Cardiovascular Physiology
ANATOMIC CONSIDERATIONS
How do arteries and veins differ in regard to the following?
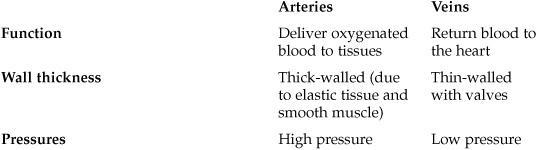
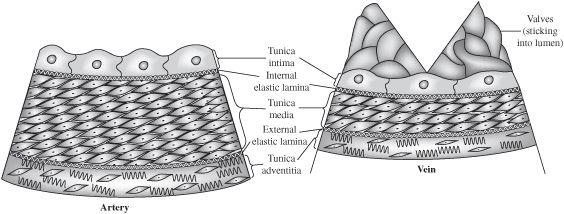
Figure 3.1 Arteries and veins: a structural comparison.
How does the heart receive its own blood flow?
The coronary arteries; they branch off in the first centimeter of the aorta
What is compliance?
Compliance describes the distensibility of a given structure
What is the formula for compliance? (Note: Compliance = Capacitance)

C = Compliance
V = Volume
P = Pressure
Which has a higher compliance, arteries or veins?
Veins
Which contains the larger proportion of blood, arteries or veins?
Veins contain a higher proportion of total blood volume; this is the unstressed volume, a reservoir that can be mobilized in times of need.
The wall of the aorta has one of the highest concentrations of elastin. What does this elastin do for circulation?
It facilitates the Windkessel effect; the heart pushes blood out into the low compliance aorta, which balloons slightly; subsequently, the elastin allows the aorta to force the blood forward into the systemic circulation
What is unique about the capillary bed of the vasculature? Why is that important?
It has the largest cross-sectional area and surface area, which allows for the efficient exchange of nutrients, water, and gases
What is unique about the pulmonary vasculature compared to the systemic vasculature?
Hypoxia causes vasoconstriction of the pulmonary vasculature. In most organs hypoxia causes vasodilation.
What is the effect of pulmonary hypoxic vasoconstriction?
It shunts blood toward lung segments that are being effectively ventilated
How does flow in the pulmonary circulation relate to flow in the systemic circulation?
They must be equal! While the total amount of blood in each circuit varies at any given time, total flow per unit time through each circuit must be equal.
HEMODYNAMICS
How do we calculate flow? Can we generalize that equation to the whole systemic circuit?

Q = flow
P = change in pressure
RT = total resistance
CO = cardiac output
MAP = mean arterial pressure
PRA = right atrial pressure
TPR = total peripheral resistance
How does increasing the pressure gradient influence flow through the circuit?
Increases the flow
What is Poiseuille equation for resistance?

R = resistance
η = viscosity of blood
l = vessel length
r= vessel radius
What happens to the resistance if the radius of the blood vessel is reduced by 50%?
Increased by a factor of 16
(R ∝ [1/r4] so 1/[½]4 = 16)
How is resistance regulated physiologically?
Through the autonomic nervous system which modulates the tone of vascular smooth muscle to change vessel radius
Which component of the vascular system is the site of the highest resistance?
The arterioles; these have the greatest ability to change their radius, and, therefore, their resistance
What factors change the resistance of the vasculature system proportionally?
Viscosity and length of the vessel
What is the major determinant of viscosity in the vascular system?
The hematocrit is mostly responsible for the viscosity within the vascular system
In what pathologic states does viscosity increase?
Polycythemia
Hyperproteinemia
Hereditary spherocytosis
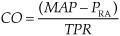
Poiseuille law gives us the resistance for a given vessel segment. What are the equations for summing the resistance of vascular segments in series? In parallel?
Series:
RT = R1 + R2 + R3….etc.
Parallel:
RT = total resistance
Rx = resistance of segment x
On which arterioles are α1-adrenergic receptors found?
Skin
Renal circulation
Splanchnic circulation
On which arterioles are β2-adrenergic receptors found?
Skeletal muscle
What is the significance of this variation in receptor expression?
By increasing resistance in nonessential circuits, we can shunt blood to vital systems during times of need (stress)
What is the equation for the velocity of blood flow?

v = velocity of blood flow (cm/s)
Q = volume of blood flow (mL/s)
A = cross-sectional area (cm2)
Why is velocity of blood flow in the aorta higher than that of the capillaries?
Velocity of blood flow is inversely proportional to cross-sectional area; the aorta has a relatively small cross-sectional area compared to that of the sum of all the capillaries
When is the systolic pressure measured?
At the peak of cardiac contraction
When is diastolic pressure measured?
At the nadir of cardiac relaxation
How can you calculate the pulse pressure?
Pulse pressure = systolic – diastolic
What is the major determinant of pulse pressure (PP)?
Stroke volume (SV), rising SV leads to a higher PP
What happens to the pulse pressure when the compliance decreases?
Increases (think: atherosclerosis)
What is the mean arterial pressure (MAP)?
Average arterial pressure with respect to time
MAP = CO × TPR or
MAP = 1/3(systolic) + 2/3(diastolic)
CO = cardiac output
TPR = total peripheral resistance
Which is lower, venous pressure or right atrial pressure?
Atrial pressure; recall that pressure drives blood flow
What is meant by laminar flow?
The movement of fluid through vessels in an organized way (think: water in a garden hose)
What is turbulent flow?
Fluid movement that is disorganized (think: white water rapids)
What can we use to predict if flow will be laminar?
Reynolds number; it is useful as an index of turbulence
Physiologic variation in what parameter most influences the Reynolds number?
Viscosity (anemia reduces viscosity, polycythemia would increase it, etc)
ELECTROPHYSIOLOGY—CARDIAC ACTION POTENTIAL
What is cardiac excitability?
The ability of the cardiac muscle cells to conduct an action potential after being depolarized by an inward current
Conductance of what ion determines the resting membrane potential in cardiac muscle cells?
Like all other excitable cells, conductance to K+
What is the resting membrane potential of nonpacemaker cardiac myocytes?
~90 mV, which is close to the K+ equilibrium potential
What maintains the resting membrane potential?
Na+-K+ -ATPase membrane protein
Again, what does it mean when a membrane depolarizes?
There is an inward current that brings positive charge into the cell
What does it mean when a membrane hyperpolarizes or repolarizes?
There is an outward current that removes positive charge from the cell
In the diagram of cardiac action potential below, label all of its phases and the currents that are responsible for them.
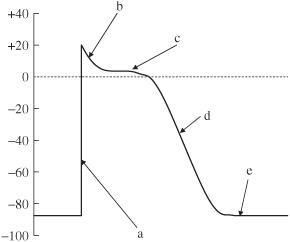
Figure 3.2 Cardiac action potential.
Describe what happens during each of the following phases of a cardiac action potential:
Phase 0
Upstroke: caused by a rapid transient increase in Na+ conductance, which allows an inward Na+ current to depolarize the membrane (INa)
Phase 1
Brief initial repolarization: caused by a decrease in inward Na+ current due to closure of voltage-activated Na+ channels
Phase 2
Plateau phase: caused by an increase in Ca2+ conductance and K+ conductance continues to increase; this phase is marked by a net electrical balance between inward Ca+ (ICa) and outward K+ currents (IKout)
Phase 3
Repolarization: K+ conductance peaks. The Ca+ conductance decreases; the electrical balance now favors the large outward K+ current (IKout)
Phase 4
Resting membrane potential: caused by an equilibrium between outward and inward ionic currents
All of these channels are triggered by what?
Threshold; the moment that threshold is reached, the sequence of cardiac conductance is set in motion.
What determines the peak of the cardiac action potential?
Conductance to Na+
ELECTROPHYSIOLOGY—ELECTROCARDIOGRAM
Identify the labeled parts and intervals of the electrocardiogram (ECG) below.
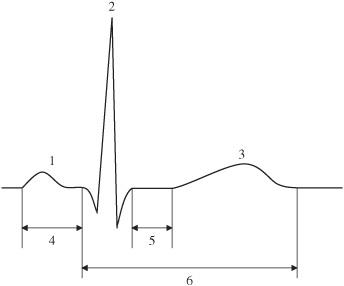
Figure 3.3 ECG.
- P wave
- QRS complex
- T wave
- PR interval
- ST segment
- QT interval
Define what the following waves/complexes from the ECG represent:
P wave
Atrial depolarization
PR interval
Conduction through the AV node
QRS complex
Conduction through the myocardium
QT interval
Mechanical contraction of the ventricle
T wave
Ventricular repolarization
How long does the PR interval last?
0.12 to 0.2 seconds (normally)
How long does the QRS complex last?
0.12 seconds (normally)
When does atrial repolarization occur?
During the QRS complex; it is not seen on the ECG because it is masked by the much greater electrical activity in the ventricle
What are the ECG changes associated with the following types of heart blocks?
1° (first degree)
PR interval > 0.20
2° (second degree) Mobitz type 1
PR intervals progressively increase from beat to beat until a beat is dropped
2° (second degree) Mobitz type 2
PR interval > 0.20 at a fixed interval with a fixed ratio of dropped beats
3° (third degree)
P waves (atrial contraction) and QRS complexes (ventricular contractions) are unrelated. Also called “complete heart block”
What are the ECG changes associated with the following abnormal rhythms?
Atrial fibrillation
No discernible P waves, irregularly spaced QRS complexes with an irregularly undulating baseline
Atrial flutter
“Sawtooth” baseline
Ventricular fibrillation
Completely abnormal rhythm that has no recognizable waves or complexes
ELECTROPHYSIOLOGY—PACEMAKER POTENTIAL
Where do pacemaker potentials occur normally?
- Sinoatrial (SA) node
- Atrioventricular (AV) node
- His-Purkinje systems
What is the normal pacemaker of the heart?
The SA node
What is the normal pacing rate of the SA node?
60 to 100 potentials/min
What are the latent pacemakers in the heart?
AV node and His-Purkinje system
When might latent pacemakers take over for the main pacemaker?
Either when the SA node is suppressed or if conduction is blocked
What are the average pacing rates of the AV node and His-Purkinje system?
Average pacing rates are 45 and 30 beats/min, respectively
What is unique about the pacemaker action potential?
It has an unstable resting potential that exhibits slow phase 4 depolarization; this steady depolarization leads to repetitive cycles of action potential propagation
What phases are not present in the pacemaker potential?
Phases 1 and 2 are not present
On the cardiac pacemaker potential figure below, label all of its phases and the currents that are responsible for them.
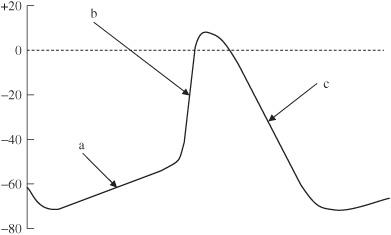
Figure 3.4 Cardiac pacemaker potential.
Describe what happens during each of the following phases of the pacemaker potential:
Phase 4
Slow depolarization: caused by a steady Na+ conductance along with some Ca2+ conductance (If)
Phase 0
Upstroke: caused by an increase in Ca+ conductance, which allows an inward Ca+ current to depolarize the membrane toward the Ca+ equilibrium potential (ICa)
Phase 3
Repolarization: caused by an increase in K+ conductance resulting in an outward K+ current (IK)
What is the name of the current that accounts for pacemaker activity?
Although it is predominately a Na+ current, we call it If, the funny current
What turns on the current that accounts for the pacemaker activity?
Membrane repolarization leads to activation of If
ELECTROPHYSIOLOGY—CONDUCTION AND EXCITABILITY
What is conduction velocity?
The rate at which an electrical impulse propagates through cardiac tissue
Describe the anatomical flow of electrical propagation in the heart:
SA node generates an AP, this flows through the right atria (and to the left atria via Bachmann bundle) to the AV node. There it is delayed briefly before flowing through the His-Purkinje system into both ventricles concurrently.
What does conduction velocity depend on?
The magnitude of the inward current due to the influx of ions during phase 0 of the cardiac action potential
Where is conduction velocity the fastest?
Purkinje system
Where is conduction velocity the slowest?
AV node
What does the difference in conduction time between the AV node and the Purkinje system allow the heart to do?
The delay allows the ventricle to fill completely by accepting the “atrial kick”
What can happen if conduction velocity through the AV node is increased?
Ventricular filling can be compromised
What is a dromotropic effect?
A change in conduction velocity through a nerve fiber. When talking about the heart, we mean conduction through the AV node with changes in the PR interval
What type of dromotropic effect does the sympathetic nervous system produce?
Positive dromotropic effect (shortening of the PR interval)
Sympathetic stimulation of the heart utilizes what receptor? What is the neurotransmitter used?
β1 receptor; norepinephrine (NE) is the neurotransmitter
How does the sympathetic nervous system produce its dromotropic effect?
By increasing the inward Ca2+ current during phase 4, this increase shortens the PR interval, thereby increasing the overall heart rate
What type of dromotropic effect does the parasympathetic nervous system produce?
Negative dromotropic effect (lengthening of the PR interval)
Parasympathetic stimulation of the heart utilizes what receptor? What is the neurotransmitter used?
Muscarinic receptor; acetylcholine (ACh) is the neurotransmitter
How does the parasympathetic system produce its dromotropic effect?
It decreases the inward Ca2+ current and increases the outward K+ current; this decreased conduction velocity increases the PR interval, slowing the heart rate
How does dromotropy differ from chronotropy?
They are intimately related, but chronotropy refers specifically to heart rate as determined by the SA node; dromotropy more specifically refers to AV nodal conduction
Diagram and identify the following elements of a cardiac action potential.
Absolute refractory period (ARP)
Effective refractory period (ERP)
Relative refractory period (RRP)
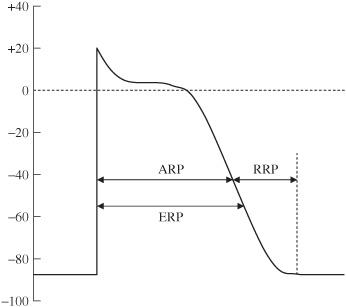
Figure 3.5 Refractory period relationships.
The time during which no number of entering impulses can initiate a new action potential
What is the ERP?
The time during which no conducted action potential can be produced
What is RRP?
The time during which an action potential can be initiated, but requires a larger depolarizing stimulus
What is the starting and ending point of the following refractory periods?
ARP
Starts with the upstroke and ends after the plateau
ERP
Starts with the upstroke and ends slightly after the ARP
RRP
Starts right after the ARP and lasts until repolarization is complete
CARDIAC MUSCLE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


