FIGURE 25.1 Sinus bradycardia with a left bundle branch block pattern.
EXPERT OPINION
This is a worrisome history. Sudden syncope associated with an injury, especially in the setting of structural heart disease, implies an abrupt drop in blood pressure with subsequent cerebral hypoperfusion and loss of consciousness. The evaluation should be based on the assumption that the mechanism is a malignant dysrhythmia.
• Differential: Ventricular tachycardia (VT); findings from the ECG suggests sinus node disease, infra-Hisian conduction block.
• Neurological etiologies and vasodepressor mechanisms of syncope are unlikely in the absence of prior neurologic disease or symptoms of vagal discharge.
• Evaluation: Electrophysiology study (EPS) to evaluate for a mechanism of syncope. Since the accuracy of electrophysiology testing in the setting of a nonischemic cardiomyopathy is low, if the EPS does not reveal the etiology of syncope, there should be a consideration for empiric implantation of a defibrillator (ICD).
PATHOPHYSIOLOGY AND MANAGEMENT
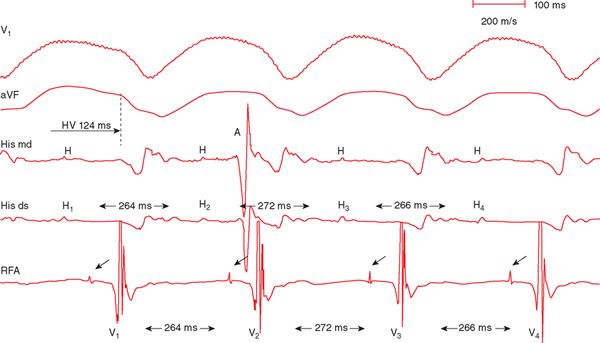
At EPS, VT was reproducibly induced with programmed stimulation of the ventricle. The tracing (Figure 25-2) shows surface leads V1 and aVF and intracardiac tracings from the His catheter and the radiofrequency ablation (RFA) catheter, positioned at the right bundle. The mechanism of the tachycardia is bundle branch reentrant ventricular tachycardia (BBR-VT). The hallmark features are:
FIGURE 25.2 Surface and intracardiac tracing during induced sustained bundle branch reentry VT.
• VA dissociation. The single atrial beat is marked with an A on the His mid electrode.
• QRS morphology during the VT is identical to the QRS morphology of the patient’s native LBBB during sinus rhythm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree