If cervical adenopathy is also present:
- This suggests cancer of the lung, breast, or head and neck, or lymphoma.
- Initial evaluation usually includes panendoscopy (nasendoscopy, laryngopharyngoscopy, bronchoscopy, and esophagoscopy) and biopsy of any suspicious lesion before excision of the lymph node.
- If squamous cell carcinoma is identified, the patient is presumed to have primary head and neck cancer and radiation therapy may be curative.
- This suggests cancer of the lung, breast, or head and neck, or lymphoma.
- If a midline mass in the mediastinum or retroperitoneum is identified:
- In both sexes, this may represent an extragonadal germ cell cancer.
- Elevations in AFP (alpha-fetoprotein) or β-HCG (human chorionic gonadotropin) further suggest this diagnosis.
- This neoplasm is potentially curable.
- In both sexes, this may represent an extragonadal germ cell cancer.
Lymphoma
- Lymphoma is usually diagnosed by biopsy of an enlarged lymph node.
- Staging of Hodgkin disease and non-Hodgkin lymphoma is organized into four categories.
- Stage I is localized to a single lymph node or group.
- Stage II involves more than one lymph node group but confined to one side of the diaphragm.
- Stage III is in the lymph nodes or the spleen and occurs on both sides of the diaphragm.
- Stage IV involves the liver, lung, skin, or bone marrow.
- Stage I is localized to a single lymph node or group.
- B symptoms include fever above 38°C, drenching night sweats, or a 10% weight loss within 6 months prior to diagnosis. These symptoms suggest bulky disease and a worse prognosis.
- Hodgkin disease usually presents with cervical adenopathy and spreads in a predictable manner along lymph node groups.
- Non-Hodgkin lymphoma is classified as low, intermediate, or high grade based on the histologic type.
- Staging evaluation is the same as for Hodgkin disease, but non-Hodgkin lymphoma has a less predictable pattern of spread.
- Advanced-stage disease (stage III or IV) is very common and can usually be diagnosed by computed tomography (CT) scan or bone marrow biopsy; exploratory laparotomy and lymphangiography are rarely necessary.
- Staging evaluation is the same as for Hodgkin disease, but non-Hodgkin lymphoma has a less predictable pattern of spread.
Leukemia
Acute Leukemias
- Patients may present with manifestations of cytopenias, including fatigue and dyspnea (anemia), cutaneous or mucosal hemorrhage (thrombocytopenia), and fever/infection (neutropenia).
- Patients may also present with leukemic infiltration of organs, manifested as lymphadenopathy, splenomegaly (more common in acute lymphocytic leukemia), gingival hyperplasia, and skin nodules (more common in acute myeloid leukemia).
- Leukemic blasts are usually present in the blood.
- Bone marrow aspiration/biopsy is performed to establish the diagnosis and often shows nearly complete replacement by blasts.
- Flow cytometry and cytogenetics must be performed on the bone marrow aspirate for classification and to provide prognostic information.
Chronic Leukemias
- Chronic lymphocytic leukemia (CLL) usually presents with lymphocytosis, lymphadenopathy, and splenomegaly. Malignant cells resemble mature lymphocytes.
- Chronic myelogenous leukemia (CML) presents with leukocytosis and a left shift, as well as splenomegaly.
- Thrombocytosis, basophilia, and eosinophilia are also common.
- The diagnosis of CML is confirmed by demonstration of the Philadelphia chromosome (t9:22), which results in production of a hybrid protein (bcr-abl).
- Thrombocytosis, basophilia, and eosinophilia are also common.
- Hairy cell leukemia represents only 2% to 3% of all adult leukemias.
- Clinical presentation includes splenomegaly, pancytopenia, and infection.
- Patients are at increased risk for bacterial, viral, and fungal infections, and have a unique susceptibility to atypical mycobacterial infections.
- Bone marrow biopsy reveals infiltration by cells that have prominent cytoplasmic projections (thus the name).
- Clinical presentation includes splenomegaly, pancytopenia, and infection.
Multiple Myeloma
- Multiple myeloma (MM) is a malignant plasma cell disorder that is usually accompanied by a serum or urine paraprotein, or both.
- Presenting manifestations may include hypercalcemia, anemia, lytic bone lesions with bone pain, and acute renal failure.
- The initial evaluation should include a radiographic bone survey, bone marrow aspiration and biopsy, serum and urine protein electrophoresis, β2-microglobulin, and quantitative immunoglobulins.
TREATMENT
General Principles of Chemotherapy
- The advice of an oncologist and precise adherence to a treatment plan are mandatory because of the low therapeutic index of chemotherapeutic agents. Specific agents are included in Table 35-2.
- The dosage of chemotherapy is usually based on body surface area. This is determined by body weight and height and should be adjusted when changes in weight occur.
- An assessment of a patient’s disease status, determination of side effects from the previous treatment, and a complete blood count should be obtained before each cycle of chemotherapy.
- Drug dosages often require adjustment for the following conditions: neutropenia, thrombocytopenia, stomatitis, diarrhea, and limited metabolic capacity for the drug.
- Oral drug administration
- May be accompanied by nausea and vomiting and may require antiemetic therapy.
- For some agents, oral absorption is variable and may require special instructions regarding diet and other medications.
- May be accompanied by nausea and vomiting and may require antiemetic therapy.
- IV drug administration
- Should be performed by experienced personnel.
- Care should be taken to ensure free flow of fluid to the vein and adequate blood return should be verified before instillation of chemotherapy.
- Infusions should be through a large-caliber, upper extremity vein. When possible, veins of the antecubital fossa, wrist, dorsum of the hand, and arm ipsilateral to an axillary lymph node dissection should be avoided.
- In patients with poor peripheral venous access or those who require many doses of chemotherapy, indwelling venous catheter devices should be considered.
- Should be performed by experienced personnel.
- Intrathecal chemotherapy
- Intrathecal (IT) chemotherapy is administered for the treatment of meningeal carcinomatosis or central nervous system (CNS) prophylaxis.
- Side effects include acute arachnoiditis, subacute motor dysfunction, and progressive neurologic deterioration (leukoencephalopathy).
- Impaired cognitive function and leukoencephalopathy occur more often when IT chemotherapy is combined with whole-brain radiation.
- Intrathecal (IT) chemotherapy is administered for the treatment of meningeal carcinomatosis or central nervous system (CNS) prophylaxis.
- Intracavitary instillation
- Some chemotherapeutic agents can be instilled directly into the pleural or peritoneal spaces when indicated.
- Systemic toxicities can be observed if the agent is systemically absorbed.
- Some chemotherapeutic agents can be instilled directly into the pleural or peritoneal spaces when indicated.
- Intra-arterial chemotherapy
- Is advocated as a method of achieving high drug concentrations at specific tumor sites.
- Although it is of theoretical advantage, there are no absolute indications for chemotherapy administered by this route.
- Is advocated as a method of achieving high drug concentrations at specific tumor sites.
TABLE 35-2 Chemotherapeutic Medications
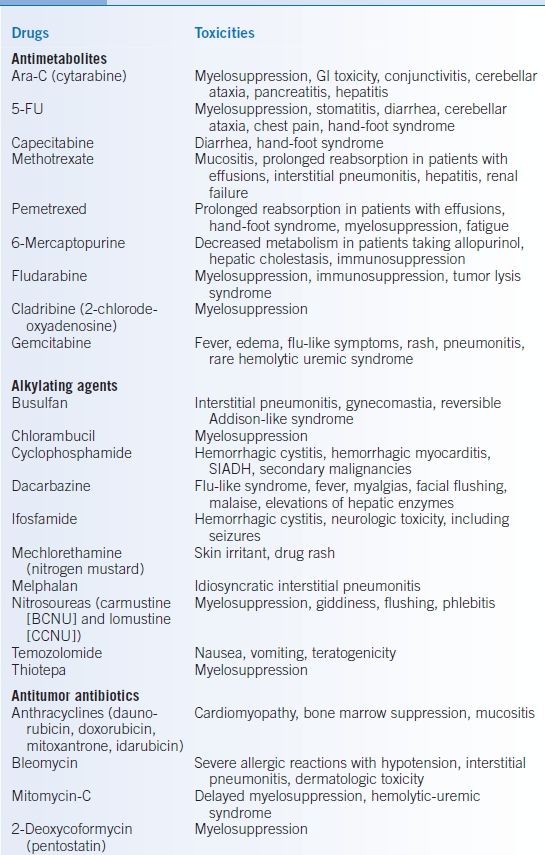
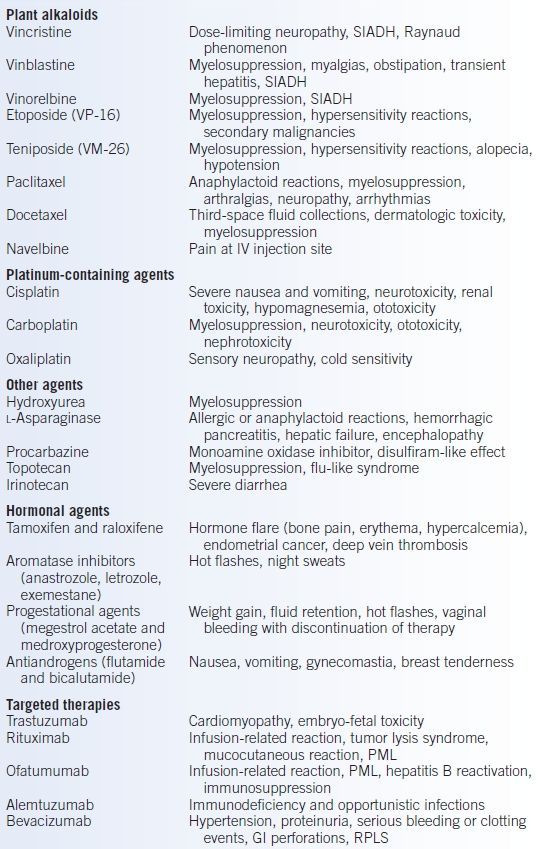
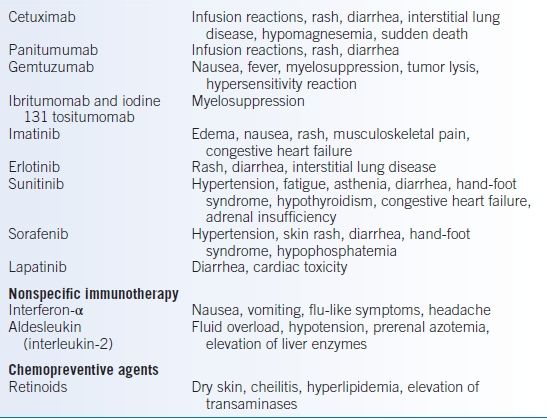
BCNU, bis-chloronitrosourea or carmustine; CCNU, lomustine; GI, gastrointestinal; SIADH, syndrome of inappropriate antidiuretic hormone; PML, progressive multifocal leukoencephalopathy; RPLS, reversible posterior leukoencephalopathy syndrome.
Breast Cancer
Overview
- Surgical options: treatment is focused on local control and reducing the risk of systemic spread.
- Local control with tylectomy (lumpectomy and axillary lymph node dissection) is as effective as a modified radical mastectomy. An axillary lymph node dissection should be included because it provides prognostic information and is of therapeutic value.
- Sentinel lymph node mapping and dissection allow many women to be spared full axillary dissection. In this procedure, blue dye, a radiotracer, or both are injected around the tumor bed. The lymph node(s) that pick up the dye/tracer are excised. If no cancer cells are seen in these lymph nodes, further axillary dissection can be avoided.
- Local control with tylectomy (lumpectomy and axillary lymph node dissection) is as effective as a modified radical mastectomy. An axillary lymph node dissection should be included because it provides prognostic information and is of therapeutic value.
- Radiation therapy is indicated for patients treated with tylectomy and for some individuals with axillary lymph node involvement. It can also be used for palliation of painful or obstructing metastatic lesions.
- Systemic therapy is given for two reasons in the treatment of breast cancer:
- Adjuvant therapy is given to reduce recurrence risk following surgery (see below).
- Palliative therapy is given to women with metastatic breast cancer to slow the progression of disease and to extend their lives (see below).
- Adjuvant therapy is given to reduce recurrence risk following surgery (see below).
- Hormone therapy is used for women with estrogen receptor (ER)-positive and/or progesterone receptor–positive disease.
- Trastuzumab (Herceptin) is appropriate for women with HER2/neu-positive breast cancer.
- Anthracycline-based chemotherapy is potentially useful in all subtypes.
Adjuvant Therapy
- The presence or absence of axillary lymph node metastases is the most important prognostic factor in breast cancer. All women with axillary nodal involvement should receive adjuvant therapy.
- Women with node-negative breast cancer should also be considered for adjuvant therapy if the tumor is >1 cm, is ER negative or has overexpression of HER2.
- Chemotherapy should be considered in patients who are premenopausal, have cancers that are ER negative, or overexpress HER2.
- Tamoxifen, 20 mg PO daily for 5 years, is recommended for all ER-positive breast cancers in premenopausal women.1
- In postmenopausal women, the aromatase inhibitors (anastrozole, letrozole, and exemestane) have generally replaced tamoxifen for adjuvant hormone therapy.
- Trastuzumab has been found to be effective in the adjuvant treatment of women with HER2/neu-positive disease.2
Metastatic Disease
- Menopausal status, hormone receptor status, HER2-neu expression, and sites of metastatic disease dictate initial treatment.
- ER-negative breast cancer, lymphangitic lung disease, and liver metastasis seldom respond to hormonal manipulation and should be treated with chemotherapy.
- ER-positive disease is treated with hormonal manipulation.
- Premenopausal women are initially treated with tamoxifen and a luteinizing hormone–releasing hormone (LHRH) agonist; postmenopausal women should receive a hormonal agent, such as tamoxifen or an aromatase inhibitor. If the disease responds to hormonal therapy, subsequent disease progression may respond to other hormonal agents.
- Chemotherapy should be considered if there is no response to initial hormonal therapy or if progression occurs during subsequent hormonal manipulations.
- Premenopausal women are initially treated with tamoxifen and a luteinizing hormone–releasing hormone (LHRH) agonist; postmenopausal women should receive a hormonal agent, such as tamoxifen or an aromatase inhibitor. If the disease responds to hormonal therapy, subsequent disease progression may respond to other hormonal agents.
- In HER2-overexpressing cancers, the addition of trastuzumab to first-line chemotherapy produced an improvement in survival compared to chemotherapy alone.3
- In women with more than one osteolytic metastasis, the monthly administration of zoledronic acid, 4 mg IV, produces an improvement in quality of life, greater response to therapy, fewer extravertebral fractures, and possibly a prolongation in survival.4 Other bone modifying agents such as denosumab have also been recently approved.
Inflammatory and Unresectable Cancers
- Inflammatory breast cancer manifests as peau d’orange changes or erythema involving more than one-third of the chest wall.
- Because of the high likelihood of metastases at diagnosis, these patients and those with inoperable primary breast cancers are initially treated with chemotherapy.
- Subsequently, surgery and radiation therapies are used for maximal local control.
Lung Cancer
- Lung cancer is the most common cause of cancer death in the United States and is the most preventable given its relationship to cigarette smoking.
- Treatment is based on the histology and stage of the disease.
Small Cell Lung Cancer
- Small cell lung cancer (SCLC) is often responsible for a variety of paraneoplastic syndromes in addition to local symptoms.
- It is treated according to whether disease is limited (confined to one hemithorax and ipsilateral regional lymph nodes) or extensive stage.
- For limited disease, combination chemotherapy and radiation therapy result in a 70% to 90% response rate, a median survival of 14 to 20 months, and a cure in 5% to 15% of patients.
- With extensive disease, the median survival is 9 to 11 months, and cures are rare.
- For limited disease, combination chemotherapy and radiation therapy result in a 70% to 90% response rate, a median survival of 14 to 20 months, and a cure in 5% to 15% of patients.
- For patients who achieve a complete remission with chemotherapy, prophylactic whole-brain radiation therapy has been shown to decrease the risk of central CNS metastases.5
- Radiation therapy to the chest as consolidation therapy may improve survival in limited disease but is not recommended in extensive disease except for palliation of local symptoms.
Non–Small Cell Lung Cancer
- Whenever possible, surgical resection should be attempted for non–small cell lung cancer (NSCLC) because it affords the best chance of cure.
- Survival rates after resection of NSCLC are improved using adjuvant chemotherapy with or without radiation therapy.
- For unresectable disease confined to the lung and regional lymph nodes, radiation therapy in combination with chemotherapy is the conventional treatment.
- In patients with metastatic disease, cisplatin-based combination chemotherapy may modestly improve survival.
- With nonsquamous histology, epidermal growth factor receptor (EGFR) mutation testing and anaplastic lymphoma kinase (ALK) testing should be performed since treatment with erlotinib or crizotinib, respectively, would be recommended in the first-line metastatic setting.
Gastrointestinal Malignancies
Esophageal Cancers
- Esophageal cancers are either squamous cell (associated with cigarette smoking and alcohol use) or adenocarcinoma (arising in Barrett esophagus).
- Surgical resection of the esophagus is recommended in small primary tumors and in selected patients after chemoradiation.
- Local control of unresectable cancers can be achieved with combined chemotherapy and radiation therapy.6
- In metastatic disease, trastuzumab should be added to chemotherapy for HER2-overexpressing esophageal adenocarcinoma in the first- and second-line settings.
- Palliation of obstructive symptoms can be accomplished by radiation therapy, dilation, prosthetic tube placement, or laser therapy.
Gastric Cancer
- Gastric cancer is usually adenocarcinoma and can be cured with surgery in the rare patient with localized disease.
- Adjuvant chemotherapy and concurrent radiation have been shown to improve outcomes in surgically resected gastric cancer.7
- Locally advanced but unresectable cancers may benefit from concomitant chemotherapy and radiation therapy.
- Chemotherapy may offer increased survival and quality of life in patients with metastatic disease. Trastuzumab should be added to chemotherapy in patients with HER2-overexpression.
Colon and Rectal Adenocarcinomas
- These cancers are primarily treated by surgical resection.
- In all patients who are undergoing surgical resection of colon or rectal cancer, a preoperative carcinoembryonic antigen level should be measured and followed. A persistently elevated or increasing level may indicate residual or recurrent tumor.
- A number of chemotherapy agents are available for the treatment of colorectal cancer. These include 5-FU, irinotecan, capecitabine, and oxaliplatin. Adjuvant chemotherapy is offered in stage III patients and in selected high-risk stage II patients.
- Rectal cancer that arises below the peritoneal reflection commonly recurs locally after surgery alone; postoperative radiation therapy and 5-FU are recommended.
- Three monoclonal antibodies have been approved for the treatment of metastatic colon cancer. Bevacizumab targets vascular endothelial growth factor (VEGF). Both cetuximab and panitumumab target EGFR. Also the multikinase inhibitor regorafenib is indicated in metastatic colon cancer.
- Selected patients with metastases confined to the liver may be candidates for liver resection.8
Anal Cancer
- Chemotherapy with concurrent radiation therapy appears to result in a higher cure rate than surgical resection and usually preserves the anal sphincter and fecal continence.9
- Surgical resection should be used only as salvage therapy.
Genitourinary Malignancies
Bladder Cancer
- In the United States, bladder cancer usually presents as transitional cell carcinoma. A variety of chemical carcinogens, including those in cigarette smoke, have been implicated.
- Unifocal tumors confined to the mucosa should be managed with cystoscopy and transurethral resection or fulguration, repeated at approximately 3-month intervals.
- Multifocal mucosal disease is treated with intravesicular bacillus Calmette-Guérin, thiotepa, or mitomycin-C.
- Locally invasive cancers should be resected.
- Adjuvant chemotherapy improves survival when regional lymph node involvement is confirmed in the cystectomy specimen.
- In metastatic or recurrent disease, the highest response rates are seen with cisplatin-containing regimens.
Prostate Cancer
- Prostate cancer is the most common cancer in men behind nonmelanoma skin cancer.
- Prostate-specific antigen is useful as a marker for recurrence, bulk of disease, and response to therapy and may detect asymptomatic early-stage disease.
- Local control of the primary lesion can be achieved with either prostatectomy or radiation therapy.
- In patients with metastatic disease, bilateral orchiectomy and LHRH analogs with or without an antiandrogen produce tumor regression in approximately 85% of patients for a median of 18 to 24 months.
- Disease that has relapsed after hormonal therapy may respond to withdrawal of that antiandrogen.10
- Anthracyclines, taxanes, vinblastine, estramustine, sipuleucel-T, and abitaterone are options in hormone-refractory disease.
- Disease that has relapsed after hormonal therapy may respond to withdrawal of that antiandrogen.10
- Anemia and bone pain dominate the advanced phases of this disease and are best relieved with transfusions, growth factors, and palliative radiation therapy.
Renal Cell Cancer
- Renal cell cancer is treated by surgical resection, which may be curative if disease is localized; no effective adjuvant therapy is available. Cytoreductive nephrectomy is offered in select stage IV patients.
- Multitargeted tyrosine kinase inhibitors (TKIs) (sunitinib, sorafenib, and pazopanib) have been approved for the treatment of metastatic renal cell cancer. These agents appear more active and better tolerated than previously available agents. Other options include temsirolimus, bevacizumab plus interferon, and high-dose interleukin-2.
Testicular Cancer
- Considered one of the most curable malignancies and should be treated aggressively.
- A patient suspected of having cancer of the testis should have tissue obtained only through an inguinal orchiectomy.
- The initial evaluation should include serum α-fetoprotein and β-human chorionic gonadotropin levels and a CT scan of the abdomen and pelvis.
- Most patients with seminoma should be treated with radiation therapy after primary treatment with orchiectomy.
- In nonseminomatous germ cell cancer, a retroperitoneal lymph node dissection should be performed for staging, except in the instance of bulky abdominal disease or pulmonary metastasis.
- If microscopic disease is identified at surgery, two alternatives are acceptable: two cycles of postoperative chemotherapy or observation until relapse occurs followed by institution of chemotherapy.
- With gross metastatic disease, cisplatin-based chemotherapy is curative for most germ cell cancers. If tumor markers normalize after chemotherapy but a radiographic mass persists, exploratory surgery should be performed. The lesion proves to be residual cancer in approximately one-third of the patients. Patients with residual cancer should receive additional chemotherapy.11
- If microscopic disease is identified at surgery, two alternatives are acceptable: two cycles of postoperative chemotherapy or observation until relapse occurs followed by institution of chemotherapy.
- Sperm banking should be discussed with patients of reproductive age prior to treatment.
Gynecologic Malignancies
Cervical Cancer
- The recognized risk factors are multiparity, multiple sexual partners, and infection with human papillomavirus (HPV).
- Carcinoma in situ and superficial disease can be treated by endocervical cone biopsy.
- Microinvasive disease is treated with an abdominal hysterectomy.
- Advanced local disease (invasion of the cervix or local extension) is initially treated with surgery or radiation therapy, or both. The addition of chemotherapy to radiation therapy postoperatively is associated with improved survival.12
- Inoperable cancer can be controlled with radiation therapy; metastatic disease is treated with cisplatin-based chemotherapy.
- The HPV vaccine (covering types 6, 11, 16, & 18) is recommended for young women ages 9 to 26 in hopes of reducing the rates of cervical and vaginal carcinoma (see Chapter 5).
Ovarian Cancer
- Ovarian cancer is primarily a disease of postmenopausal women.
- Because symptoms are uncommon with localized disease, most patients present with advanced local disease, malignant ascites, or peritoneal metastases.
- Surgical staging and treatment include a total abdominal hysterectomy (TAH), bilateral oophorectomy, lymph node sampling, omentectomy, peritoneal cytology, and removal of all gross tumor. If the tumor is localized to the ovary, the surgery may be curative and further treatment is not routinely recommended. However, if microscopic foci of cancer are identified, chemotherapy is administered postoperatively.
- The serum marker CA-125, although not specific, is elevated in >80% of women with epithelial ovarian cancer and is a sensitive indicator of response and recurrence.
Endometrial Cancer
- The risks include obesity, nulliparity, early age at menarche, late age at menopause, polycystic ovaries, older age, Lynch syndrome, and the use of unopposed estrogens (including tamoxifen).
- Patients generally present with vaginal bleeding.
- Surgery TAH and bilateral salpingo-oophorectomy (BSO) and radiation therapy (tumor-directed external beam radiation and brachytherapy) are often curative.
Head and Neck Cancer
- Head and neck cancer is usually squamous cell.
- It may arise in a variety of sites, each of which has a different natural history.
- Early lesions can be cured with surgery, radiation therapy, or both.
- Despite aggressive surgical and radiation therapy, approximately 65% of patients with head and neck cancer have uncontrolled local disease.
- The addition of chemotherapy to radiation therapy improves the survival in patients with nasopharyngeal cancers and selected patients with other primary disease sites.13
Malignant Melanoma
- This should be considered when evaluating any changing or enlarging nevus. Suspicious lesions should be removed by excisional biopsy. Subsequently, a wide local excision is performed to remove possible vertical and radial spread of tumor.
- Deeper invasion is associated with a worse prognosis.
- Adjuvant interferon is an option for melanoma patients with nodal involvement.
- Systemic disease may respond to ipilimumab (monoclonal antibody targeting CTLA-4) or vemurafenib (targeting BRAF V600 mutation). Other options include dacarbazine, interferon-α, or high-dose interleukin-2.
Sarcomas
- Sarcomas are tumors arising from mesenchymal tissue and occur most commonly in soft tissue or bone.
- Initial evaluation should include a CT scan of the chest, as hematogenous spread to the lungs is common.
Soft Tissue Sarcoma
- Prognosis is primarily determined by tumor grade and not by the cell of origin.
- Surgical resection should be performed when feasible and may be curative.
- In low-grade tumors, local and regional recurrence is most common, and adjuvant radiation therapy may be of benefit.
- High-grade tumors often recur systemically but no advantage to the routine use of adjuvant chemotherapy has been demonstrated.
- In metastatic disease, doxorubicin, ifosfamide, and dacarbazine produce responses in 40% to 55% of patients. Targeted agents such as pazopanib, imatinib, and sunitinib have also shown therapeutic efficacy.
Osteogenic Sarcoma
- Osteogenic sarcoma is usually treated with neoadjuvant chemotherapy followed by surgical resection. If this results in a good response, further adjuvant chemotherapy is recommended. In patients who are not resectable after neoadjuvant chemotherapy, further chemotherapy or radiation are options.
- Treatment of isolated pulmonary metastasis by surgical resection is associated with long-term survival.
Kaposi Sarcoma
- In an immunocompetent patient, Kaposi sarcoma is generally a low-grade lesion of the lower extremities that is readily treated with local radiation therapy or vinblastine.
- When Kaposi sarcoma complicates organ transplantation or AIDS, it is more aggressive and may arise in visceral sites.
- Liposomal doxorubicin alone is as effective as combination chemotherapy for palliation.14 Paclitaxel is another systemic option.
Lymphoma
Hodgkin Disease
- Treatment is based on the presenting stage of the disease; the cell type is relatively unimportant in the natural history and prognosis.
- Initial staging evaluation includes a CT scan of the chest, abdomen, and pelvis, PET/CT, and bilateral bone marrow biopsies to determine the clinical stage of the disease.
- Stages IA and IIA (favorable disease) are treated with a combination of chemotherapy and radiation or chemotherapy alone as an alternative treatment option.
- Stage IA and IIA (unfavorable disease) and IIIA disease are treated with chemotherapy followed by consolidative radiation therapy.
- All Stage IV patients should receive combination chemotherapy followed by consolidative radiation, if the patient presented with bulky mediastinal disease.
- When B symptoms are present, chemotherapy is recommended regardless of the stage.
Non-Hodgkin Lymphoma
- Low-grade lymphoma
- It often involves the bone marrow at diagnosis but the disease has an indolent course.
- Because this tumor is not curable with standard chemotherapy, treatment can be delayed until the patient is symptomatic (i.e., watch and wait).
- Radiation therapy or an alkylating agent (e.g., cyclophosphamide) can be used to ameliorate symptoms.
- Radiation therapy may produce long-term complete remission in stage I or II disease.
- Rituximab produces an objective response in approximately 50% of patients with follicular lymphoma without the usual toxicities of chemotherapy in the elderly or infirm.
- It often involves the bone marrow at diagnosis but the disease has an indolent course.
- Intermediate-grade lymphoma
- This has a more aggressive course, usually does not involve the bone marrow at diagnosis, and can be cured with chemotherapy.
- Complete response rates exceed 80%.
- Features associated with a lower likelihood of cure include an elevated lactate dehydrogenase level, stage III/IV disease, age >60 years, more than one extranodal site, and poor performance status.
- This has a more aggressive course, usually does not involve the bone marrow at diagnosis, and can be cured with chemotherapy.
- High-grade lymphoma
- This subtype includes Burkitt and lymphoblastic lymphoma, the most aggressive subtypes that have a high frequency of CNS and bone marrow involvement.
- Cerebrospinal fluid (CSF) cytology should be included as part of the initial evaluation.
- Combination chemotherapy is the mainstay of treatment and should include CNS prophylaxis, if the CSF is cytologically free of tumor.
- If tumor cells are seen in the CSF, additional therapy may be indicated.
- Prophylaxis to prevent tumor lysis syndrome should be initiated before induction chemotherapy.
- This subtype includes Burkitt and lymphoblastic lymphoma, the most aggressive subtypes that have a high frequency of CNS and bone marrow involvement.
Leukemia
Acute Leukemias
- Acute myeloid leukemia (AML)
- Acute myeloid leukemia constitutes approximately 80% of adult acute leukemia.
- Approximately 50% to 80% of patients achieve complete remission with induction chemotherapy that includes cytarabine (cytosine arabinoside [ara-C]) and daunorubicin.
- Consolidation therapy is given with at least one additional cycle of chemotherapy, which is typically ara-C at a dose of 10 to 30 times that used for induction (high-dose ara-C). High-dose ara-C consolidation results in cure in approximately 30% to 40% of patients <60 years of age.
- Pretreatment factors associated with a low (<10%) chance for cure includes the following: preceding myelodysplastic syndrome, prior exposure to radiation, benzene, or chemotherapy, and adverse cytogenetic abnormalities.
- For these high-risk patients, allogeneic stem cell transplant in first remission increases the likelihood of cure.
- Acute myeloid leukemia constitutes approximately 80% of adult acute leukemia.
- Acute promyelocytic leukemia
- Acute promyelocytic leukemia is characterized by a chromosomal translocation (t[15;17]) that results in a hybrid protein (PML-RAR).
- Induction treatment with oral tretinoin (all-trans retinoic acid) plus chemotherapy results in complete remission in >90% of patients.
- After consolidation chemotherapy, approximately 75% of patients are cured.
- Acute promyelocytic leukemia is characterized by a chromosomal translocation (t[15;17]) that results in a hybrid protein (PML-RAR).
- Acute lymphocytic leukemia
- Typically a disease of childhood with a median age at diagnosis of 13 years. It represents only 20% of all leukemias in adults.
- For adults, induction and consolidation involve treatment with multiple chemotherapeutic agents over a period of approximately 6 months followed by at least 18 months of lower-dose maintenance chemotherapy.
- To prevent CNS relapse, patients receive IT chemotherapy and either cranial radiation or CNS-penetrating chemotherapy.
- Approximately 60% to 80% of adults achieve complete remission, with about 30% to 40% cured. Increasing age, higher white blood cell count, and longer time to remission are associated with reduced survival. Cytogenetics is crucial in determining prognosis and allogeneic stem cell transplantation during the first remission should be considered in patients with a poor prognosis.
- Typically a disease of childhood with a median age at diagnosis of 13 years. It represents only 20% of all leukemias in adults.
Chronic Leukemias
- Chronic lymphocytic leukemia
- Treatment of CLL is similar to that for low-grade lymphoma except that fludarabine appears to be more active than alkylating agents.
- Median survival is approximately 6 to 8 years.
- Anemia and thrombocytopenia are associated with shortened survival.
- As in low-grade lymphoma, patients are treated for control of symptoms or cytopenias.
- Because CLL is accompanied by immunodeficiency, life-threatening infections may occur. Therefore, febrile patients must be evaluated carefully.
- Autoimmune hemolytic anemia or immune thrombocytopenia may develop as complications of CLL and are treated with glucocorticoids (e.g., prednisone, 1 mg/kg PO daily) or chemotherapy, or both.
- CLL may transform to an intermediate or high-grade lymphoma (Richter transformation).
- Treatment of CLL is similar to that for low-grade lymphoma except that fludarabine appears to be more active than alkylating agents.
- Chronic myelogenous leukemia
- During the stable phase of the CML, the disease can be controlled, and most patients are asymptomatic.
- Imatinib is an orally administered medication designed specifically to inhibit the BCR-ABL tyrosine kinase. Because imatinib is highly active and has few toxicities, it is currently the first-line therapy for this disease. Even blast-phase CML or Philadelphia chromosome–positive acute leukemia may respond to imatinib. Responses in this setting are generally of relatively short duration.
- Next generation TKIs nilotinib and dasatinib are also first-line therapy options.
- Allogeneic transplant is appropriate in patients with blast phase, patients with BCR-ABL mutations resistant to all TKIs, and those intolerant of all TKIs.
- During the stable phase of the CML, the disease can be controlled, and most patients are asymptomatic.
- Hairy cell leukemia
- For hairy cell leukemia, a single 7-day course of chlorodeoxyadenosine (cladribine) produces remission in >90% of patients.
- Although this drug is not curative, 5-year progression-free survival exceeds 50%.
- For hairy cell leukemia, a single 7-day course of chlorodeoxyadenosine (cladribine) produces remission in >90% of patients.
Multiple Myeloma
- Treatment of MM depends on whether the patient is a candidate for stem cell transplant. Steroids such as dexamethasone or prednisone are included in all treatment regimens. Alkylating agents such as melphalan are not recommended for transplant candidates.
- Local radiation therapy can be used to relieve painful bone lesions, and zoledronic acid, 4 mg IV every month decreases skeletal complications.
- Thalidomide and lenalidomide are immunomodulatory agents that have been shown to be effective in MM.
- Because thalidomide can cause severe fetal malformations, prescribing this medication requires participation in a prescriber program.
- Prophylaxis with anticoagulation agents is also recommended.
- Because thalidomide can cause severe fetal malformations, prescribing this medication requires participation in a prescriber program.
- Bortezomib (Velcade) is a proteasome inhibitor that degrades ubiquitinated proteins which has shown activity in MM.
- Treatment options include various combinations of the above-mentioned agents with adjustment based on whether a patient is a transplant candidate.
- After induction chemotherapy, consolidation with high-dose therapy and autologous stem cell transplant improves survival.
COMPLICATIONS
Complications Related to Tumor
Brain Metastasis
- Patients with parenchymal brain metastasis may present with headache, mental status changes, weakness, or focal neurologic deficits. Papilledema is observed in only 25% of patients.
- In individuals with malignancy, a CT scan of the head showing one or more round, contrast-enhancing lesions surrounded by edema is usually sufficient for the diagnosis. If cancer has not been diagnosed previously, tissue should be obtained from the brain lesion or a more accessible site before radiation therapy is initiated.
- Therapy with dexamethasone, 10 mg IV or PO, should be initiated to decrease cerebral edema and should be continued at a dosage of 4 to 6 mg PO every 6 hours throughout the course of radiation therapy, or longer if symptoms related to edema persist.
- Subsequent therapy depends on the number and location of the brain lesions as well as the prognosis of the underlying cancer.
- Patients with a chemotherapy-responsive neoplasm and a solitary accessible lesion should be considered for surgical resection.
- All patients who have not received prior radiation therapy should be given whole-brain radiation therapy.
- Meningeal carcinomatosis should be suspected in a cancer patient with headache or cranial neuropathies.
- This pattern of spread is most often seen with lung cancer, breast cancer, melanoma, or lymphoma.
- The diagnosis is confirmed by cytology of the CSF.
- A CT scan of the head should be performed to rule out parenchymal metastases or hydrocephalus before a lumbar puncture is performed.
- Local radiation therapy or IT chemotherapy may provide temporary relief of symptoms.
- This pattern of spread is most often seen with lung cancer, breast cancer, melanoma, or lymphoma.
Spinal Cord Compression
- Spinal cord compression is most commonly caused by hematogenous spread of cancer to the vertebral bodies followed by expansion into the spinal canal or ischemia of the spinal cord.
- The most common malignancies causing spinal cord compression are breast, lung, and prostate cancer, but the diagnosis should be considered in any patient with cancer who complains of back pain.
- Magnetic resonance imaging is the imaging modality of choice to assess for acute cord compression.
- Treatment involves urgent neurosurgical and radiation oncology consultation in addition to high-dose corticosteroid therapy.
Superior Vena Cava Obstruction
- Most commonly caused by cancers that arise in or spread to the mediastinum, such as lymphoma or lung cancer.
- The compressed superior vena cava leads to swelling of the face or trunk, chest pain, cough, and shortness of breath. A mediastinal mass may compromise the airway.
- Dilated superficial veins of the chest, neck, or sublingual area suggest an engorged collateral circulation.
- The presence of a mass on chest radiograph or CT scans usually confirms the diagnosis.
- If the histologic origin of the obstruction is unknown, tissue can be obtained for diagnosis via bronchoscopy or mediastinoscopy.
- Therapy is directed at the underlying disease.
- Neoplasms that are not responsive to chemotherapy are treated with radiation therapy.15
Malignant Pericardial Effusions
- Most malignant pericardial effusions result from cancer of the breast or lung.
- Initial presentations range from dyspnea to acute cardiovascular collapse due to cardiac tamponade requiring emergency pericardiocentesis.
- After cardiovascular stabilization, some patients may improve with treatment if the tumor is chemotherapy sensitive.
- When the pericardial effusion is a complication of uncontrolled disease, palliation can be achieved by pericardiocentesis with sclerosis.
- Subxiphoid pericardiotomy can be performed in patients whose effusions do not respond to other treatment.
Malignant Pleural Effusions
- Malignant pleural effusions develop as a result of pleural invasion by tumor or obstruction of lymphatic drainage.
- When systemic control is impossible and reaccumulation of fluid occurs rapidly after drainage, removal of the fluid followed by instillation of a sclerosing agent into the pleural space is recommended.
- Resistant effusions can be controlled with pleurectomy or placement of an indwelling pleural catheter, which can be used to drain pleural fluid as needed.
Malignant Ascites
- Most commonly caused by peritoneal carcinomatosis and best controlled by systemic chemotherapy.
- Therapeutic paracenteses can provide symptomatic relief.
- Intraperitoneal instillation of chemotherapy has been used but is not routinely recommended.
Bone Metastases
- Bone metastases can result in spontaneous (pathologic) fractures.
- Prophylactic surgical pinning and radiation therapy may be indicated.
- Bone modifying agents (e.g., zoledronic acid, pamidronate, and denosumab) can also protect against skeletal-related events.
Paraneoplastic Syndromes
- Are complications of malignancy not directly caused by a tumor mass effect and are presumed to be mediated by either secreted tumor products or the development of autoantibodies.
- Paraneoplastic syndromes can affect virtually every organ system, and, in most cases, successful treatment of the underlying malignancy eliminates these effects.
- Metabolic complications
- Hypercalcemia is the most common metabolic complication in malignancy and can cause mental status changes, gastrointestinal (GI) discomfort, arrhythmias, and constipation.
- The syndrome of inappropriate antidiuretic hormone (SIADH) should be considered in a euvolemic cancer patient with unexplained hyponatremia. Although a variety of neoplasms have been described in association with SIADH, SCLC is most often responsible.
- Cancer-related anorexia and cachexia (CRCA):
- A clinical syndrome of anorexia, distortion of taste perception, and loss of muscle mass.
- The asthenic appearance of patients is more often related to tumor type than to tumor burden.
- Mirtazapine 15 to 30 mg PO daily has been used as an appetite stimulant and is a promising agent in CRCA treatments.16 Other appetite stimulants include corticosteroids, cannabinoids, and promotility agents such as metoclopramide.
- A clinical syndrome of anorexia, distortion of taste perception, and loss of muscle mass.
- Hypercalcemia is the most common metabolic complication in malignancy and can cause mental status changes, gastrointestinal (GI) discomfort, arrhythmias, and constipation.
- Neuromuscular complications
- Dermatomyositis, more often than polymyositis, has been associated with a variety of malignancies, including NSCLC and colon, ovarian, and prostate cancers.
- Successful treatment of the underlying malignancy may result in resolution of the symptoms.
- In a patient with no known malignancy, an exhaustive search for a malignancy is not recommended because a primary malignancy is found in <20% of patients.17
- Successful treatment of the underlying malignancy may result in resolution of the symptoms.
- Lambert-Eaton myasthenic syndrome is characterized by proximal muscle weakness, decreased or absent deep tendon reflexes, and autonomic dysfunction.
- Electromyography using high-frequency nerve stimulation may show posttetanic potentiation.
- SCLC is most often associated with this syndrome, and effective chemotherapy may result in improvement.
- Worsening symptoms have been reported with the use of calcium channel antagonists; these agents are contraindicated in this syndrome.18
- Electromyography using high-frequency nerve stimulation may show posttetanic potentiation.
- Dermatomyositis, more often than polymyositis, has been associated with a variety of malignancies, including NSCLC and colon, ovarian, and prostate cancers.
- Hematologic complications
- Although cytopenias occur more often as a complication of treatment or marrow involvement with cancer, elevated blood counts may be explained by paraneoplastic syndromes.
- Erythrocytosis is a rare complication of hepatoma, renal cell cancer, and benign tumors of the kidney, uterus, and cerebellum. Debulking the tumor with surgery or radiation therapy generally results in resolution of the erythrocytosis. Occasionally, therapeutic phlebotomy is indicated.
- Granulocytosis (leukemoid reaction) in the absence of infection is seen with cancers of the stomach, lung, pancreas, and brain, as well as lymphoma. Because the neutrophils are mature and seldom exceed 100,000/mm3, complications are rare and intervention is generally unnecessary.
- Thrombocytosis in patients with cancer may be caused by splenectomy, iron deficiency, acute hemorrhage, or inflammation; treatment is usually not necessary.
- Although cytopenias occur more often as a complication of treatment or marrow involvement with cancer, elevated blood counts may be explained by paraneoplastic syndromes.
- Thromboembolic complications
- Mucin-secreting adenocarcinomas of the GI tract and lung cancer have been associated with a hypercoagulable state, resulting in recurrent venous and arterial thromboembolism.
- Nonbacterial thrombotic (marantic) endocarditis, usually involving the mitral valve, may also occur.
- Heparin anticoagulation or low molecular weight heparin should be instituted, as well as treatment of the underlying cancer.19
- Mucin-secreting adenocarcinomas of the GI tract and lung cancer have been associated with a hypercoagulable state, resulting in recurrent venous and arterial thromboembolism.
- Glomerular injury
- Glomerular injury has been observed as a paraneoplastic syndrome.
- Minimal change disease is often associated with lymphoma, especially Hodgkin disease.
- Membranous glomerulonephritis is more often seen with solid tumors.
- The process can be reversed with treatment of the underlying cancer.
- Glomerular injury has been observed as a paraneoplastic syndrome.
- Clubbing and hypertrophic osteoarthropathy
- This includes polyarthritis and periostitis of long bones.
- Most often observed in NSCLC but also seen with lesions that are metastatic to the mediastinum.
- Some improvement in the osteoarthropathy can be achieved with nonsteroidal anti-inflammatory drugs (NSAIDs), but definitive therapy requires treatment of the underlying malignancy.
- This includes polyarthritis and periostitis of long bones.
- Fever
- Fever may accompany lymphoma, renal cell cancer, and hepatic metastasis.
- Once an infectious etiology for the fever has been excluded, NSAIDs (e.g., ibuprofen, 400 mg PO every 6 hours, or indomethacin, 25 to 50 mg PO tid) may provide symptomatic relief.
- Fever may accompany lymphoma, renal cell cancer, and hepatic metastasis.
Complications Related to Treatment
Cancer treatments can cause serious or life-threatening toxicity. The most common and predictable toxicities are to the rapidly proliferating cells of hematopoietic and mucosal tissue. Because repair of these tissues cannot be accelerated, palliation during the healing process is the primary goal.
Complications of Radiation Therapy
- Toxicity is related to the location of the therapy, total dose delivered, and rates of delivery. Large-dose fractions of radiation are associated with greater toxicity to the normal tissues encompassed in the radiation field.
- Acute toxicity
- Develops within the first 3 months of therapy and is characterized by an inflammatory reaction in the tissue receiving radiation.
- Such toxicity may respond to anti-inflammatory agents such as glucocorticoids.
- Local irritations or burns in the treatment field generally resolve with time.
- Close observation and treatment of any infections and palliation of symptoms, such as pain, dysphagia, dysuria, or diarrhea (depending on the site of treatment) are the mainstays of supportive care until healing has occurred.
- Develops within the first 3 months of therapy and is characterized by an inflammatory reaction in the tissue receiving radiation.
- Subacute and chronic toxicity
- Tends to be less amenable to therapy, as fibrosis and scarring are present.
- Daily amifostine before head and neck radiation therapy decreases the incidence of xerostomia.20
- Tends to be less amenable to therapy, as fibrosis and scarring are present.
Tumor Lysis Syndrome
- Tumor lysis syndrome occurs in patients with rapidly proliferating neoplasms that are highly sensitive to chemotherapy.
- Rapid tumor cell death releases intracellular contents and causes hyperkalemia, hyperphosphatemia, and hyperuricemia.
- Although reported in the treatment of a variety of malignancies, it is usually associated with high-grade non-Hodgkin lymphoma and acute leukemia.
- The diagnosis of tumor lysis syndrome is based on susceptibility, clinical suspicion, and close monitoring of laboratory data in patients at risk. Rapidly progressive hyperkalemia, hyperphosphatemia, and hyperuricemia as well as acutely worsening renal failure are the hallmarks.
- Prophylaxis and pretreatment are paramount in preventing tumor lysis syndrome.
- During induction chemotherapy, prophylactic measures typically include the following:
- Allopurinol, 300 to 600 mg PO daily, and aggressive IV volume expansion (e.g., 3,000 mL/m2/day).
- The addition of sodium bicarbonate, 50 mEq/1,000 mL IV fluid, to alkalinize the urine may prevent uric acid nephropathy and acute renal failure, but should be avoided in hyperphosphatemia.
- Allopurinol, 300 to 600 mg PO daily, and aggressive IV volume expansion (e.g., 3,000 mL/m2/day).
- Rasburicase is a recombinant urate oxidase enzyme that catalyzes the oxidation of uric acid into allantoin, a soluble metabolite. It can be used prophylactically or in the treatment of hyperuricemia.
- Despite these preventive measures, hemodialysis may be needed for hyperkalemia, hyperphosphatemia, acute renal failure, or fluid overload.
Hematologic Complications
- Myelosuppression and febrile neutropenia
- A febrile neutropenic patient should be presumed to be infected and must be evaluated and treated promptly in an inpatient setting.
- The risk of infection increases dramatically with neutropenia (defined as an absolute neutrophil count of <500/mm3) and is directly related to the duration of the neutropenia.
- Fever is defined as a single core temperature reading of >38.3°C orally or two readings of >38.0°C spanning 1 hour.
- Other clinical signs of infection must be considered because the inflammatory response may be muted in the absence of neutrophils.
- A febrile neutropenic patient should be presumed to be infected and must be evaluated and treated promptly in an inpatient setting.
- Growth factors for myelosuppression
- Growth factors include many cytokines that may ameliorate the myelosuppression associated with cytotoxic chemotherapy. They act on hematopoietic cells, stimulating proliferation, differentiation, commitment, and some functional activation.
- Because they can increase myelosuppression, they should not be given within 24 hours of chemotherapy or radiation.
- Filgrastim (G-CSF, given at an initial dose of 5 μg/kg SC/day or IV), and pegfilgrastim (a pegylated form of G-CSF 6 mg single dose), beginning the day after the last dose of cytotoxic chemotherapy, may reduce the incidence of febrile neutropenic events. Blood counts should be monitored twice a week during therapy. Bone pain is a common toxicity that can be managed with nonopiate analgesics.
- Sargramostim (GM-CSF) given subcutaneously at a dose of 250 μg/m2/day beginning the day after the last dose of cytotoxic chemotherapy, shortens the period of neutropenia after stem cell transplant.
- Growth factors include many cytokines that may ameliorate the myelosuppression associated with cytotoxic chemotherapy. They act on hematopoietic cells, stimulating proliferation, differentiation, commitment, and some functional activation.
- Anemia
- Anemia is a common side effect of multiple chemotherapeutic agents. Symptoms include fatigue, dyspnea, or lethargy.
- RBC transfusions are indicated for patients who have symptoms of anemia, active bleeding, or a hemoglobin concentration below 7 to 8 g/dL. Because of anecdotal reports of graft versus host disease (GVHD) associated with transfusions, radiation of all blood products is generally recommended for immunosuppressed marrow transplant patients.
- Recombinant erythropoietin (epoetin alfa) given at a starting dose of 150 U/kg SC three times a week or 40,000 U SC weekly has been shown to improve anemia and decrease transfusion requirements in cancer patients, particularly those in whom the anemia is predominantly caused by cytotoxic chemotherapy.21
- Darbepoetin alfa is a recombinant erythropoietin with a longer half-life. It is started at 500 μg SC every 3 weeks.
- Erythropoiesis-stimulating agents (ESA) such as epoetin and darbepoetin can only be administered with patient consent under a Risk Evaluation Mitigation Strategy (REMS) program. Hematocrit should be monitored weekly during therapy, and the dosage should be adjusted accordingly. ESAs should be discontinued when the chemotherapy is complete and the anemia has resolved. They should not be used when the patient is undergoing potentially curative therapy.
- Anemia is a common side effect of multiple chemotherapeutic agents. Symptoms include fatigue, dyspnea, or lethargy.
- Thrombocytopenia
- Thrombocytopenia is another common side effect of chemotherapeutic agents toxic to the bone marrow. Symptoms include easy bruising and bleeding (e.g., epistaxis and gingival bleeding).
- Thrombocytopenia <10,000/mm3 which is the result of chemotherapy should be treated with platelet transfusions to minimize the risk of spontaneous hemorrhage.
- Interleukin-11 was approved to reduce the duration and severity of thrombocytopenia after chemotherapy. However, limited efficacy and significant toxicity (fluid retention and atrial arrhythmias) have limited its use.
- When prolonged thrombocytopenia is anticipated, histocompatibility testing should be performed before therapy so that HLA-matched single-donor platelets can be provided when alloimmunization makes the patient refractory to random-donor platelets.
- Thrombocytopenia is another common side effect of chemotherapeutic agents toxic to the bone marrow. Symptoms include easy bruising and bleeding (e.g., epistaxis and gingival bleeding).
Gastrointestinal Complications
- Stomatitis
- The severity of stomatitis ranges from mild (oral discomfort) to severe (ulceration, impaired oral intake, and hemorrhage). Toxicity is more severe with simultaneous radiation therapy.
- It is often the dose-limiting toxicity of methotrexate and 5-FU but can be an unpleasant consequence of many chemotherapeutic agents.
- Healing generally occurs within 7 to 10 days of the development of symptoms.
- For mild cases of stomatitis, oral rinses (chlorhexidine, 15 to 30 mL swish and spit tid, or a combination of equal parts diphenhydramine elixir, saline, and 3% hydrogen peroxide) may provide relief. Polyvinylpyrrolidone-sodium hyaluronate gel can also be used.
- Palifermin, a keratinocyte growth factor analog, has been approved for use in chemotherapy-induced stomatitis.22
- In severe cases, IV morphine is appropriate and IV fluids can be used to supplement oral intake as needed.
- Patients with moderate or severe stomatitis may develop aspiration. Precautions should include elevation of the head of the bed and availability of a handheld suction apparatus.
- In severe or prolonged episodes, superinfection with Candida or herpes simplex is possible and requires appropriate diagnosis and antimicrobial intervention.
- The severity of stomatitis ranges from mild (oral discomfort) to severe (ulceration, impaired oral intake, and hemorrhage). Toxicity is more severe with simultaneous radiation therapy.
- Diarrhea
- In this context, diarrhea is the result of cytotoxicity to proliferating cells of the intestinal mucosa.
- The use of oral opioid agents as antidiarrheals is commonly limited by abdominal cramping.
- Severe diarrhea associated with 5-FU and LV may respond to octreotide, 150 to 500 μg SC tid.
- Diarrhea, sometimes severe, is a common side effect of irinotecan and can be treated with loperamide, 4 mg PO, and then 2 mg every 2 hours while awake and 4 mg every 4 hours during the night.
- In some cases, IV fluids are necessary to avoid intravascular volume depletion.
- In this context, diarrhea is the result of cytotoxicity to proliferating cells of the intestinal mucosa.
- Nausea and vomiting
- Nausea and vomiting occur with varying degrees and frequency. The focus is on prevention.
- Chemotherapy regimens are classified by emetic risk: high (>90%), moderate (30% to 90%), low (10% to 30%), and minimal (<10%) with recommendations for emesis prophylaxis dependent on level of risk. Suggestions for breakthrough antiemetic agent(s) are listed in Table 35-3.
- Nausea and vomiting occur with varying degrees and frequency. The focus is on prevention.
TABLE 35-3 Recommendations for Breakthrough Antiemetic Therapy
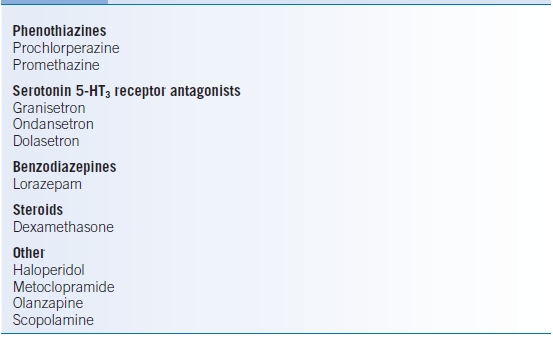
Adapted from NCCN Guidelines® Version 1.2013 Antiemesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


