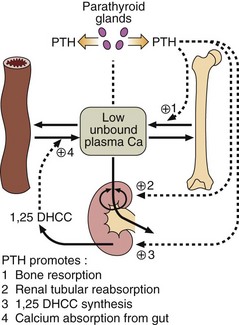
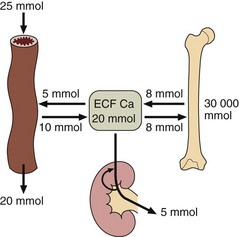
35 The amount of calcium present in the extracellular fluid is very small in comparison to that stored in bone. Even in the adult, calcium in bone is not static; some bone is resorbed each day and the calcium returned to the ECF. To maintain calcium balance, an equal amount of bone formation must take place. Figure 35.1 shows how much calcium is exchanged between one compartment and another daily. Fig 35.1 Normal calcium balance. Calcium is exchanged each day, in the amounts shown, between the extracellular fluid and the gut, bone and kidney. Calcium homeostasis is modulated by hormones (Fig 35.2). Parathyroid hormone (PTH), which consists of 84 amino acids, is secreted from the parathyroid glands in response to a low unbound plasma calcium. PTH causes bone resorption and promotes calcium reabsorption in the renal tubules, preventing loss in the urine. 1,25-dihydroxycholecalciferol (1,25 DHCC) maintains intestinal calcium absorption. This sterol hormone is formed from vitamin D (cholecalciferol), following hydroxylation in the liver (at carbon-25) and kidney (at carbon-1). However, hydroxylation in the kidney is PTH dependent, and so even the absorption of calcium from the gut relies (albeit indirectly) on PTH. Laboratories routinely measure total calcium concentration (that is both the bound and unbound fractions) in a serum sample. However, this may give rise to problems in the interpretation of results because changes in serum albumin concentration cause changes in total calcium concentration. If albumin concentration falls, total serum calcium is low because the bound fraction is decreased (Fig 35.3
Calcium regulation and hypocalcaemia
Calcium homeostasis
Serum calcium
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine