Cardiovascular/Renal Agents
ANTIARRHYTHMIC (ANTIDYSRRHYTHMIC) AGENTS
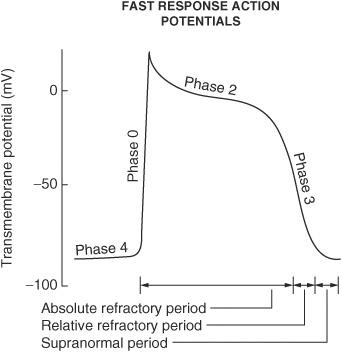
Describe what happens during each of the following phases of the cardiac action potential for fast-response fibers:
Phase 0
Sodium ion channels open (inward) which leads to membrane depolarization.
Phase I
Sodium ion channels are inactivated; potassium ion channels (outward) are activated; chloride ion channels (inward) are activated.
Phase II
Plateau phase; slow influx of calcium ion balanced by outward potassium ion current (delayed rectifier current IK)
Phase III
Repolarization phase; outward K+ current increases and inward calcium ion current decreases
Phase IV
Membrane returns to resting potential.
Figure 6.1
On what phase(s) of the cardiac action potential do amiodarone and sotalol work?
Phase 0 and phase III
On what phase(s) of the cardiac action potential do lidocaine, flecainide, and quinidine work?
Phase 0
On what phase(s) of the cardiac action potential do β-blockers work?
Phase II and phase IV
What is responsible for maintaining the electrochemical gradient at resting membrane potential?
Na+/K+-ATPase
What ion current is responsible for the depolarization of sinoatrial (SA) and atrioventricular (AV) nodal fibers?
Calcium ion (inward)
What ion current is responsible for the repolarization of SA and AV nodal fibers?
Potassium ion (outward)
How does phase IV of the action potential in slow-response fibers (SA and AV nodes) differ from that of fast-response fibers?
Slow-response fibers display automaticity (ability to depolarize spontaneously); rising phase IV slope of the action potential = pacemaker potential
What ion current is responsible for the “pacemaker current” (rising slope of phase IV) in slow-response fibers?
Sodium ion (inward); calcium ion (inward); potassium ion (outward)
The pacemaker of the heart has the fastest uprising phase IV slope; where is this pacemaker in nondiseased patients?
SA node
Where is the SA node located?
Right atrium
How do the effective refractory period (ERP) and relative refractory period (RRP) differ from each other?
No stimulus, no matter the strength, can elicit a response with fibers in the ERP, whereas a strong enough stimulus will elicit a response with fibers in the RRP.
What are the three states the voltage-gated Na+ channel exists in?
- Resting state
- Open state
- Inactivated state
What state(s) of the voltage-gated Na+ channel is/are most susceptible to drugs?
Open state; inactivated state
What two types of gates does the voltage-gated Na+ channel have?
- M (activating)
- H (inactivating)
Why is the rate of recovery from an action potential slower in ischemic tissue?
The cells are already partly depolarized at rest.
What class of antiarrhythmic agents has membrane-stabilizing effects?
β-Blockers
Antiarrhythmic agents are grouped into four classes according to what classification system?
Vaughn-Williams classification
Give the general mechanism of action for each of the following antiarrhythmic drug classes:
Class I
Na+ channel blockers
Class II
β-Blockers
Class III
K+ channel blockers
Class IV
Ca++ channel blockers
Class I antiarrhythmics are further subdivided into what classes?
la; Ib; Ic
Give examples of antiarrhythmic drugs in class la:
Quinidine (antimalarial/antiprotozoal agent); procainamide; disopyramide
Give examples of antiarrhythmic drugs in class Ib:
Lidocaine; mexiletine; tocainide; phenytoin
Give examples of antiarrhythmic drugs in class Ic:
Encainide; flecainide; propafenone; moricizine
Give examples of antiarrhythmic drugs in class II:
Propranolol; esmolol; metoprolol
Give examples of antiarrhythmic drugs in class III:
Amiodarone; sotalol; ibutilide; dofetilide
Give examples of antiarrhythmic drugs in class IV:
Verapamil; diltiazem
Name three antiarrhythmic drugs that do not fit in the Vaughn-Williams classification system:
- Digoxin
- Adenosine
- Magnesium
Magnesium is used to treat what specific type of arrhythmia?
Torsades de pointes (polymorphic ventricular tachycardia)
Adenosine is used to treat what types of arrhythmias?
Paroxysmal supraventricular tachycardia (PSVT), specifically narrow complex tachycardia or supraventricular tachycardia (SVT) with aberrancy; AV nodal arrhythmias (adenosine causes transient AV block). Note: synchronized cardioversion and not adenosine should be used on symptomatic patients or unstable tachycardia with pulses.
Where anatomically should the IV be placed to administer adenosine?
As close to the heart as possible, that is, the antecubital fossa since adenosine has an extremely short half-life. Adenosine rapid IV push should be followed immediately by a 5-10 cc (mL) flush of saline to facilitate its delivery to the heart.
What is the mechanism of action of adenosine?
Stimulates α1-receptors which causes a decrease in cyclic adenosine monophosphate (cAMP) (via Grcoupled second messenger system); increases K+ efflux leading to increased hyperpolarization; increases refractory period in AV node
What are the adverse effects of adenosine?
Flushing; chest pain; dyspnea; hypotension
What two drugs can antagonize the effects of adenosine?
- Theophylline
- Caffeine
How is adenosine dosed?
6 mg initially by rapid IV push; if not effective within 1-2 minutes, give 12 mg repeat dose (follow each bolus of adenosine with normal saline flush). The 12 mg dose may be repeated once.
What is the most deadly ion that can be administered?
Potassium ion
What ECG changes are seen in hyperkalemia?
Flattened P waves; widened QRS complex; peaked T waves; sine waves; ventricular fibrillation
What ECG changes are seen in hypokalemia?
Flattened or inverted T waves; U waves; ST-segment depression
What do class la antiarrhythmics do to each of the following?
Action potential duration
Increase
ERP
Increase
Conduction velocity
Decrease
Phase IV slope
Decrease
What do class Ib antiarrhythmics do to each of the following?
Action potential duration
Decrease
ERP
Little or no change
Conduction velocity
Decrease (primarily in ischemic tissue)
Phase IV slope
Decrease
What do class Ic antiarrhythmics do to each of the following?
Action potential duration
Little or no change
ERP
Little or no change
Conduction velocity
Decrease
Phase IV slope
Decrease
Drugs that affect the strength of heart muscle contraction are referred to as what types of agents?
Inotropes (either positive or negative)
Drugs that affect the heart rate are referred to as what types of agents?
Chronotropes (either positive or negative)
Drugs that affect AV conduction velocity are referred to as what types of agents?
Dromotropes (either positive or negative)
QT interval prolongation, and therefore torsades de pointes, is more likely to occur with what two classes of antiarrhythmics?
- la
- Ill
Which class la antiarrhythmic also blocks α-adrenergic and muscarinic receptors, thereby potentially leading to increased heart rate and AV conduction?
Quinidine
What are the adverse effects of quinidine?
Tachycardia; proarrhythmic; increased digoxin levels via protein-binding displacement; nausea; vomiting; diarrhea; cinchonism
What is cinchonism?
Syndrome that may include tinnitus; high-frequency hearing loss; deafness; vertigo; blurred vision; diplopia; photophobia; headache; confusion; delirium
What are the adverse effects of procainamide?
Drug-induced lupus (25%-30% of patients); proarrhythmic; depression; psychosis; hallucination; nausea; vomiting; diarrhea; agranulocytosis; thrombocytopenia; hypotension
What drugs can cause drug-induced lupus?
Procainamide; isoniazid (INH); chlorpromazine; penicillamine; sulfasalazine; hydralazine; methyldopa; quinidine; phenytoin; minocycline; valproic acid; carbamazepine; chlorpromazine
Which class la antiarrhythmic can cause peripheral vasoconstriction?
Disopyr amide
What are the adverse effects of disopyramide?
Anticholinergic adverse effects, such as urinary retention; dry mouth; dry eyes; blurred vision; constipation; sedation
True or False? Lidocaine is useful in the treatment of ventricular arrhythmias?
True
True or False? Lidocaine is useful in the treatment of atrial arrhythmias?
False
True or False? Lidocaine is useful in the treatment of AV junctional arrhythmias?
False
What are the adverse effects of lidocaine?
Proarrhythmic; sedation; agitation; confusion; paresthesias; seizures
What class Ib antiarrhythmic is structurally related to lidocaine?
Mexiletine
What class Ib antiarrhythmic can cause pulmonary fibrosis?
Tocainide
Propaf enone, even though a class Ic antiarrhythmic, exhibits what other type of antiarrhythmic activity?
β-Adrenergic receptor blockade
What famous trial showed that encainide and flecainide increased sudden cardiac death in postmyocardial infarction (MI) patients with arrhythmias?
Cardiac Arrhythmia Suppression Trial (CAST)
Sotalol, even though a class III antiarrhythmic, exhibits what other type of antiarrhythmic activity?
β-Adrenergic receptor blockade
Even though this agent is labeled as a Vaughn-Williams class III antiarrhythmic, it displays class I, II, III, and IV antiarrhythmic activity.
Amiodarone
What is the half-life of amiodarone?
40 to 60 days
What are the adverse effects of amiodarone?
Pulmonary fibrosis; tremor; ataxia; dizziness; hyperthyroidism; hypothyroidism; hepatotoxicity; photosensitivity; blue skin discoloration; neuropathy; muscle weakness; proarrhythmic; corneal deposits; lipid abnormalities; hypotension; nausea; vomiting; congestive heart failure (CHF); optic neuritis; pneumonitis; abnormal taste; abnormal smell; syndrome of inappropriate secretion of antidiuretic hormone (SIADH)
How should patients on amiodarone therapy be monitored?
ECG; thyroid function tests (TFTs); pulmonary function tests (PFTs); liver function tests (LFTs); electrolytes; ophthalmology examinations
Verapamil should not be given in what types of arrhythmias?
Wolff-Parkinson-White (WPW) syndrome; ventricular tachycardia
What are the adverse effects of verapamil?
Drug interactions; constipation; hypotension; AV block; CHF; dizziness; flushing
Digoxin is used to control ventricular rate in what types of arrhythmias?
Atrial fibrillation; atrial flutter
Digoxin-induced arrhythmias are treated by what drugs?
Lidocaine; phenytoin
Digoxin does what to each of the following?
Strength of heart muscle contraction
Increases (positive inotrope)
Heart rate
Decreases (negative chronotrope)
AV conduction velocity
Decreases (negative dromotrope)
What does QTc stand for?
Corrected QT interval
How is QTc calculated?
(QT)/(square root of R to R interval)
Why must the QT interval be corrected?
The QT interval is dependent on heart rate, so higher heart rates will display shorter QT intervals on ECG. It is corrected to remove the variable of the heart rate.
What is the normal value for QTc?
Less than 440 milliseconds
What does a long QT interval put a patient at risk for?
Torsades de pointes, a ventricular arrhythmia that can degenerate into ventricular fibrillation
CONGESTIVE HEART FAILURE AGENTS
What is the cardiac output equation?
Cardiac output (CO) = heart rate (HR) × stroke volume (SV)
What is normal CO?
5 L/min
What is the most common cause of right-sided heart failure?
Left-sided heart failure
Name three compensatory physiologic responses seen in congestive heart failure (CHF):
- Fluid retention
- Increased sympathetic drive
- Hypertrophy of cardiac muscle
Define preload:
The pressure stretching the ventricular walls at the onset of ventricular contraction; related to left ventricular end-diastolic volume/pressure
Define afterload:
The load or force developed by the ventricle during systole
What drugs are used to decrease preload?
Diuretics; vasodilators; angiotensin-converting enzyme inhibitors (ACEIs); angiotensin II receptor blockers (ARBs); nitrates
What drugs are used to decrease afterload?
Vasodilators; ACEIs; ARBs; hydralazine
What drugs are used to increase contractility?
Digoxin; phosphodiesterase inhibitors (amrinone and milrinone); β-adrenoceptor agonists
What is the mechanism of action of digoxin?
Inhibition of the Na+/K+-ATPase pump which leads to positive inotropic action (via increased intracellular sodium ions that exchanges with extracellular calcium ions; resulting increase in intracellular calcium ions leads to increased force of contraction)
What are the two digitalis glycosides?
- Digoxin
- Digitoxin
What are the adverse effects of digoxin?
Arrhythmias; nausea; vomiting; anorexia; headache; confusion; blurred vision; visual disturbances, such as yellow halos around light sources
What electrolyte disturbances predispose to digoxin toxicity?
Hypokalemia; hypomagnesemia; hypercalcemia
Digoxin can cause what types of arrhythmias?
Supraventricular tachycardias; AV nodal tachycardias; AV block; ventricular tachycardias; ventricular fibrillation; complete heart block
Can digoxin be used in WPW syndrome?
No. Since digoxin slows conduction through the AV node, the accessory pathway present in WPW is left unopposed, leading to supraventricular tachycardias and atrial arrhythmias.
How is digoxin toxicity treated?
Correction of electrolyte disturbances; antiarrhythmics; anti-digoxin Fab antibody (Digibind)
What drugs can increase digoxin concentrations?
Quinidine; amiodarone; erythromycin; verapamil
What drugs can decrease digoxin concentrations?
Loop diuretics; thiazide diuretics; corticosteroids
Does digoxin therapy in CHF lead to prolonged survival?
No. It is of symptomatic benefit only, improving quality, but not necessarily duration of life.
What classes of medications have been shown to increase survival in CHF patients?
ACEs/ARBs; β-blockers
How does dobutamine work in CHF?
β-Adrenergic agonist (sympathomimetic that binds to (β1-adrenoceptors) that increases force of contraction and vasodilation via increased cAMP
How do amrinone and milrinone work in CHF?
Inhibits phosphodiesterase (PDE) thereby increasing cAMP levels; increased cAMP leads to increased intracellular calcium; increased intracellular calcium leads to increased force of contraction; increased cAMP also leads to increased vasodilation
What are the side effects of the PDEIs?
Milrinone may actually decrease survival in CHF; amrinone may cause thrombocytopenia.
How do diuretics work in CHF?
Decrease in intravascular volume thereby decrease in preload; reduce pulmonary and peripheral edema often seen in CHF patients
How can increased sympathetic activity in CHF be counteracted?
β-Blockers
What two β-blockers have specific indications for the treatment of CHF?
- Metoprolol
- Carvedilol (mixed α-/β-blocker)
What is the mechanism of action of nesiritide?
Recombinant B-type natriuretic peptide that binds to guanylate cyclase receptors on vascular smooth muscle and endothelial cells, thereby increasing cyclic guanosine monophosphate (cGMP) levels; increased cGMP leads to increased relaxation of vascular smooth muscle
How do ACEIs work in CHF?
Inhibition of angiotensin-II (AT-II) production thereby decreasing total peripheral resistance (TPR) and thus afterload; prevents left ventricular remodeling
ANTIANGINAL AGENTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree