2 Cardiovascular system
The heart
Basic concepts
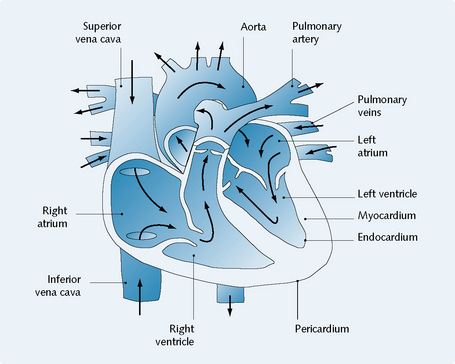
The flow of blood around the body is as follows (Fig. 2.1):
Cardiac rate and rhythm
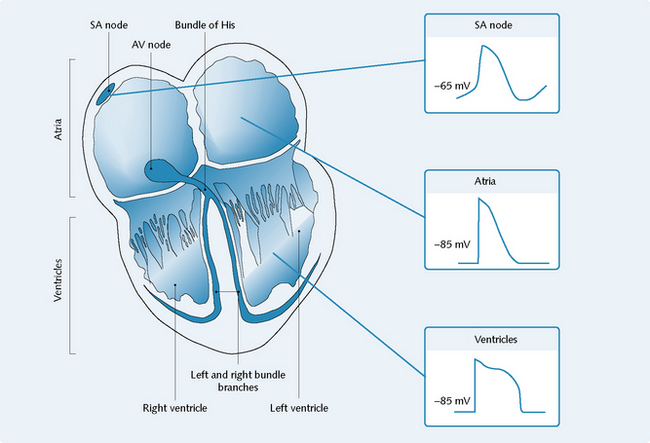
The secondary action potential generated by the AVN descends into the interventricular septum via the bundle of His. The bundle of His splits into left and right branches making contact with the Purkinje fibres, which conduct the impulse throughout the ventricles, causing them to contract (Fig. 2.2).
Cardiac action potential
The shape of the action potential is characteristic of the location of its origin (i.e. whether from nodal tissue, the atria or the ventricles) (Fig. 2.2).
Non-nodal cells
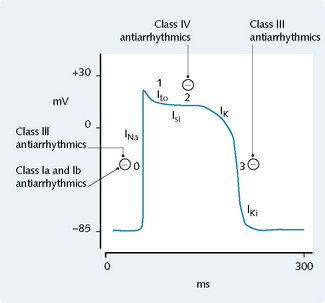
The resting membrane potential across the ventricular cell membrane is approximately − 85 mV; this is because the resting membrane is more permeable to potassium than to other ions. Four phases occurring at the ventricular cell membrane are (Fig. 2.3):
Nodal cells
The resting membrane potential of nodal cells is approximately − 60 mV.
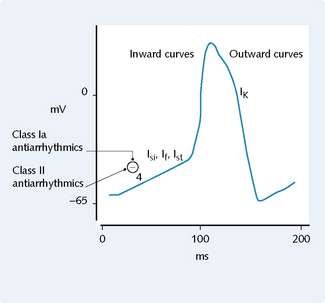
Nodal cells have a phase known as phase 4 (the pacemaker potential). This phase involves a gradual depolarization that occurs during diastole and is known as the f current (If′ funny). The f current is activated by hyperpolarization at − 45 mV, and consists of sodium and calcium ions entering the cell (Fig. 2.4).
Autonomic control of the heart
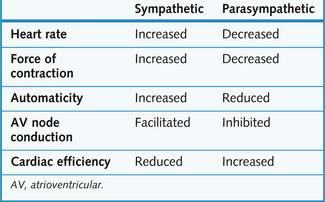
The effects of the sympathetic and parasympathetic nervous systems on the heart are summarized in Figure 2.5.
Cardiac contractility
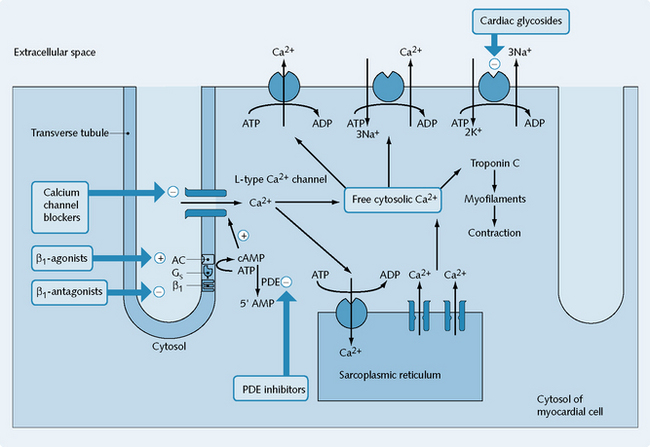
Myocardial contraction is the result of calcium entry through L-type channels, giving rise to an increase in cytosolic calcium in the myocytes (Fig. 2.6).
The calcium is derived from two sources:
Cardiac dysfunction and treatment
Congestive cardiac failure
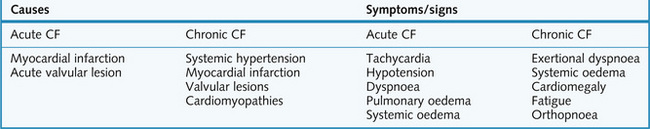
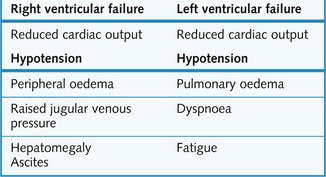
CCF occurs when the cardiac output does not meet the needs of the tissues. This is thought to be due to defective excitation–contraction coupling, with progressive systolic and diastolic ventricular dysfunction. Some of the causes, symptoms and signs of acute and chronic cardiac failure are given in Figure 2.7. The characteristics of left and right ventricular failure are listed in Figure 2.8.
The body attempts to compensate for the effects of CCF by two processes: extrinsic and intrinsic.
Extrinsic cardiac compensation
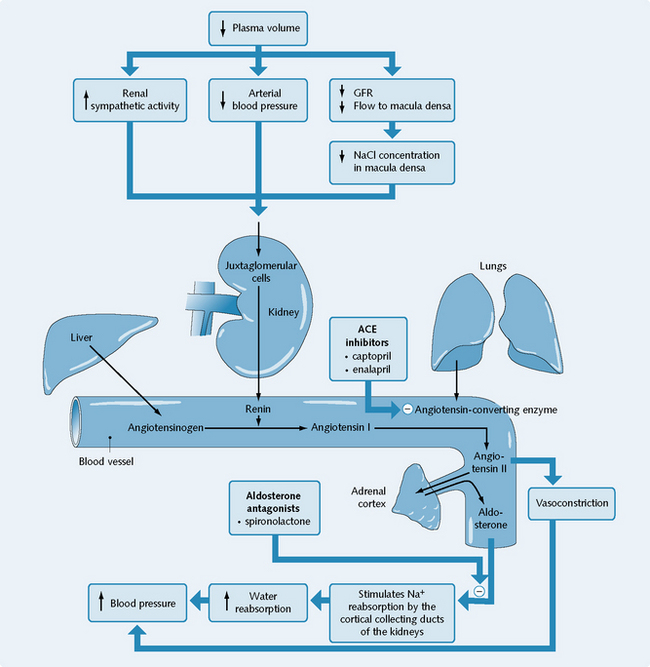
The reduced perfusion of the kidneys activates the renin–angiotensin system (RAS), leading to renin secretion and subsequent elevation of plasma angiotensin II and aldosterone levels (see Fig. 2.13). Angiotensin II causes peripheral vasoconstriction and aldosterone increases sodium retention, leading to increased water retention, oedema and an increased preload.
Drugs used in heart failure
Cardiac glycosides
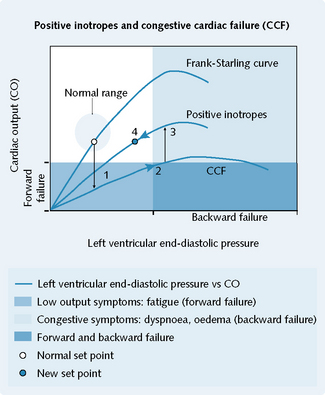
Prototypical cardiac glycosides are digoxin and digitoxin. The drugs in this class shift the Frank–Starling ventricular function curve to a more favourable position (Fig. 2.9).
Mechanism of action
Cardiac glycosides act by inhibiting the membrane Na+/K+ ATPase pump (see Fig. 2.6). This increases intracellular Na+ concentration, thus reducing the sodium gradient across the membrane and decreasing the amount of calcium pumped out of the cell by the Na+/Ca2+ exchanger during diastole. Consequently, the intracellular calcium concentration rises, thus increasing the force of cardiac contraction and maintaining normal blood pressure.
Adverse effects
Arrhythmias, anorexia, nausea and vomiting, visual disturbances, abdominal pain and diarrhoea.
Phosphodiesterase inhibitors
Mechanism of action
The type III PDE isoenzyme is found in myocardial and vascular smooth muscle.
Phosphodiesterase is responsible for the degradation of cAMP; thus, inhibiting this enzyme raises cAMP levels and causes an increase in myocardial contractility and vasodilatation (Fig. 2.6). Cardiac output is increased, and pulmonary wedge pressure and total peripheral resistance are reduced, without much change in heart rate or blood pressure.
Indications
PDE inhibitors are given for severe acute heart failure that is resistant to other drugs.
β-Adrenoceptor agonists
Examples of β-adrenoceptor agonists (p. 35) include dobutamine and dopamine. They are used intravenously in CCF emergencies (see Fig. 2.6).
Diuretics
The main diuretic drug classes are:
Diuretics inhibit sodium and water retention by the kidneys, and so reduce oedema due to heart failure. Venous pressure and thus cardiac preload are reduced, increasing the efficiency of the heart as a pump (see Ch. 7). Spironolactone appears to have a beneficial effect in cardiac failure at doses lower than it would be expected to function as a diuretic.
Angiotensin-converting-enzyme inhibitors
For details of angiotensin converting enzyme (ACE) inhibitors see p. 32.
Arrhythmias
The two main mechanisms by which cardiac rhythm becomes dysfunctional are:
Abnormal impulse generation
Automatic
Triggered
Forms of triggered abnormal impulse generation are:
Abnormal impulse conduction
Re-entry
Antiarrhythmic drugs
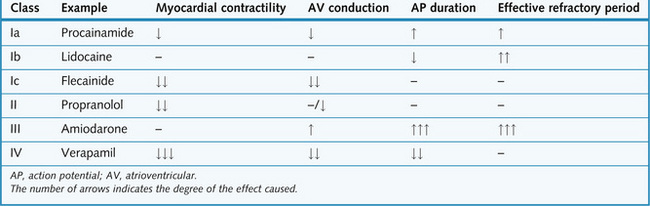
Antiarrhythmic drugs are classified according to a system devised by Vaughan Williams in 1970, and later modified by Harrison. A summary of the effects of the different classes of drug is given in Figure 2.10.
Class I
All class I drugs block the voltage-dependent sodium channels in a dose-dependent manner. Their action resembles that of local anaesthetics (Ch. 9).
All class I drugs have the following effects:
Class Ia
Examples of class Ia drugs include quinidine, procainamide and disopyramide.
Mechanism of action
Class Ia drugs block voltage-dependent sodium channels in their open (activated) or refractory (inactivated) state (see Figs. 2.3 and 2.4). Their effects are to slow phase 0 (increasing the effective refractory period) and phase 4 (reducing automaticity), and to prolong action potential duration.
Class Ib
Examples of class Ib drugs include lidocaine, mexiletine and phenytoin.
Mechanism of action
Class Ib drugs exert their effects in several ways (see Fig. 2.3). These include:
Indications
Ventricular arrhythmias following myocardial infarction. Phenytoin is used in epilepsy (Ch. 5).
Contraindications
Class Ib drugs should not be given to patients with SA disorders, AV block and porphyria.
Class II
Examples of class II drugs include propranolol, atenolol and pindolol (see Figs. 2.4 and 2.6).
Class III
Examples of class III drugs include bretylium, amiodarone, sotalol and ibutilide.
Mechanism of action
All class III drugs used clinically are potassium-channel blockers. They prolong cardiac action potential duration (increased QT interval on the ECG), and prolong the effective refractory period (see Fig. 2.3).
Class IV
Examples of class IV drugs include verapamil and diltiazem (see Fig. 2.3 and Fig. 2.6).
Details of the drugs are given in the section on antianginal drugs (p. 28).
Antianginal drugs
Acute attacks of angina are treated with:
In the hospital setting, acute anginal pain is treated with an opiate (Ch. 9).
Stable angina is treated with:
β-Adrenoceptor antagonists (β-blockers)
Examples of β-blockers include propranolol, atenolol, bisoprolol and metoprolol.
Mechanism of action
The aim of using β-adrenoceptor antagonists in cardiac disease is to block β-adrenoceptors in the heart. This has the effect of causing a fall in heart rate (slowing of phase 4; Fig. 2.4), in systolic blood pressure, in cardiac contractile activity and in myocardial oxygen demand.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree