12 Cancer
Concepts of cancer chemotherapy
Chemotherapy
The chemotherapeutic techniques currently used include:
A diagnosis of cancer carries a significant social and emotional impact. Hair loss and sickness are more often the initial concern for patients, rather than other potentially serious side-effects of chemotherapy. Nausea and vomiting should be taken seriously in cancer management, as these can have a devastating impact on quality of life; antiemetic drugs are discussed in Chapter 8.
Cytotoxic chemotherapy
Mechanisms of action
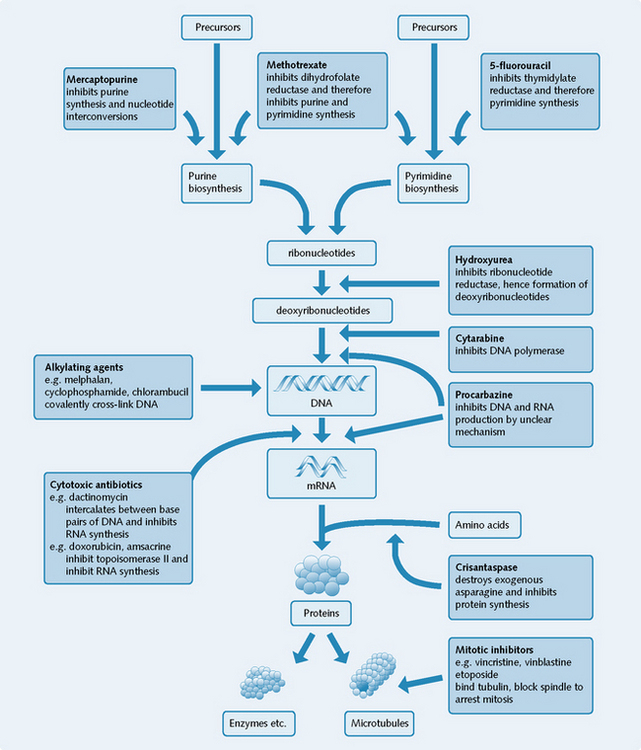
Most cytotoxic drugs affect DNA synthesis. They can be classified according to their site of action on the process of DNA synthesis within the cancer cell (Fig. 12.1). Cytotoxic drugs are therefore most active against actively cycling/proliferating cells, both normal and malignant, and least active against non-dividing cells.
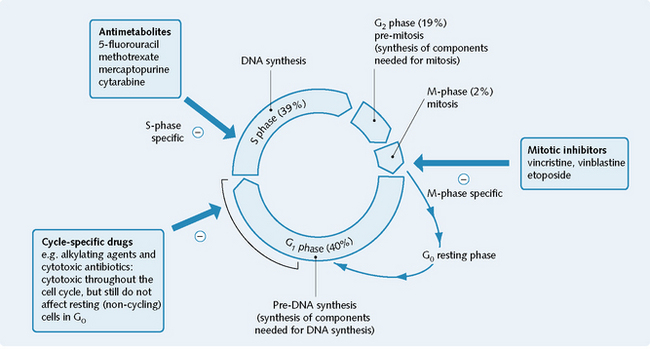
Some drugs are only effective at killing cycling cells during specific parts of the cell cycle. These are known as phase-specific drugs (Fig. 12.2). Other drugs are cytotoxic towards cycling cells throughout the cell cycle (e.g. alkylating agents) and are known as cycle-specific drugs.
Selectivity
Cytotoxic drugs affect all dividing tissues, both normal and malignant, and thus are likely to have general toxic side-effects (see Fig. 12.4). The side-effects of cytotoxic drugs are most often related to the inhibition of division of non-cancerous host cells, namely in the gut, in the bone marrow and in the reproductive and immune systems.
Relative selectivity can occur with some cancers because:
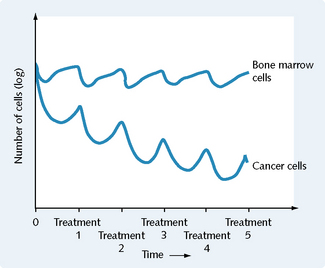
Knowledge of these principles and knowing that cytotoxic drugs kill a constant fraction, not a constant number, of cells, lays down the foundation for chemotherapeutic dosing schedules (Fig. 12.3).
Mechanisms of genetic resistance to cytotoxic drugs
The mechanisms of genetic resistance to cytotoxic drugs include:
Cytotoxic agents
Cytotoxic agents, the major group of anticancer drugs, include the:
Alkylating agents
Examples of alkylating agents include melphalan, cyclophosphamide and chlorambucil.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree