Summary by Shaojie Han, MD, MS, and Rashi Aggarwal, MD
73
Based on “Principles of Addiction Medicine” Chapter by Steven Pfau, MD, and Howard S. Friedman, MD
The most common heart diseases in Western society—hypertension, coronary artery disease (CAD), atrial fibrillation (AFib), heart failure, and stroke—have important associations with the use of alcohol and other drugs. Treatment of cardiac conditions requires recognition and treatment for addiction and vice versa.
ALCOHOL
The manifestations of alcohol-related heart disease depend in large part on the amount of alcohol ingested and the time period of exposure. Alcohol use of more than 14 drinks per week in men and 7 drinks per week in women is considered heavy use.
Cardiac output usually increases even after small amounts of alcohol ingestion in healthy subjects, reflecting the changes in heart rate and peripheral resistance that ensue. By contrast, a left ventricular (LV) ejection fraction, a more sensitive index of cardiac function, generally declines during alcohol use. Acute myocardial depression is due to intracellular acidosis, reduction in action potential, and suppression in calcium activation. Chronic cardiac dysfunction may result from activation of the renin–angiotensin system.
Alcoholic Cardiomyopathy
In Western societies, alcoholic myopathy is the second leading cause of secondary dilated cardiomyopathies after ischemia. Worldwide, as many as one third to one half of cases of dilated cardiomyopathy may be attributable to alcohol use. The likelihood of developing clinical cardiomyopathy correlates with daily alcohol intake and duration of drinking and is independent of a patient’s nutritional status. Chronic heavy alcohol users begin to manifest cardiac abnormalities before clinical symptoms arise: Increased wall thickness, LV mass, and LV volumes may be observed before a decrease in ejection fraction is noted.
To establish the diagnosis of alcoholic cardiomyopathy, a history of chronic and prolonged alcohol use, usually 80 to 90 g of alcohol daily for at least 5 years, is of primary importance. Ischemic cardiomyopathy must be excluded. A history of prior myocardial infarction (MI), chest discomfort, or evidence of ischemia and/or MI on the electrocardiogram favors a diagnosis of ischemic cardiomyopathy. Other causes of dilated cardiomyopathy to be considered are toxin exposure (especially chemotherapy, lead, and mercury), familial/genetic myopathies, prolonged arrhythmias, and viral infections. Cardiac imaging (e.g., cardiac MRI and echocardiogram) and functional studies are helpful for the differential diagnosis. Four-chamber enlargement is the typical echocardiographic appearance of an alcoholic cardiomyopathy, with either normal or increased wall thickness. When detected early and treated aggressively with alcohol abstinence and standard medical therapy, its prognosis may be better than that of other dilated myopathies. However, without complete abstinence, the 4-year mortality approaches 50%.
Hypertension
Alcohol use, especially in moderate-to-heavy amounts, is associated with hypertension. Alcohol raises blood pressure through direct sympathetic vasomotor effects and secondary mechanisms, such as worsened sleep apnea. Alcohol and its metabolites, acetaldehyde and acetate, have both direct vasodilatory effects and sympathetic vasoconstrictive effects. Corticotrophin-releasing hormone possibly participates in the acute hypertensive effects of alcohol. Alcohol also impairs the baroreceptor reflex, and the subsequent activation effect on the renin–angiotensin system may persist even after 4 weeks of abstinence.
The degree of blood pressure increased by alcohol is dose dependent. Although there is some debate regarding possible cardiovascular benefits of alcohol, the hypertensive effects are consistent. Alcohol can be an important factor when hypertension is refractory to standard treatment. Reduction of alcohol consumption is associated with significant decreases in blood pressure noted in the treatment of hypertension.
Atrial Fibrillation
AFib is the most common clinical arrhythmia in adults, with a lifetime risk of one in four for people over the age of 40. Risk factors other than age are hypertensive heart disease, coronary heart disease, and heavy alcohol use. The occurrence of AFib in the context of alcohol use must be considered as a potential harbinger of significant heart disease and must be evaluated in the same manner as new-onset AFib occurring in any other context. EKG, echocardiogram, and blood tests for renal, thyroid, and liver function are all recommended in the initial workup.
Coronary Artery Disease and Stroke
Low-to-moderate alcohol consumption appears to have a protective effect on CAD and stroke. In patients with CAD, both cardiovascular mortality and all-cause mortality are lower with low-to-moderate alcohol intake, with a dose–response curve indicating benefit at ranges from 5 to 26 g/day of alcohol intake. Similarly, low amounts of alcohol intake may be associated with lower risks in congestive heart failure and MI, as well as favorable metabolic profiles in lipid and insulin sensitivity. The particular advantage to red wine over other forms of alcohol is that the presence of polyphenols, tannins, and flavonoids adds favorable effects. However, it should be noted that the evidence of the beneficial effect of alcohol has been debated, particularly since the epidemiologic data suffer the potential bias of self-reporting of alcohol intake and randomized controlled data are scarce.
Heavy alcohol use has been consistently linked with an increase in CAD. In heavy alcohol users, progressive increases in coronary calcification can be noted on computed tomography over 2 to 4 years. Coronary calcification as a marker for coronary atherosclerosis is not correlated with incident coronary events in heavy alcohol users, which suggests mechanisms other than atherosclerosis are involved.
At any level of consumption, alcohol is associated with a lower risk of ischemic stroke and a higher risk of hemorrhagic stroke, which may be explained by the antithrombotic properties of alcohol. Heavy alcohol use consistently increases the relative risk of total strokes (either ischemic or hemorrhagic).
NICOTINE
While nicotine has direct and immediate effects on the cardiovascular system, the specific role of nicotine in cigarette-related heart disease is still debated. Within minutes of a dose, nicotine promotes the release of norepinephrine from nerve terminals and the release of epinephrine from the adrenal medulla. As a result, heart rate and blood pressure both increase. Smoking also attenuates baroreceptor responses to blood pressure elevations. Tolerance to these physiologic effects develops rapidly.
Nicotine use, both acute and chronic, has been implicated as a risk for cardiac arrhythmias, especially AFib in animal studies. However, studies in patients with cardiac disease did not show any increased arrhythmias with patients on nicotine replacement therapy. There are likely net benefits and decrease in overall arrhythmic events when nicotine administration replaces traditional cigarette smoking, even though nicotine may be itself proarrhythmic to otherwise healthy hearts.
Clinical manifestations of atherosclerosis often are the result of both atherogenesis and atherothrombosis. The role of nicotine in both processes is much smaller than that of other components of cigarette smoke. Endothelial injury and dysfunction occurs early in smokers, with impairment in nitric oxide production and endothelium-dependent vasodilatation. Chronic smoking alters normal platelet function, which increases aggregation. Elevated fibrinogen in smokers is an acquired risk factor for cardiovascular diseases. Particulate matter inhalation has also been demonstrated to be proinflammatory and contribute to atherogenesis.
In a given individual, smoking cessation is associated with a rapid decline in the risk for acute MI, approaching the level of a nonsmoker after 2 to 3 years. Mandatory smoking prohibition programs have repeatedly been related to decreased hospitalization rates for acute MI.
COCAINE
Chest pain, acute MI, aortic dissection, stroke, heart failure, and sudden cardiac death have all been associated with acute and chronic cocaine abuse. Cocaine has potent sympathomimetic actions. The adrenergic effects are the result of blocking presynaptic norepinephrine and dopamine reuptake, thereby making more catecholamines available at postsynaptic receptors and stimulating the sympathetic nervous system. Acute hemodynamic effects of cocaine administration are elevation in heart rate and blood pressure. Cocaine-induced vasoconstriction may be accentuated by the presence of atherosclerosis and cigarette smoking. Cocaine also suppresses cardiac contractility by inhibiting transmembrane sodium flux and sodium–calcium exchange.
Cocaine affects all components of hemostasis, such as causing platelets–endothelial dysfunction and increasing the level of fibrinogen and von Willebrand factor. Although some evidence suggested that cocaine use accelerates the atherosclerotic process, it is difficult to separate cocaine from other major environmental, genetic, and behavioral factors.
In general, cardiovascular symptoms occur early after cocaine use, with a markedly elevated risk of cocaine-associated MI within the first 24 hours. Cocaine-related chest pain is the most frequent cardiovascular presentation associated with cocaine use. However, the incidence of acute MI in patients presenting to ERs with cocaine-associated chest pain is actually relatively low (0.7% to 6%). The most recent ACC/AHA guidelines for the evaluation of unstable angina state that in the absence of other high-risk features, a history of cocaine use is associated with a lower risk of MI. Still, as the demographic of cocaine shifts to an older population who themselves have a higher proportion of other CAD risk factors, the diagnosis of MI must be considered carefully. A series of troponin measurements has high sensitivity and specificity. Benzodiazepine and nitroglycerin have been shown to alleviate acute chest pain symptoms.
When acute MI in the context of cocaine abuse does occur, the treatment approach differs from non-cocaine–associated infarction in several important aspects. Antiplatelet therapy with aspirin or P2Y12 inhibitors seems to be beneficial. Without a combination with an alpha-blocker, β-adrenergic receptor blockers are not recommended to address cocaine-related chest pain because unopposed alpha-receptor stimulation precipitates arterial vasoconstriction. More recent data suggest that this may not be as concerning as previously thought, but recent practice guidelines still do not endorse beta-blockers in early management of cocaine-related chest pain. Evidences seem to favor the use of thrombolytics for reperfusion therapy in cocaine-related ST segment elevation MI. Unfortunately, this has never been tested formally. Similarly, primary angioplasty with stenting has improved MI outcomes, but cocaine use increases the risk of stent thrombosis.
Aortic dissection and stroke are also related to cocaine use. Cocaine-related dissection tends to occur more frequently in young, hypertensive subjects. Both ischemic and hemorrhagic strokes have been reported with approximately equal frequency in cocaine users. Hemorrhage appears to be more frequent in current users, while ischemic stroke and transient ischemic attack are more common in remote cocaine users. Large artery atherosclerotic disease is the most common finding in ischemic stroke, consistent with the hypothesis that cocaine use accelerates atherosclerosis.
OPIOIDS
From a strictly cardiovascular perspective, opioids have significant medicinal value. The hemodynamic effects of lowering heart rate and blood pressure, as well as decreasing preload, combined with their analgesic and anxiolytic properties, have made morphine a cornerstone of the treatment of MI and acute pulmonary edema. The primary cardiovascular risk of opioid use is associated with the intravenous route of administration. Right-sided valvular disease (typically the tricuspid valve) is much more likely to be associated with injection drug use. Polymicrobial or fungal endocarditis, which carries higher mortality, is also more common. Patients with opioid use disorders are at risk for repeated episodes of endocarditis.
AMPHETAMINES
Amphetamines are a group of synthetic compounds used both recreationally and medicinally. Amphetamines and their derivatives are used in the treatment of attention deficit hyperactivity disorder and traumatic brain injury. Many amphetamines are abused recreationally and include 3,4-methylenedioxymethamphetamine (MDMA or “ecstasy”) and methylenedioxyethylamphetamine (MDEA or “eve”). Amphetamines produce a dose-dependent elevation of blood pressure and an increase of heart rate. The magnitude of the changes reflects their α1-adrenergic (elevate blood pressure with reflex slowing of heart rate) and β1-adrenergic (enhance cardiac contractility and increase heart rate) effects. The blood pressure elevations dissipate over 3 to 4 hours, while the tachycardia can persist for as much as 10 hours.
Amphetamines are reported to be associated with acute MI and may be associated with a worse prognosis in those with acute coronary syndrome. Similarly, ischemic and hemorrhagic stroke have been associated with amphetamine use. Phenylpropanolamine, an appetite suppressant, was removed from over-the-counter sale by the FDA because of a strong association with a risk for hemorrhagic stroke, especially in young women. Some amphetamine derivatives (e.g., fenfluramine as appetite suppressants) are strong serotonin receptor (especially 5-HT2B receptor) agonists and were also removed from the market after these showed evidence for the development of a valvular heart disease similar to a complication of serotonin-secreting carcinoid tumors. Similar lesions have been described in recreational amphetamine use.
Cardiomyopathy is perhaps the most commonly associated heart disease in chronic amphetamine use. Chronic stimulant users account for as many as 5% of all patients presenting to ERs in the United States with decompensated heart failure. Concentric hypertrophy is a common finding in methamphetamine users and may precede the development of heart failure.
CANNABIS
Cannabis increases heart rate and cardiac output. The effects on the cardiovascular system are likely mediated through sympathetic activation. At least two types of cannabis receptors have been identified (CB1 and CB2) and exist in a variety of tissues related to atherosclerosis. However, stimulation of these receptors could be protecting from atherosclerosis or promoting atherosclerosis. Most data are suggesting proatherogenic effects from CB1 agonists and antiatherogenic effects from CB2 agonists. Summaries of the association of marijuana and MI rely heavily on case reports. Scarce data limit the accuracy in determining the cardiovascular risk from cannabis. Major cardiovascular effects of alcohol and other drugs are listed in Table 73-1.
TABLE 73-1. SALIENT CARDIOVASCULAR EFFECTS OF ALCOHOL AND OTHER DRUGS
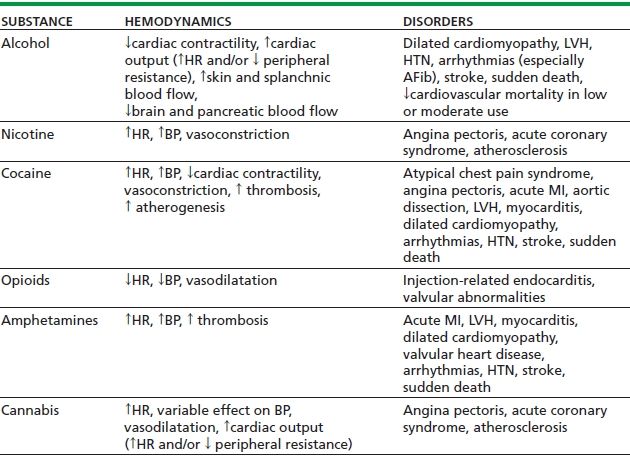
LVH, left ventricular hypertrophy; HTN, hypertension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


