FIGURE 6-1
(A) Absence of myoepithelial cells on immunohistochemical staining
(B) Angular-shaped glands with open lumens
(C) Desmoplastic, cellular stroma
(D) Minimal cytologic atypia
(E) Peripheral lobular architecture around a central scar
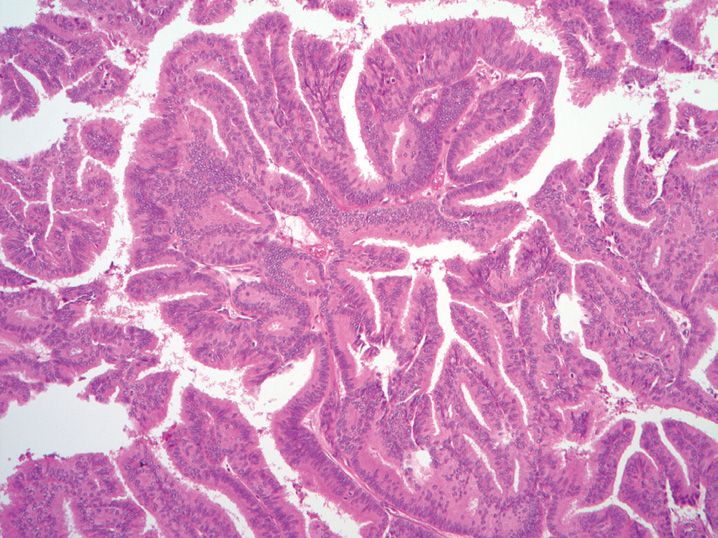
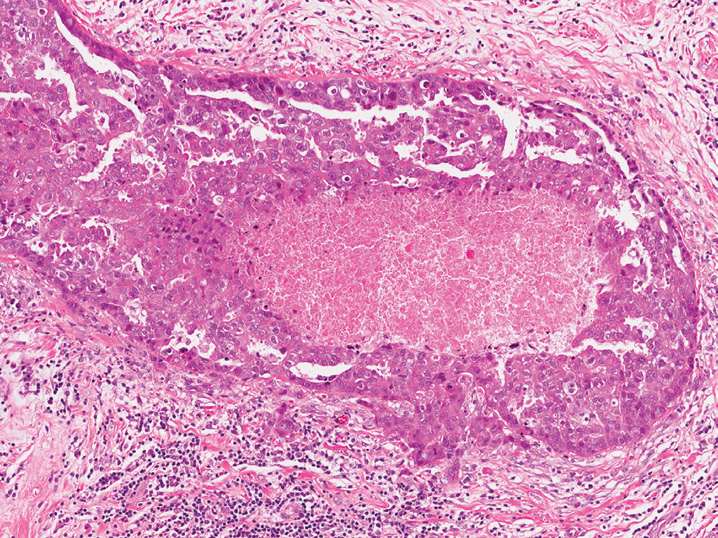
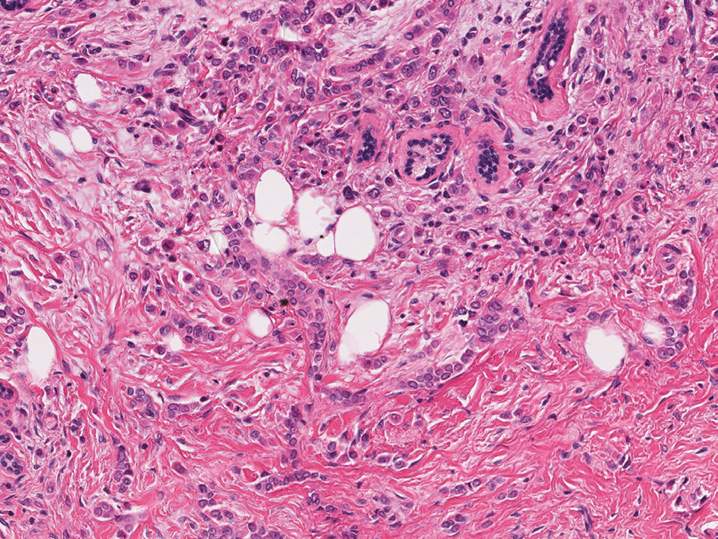
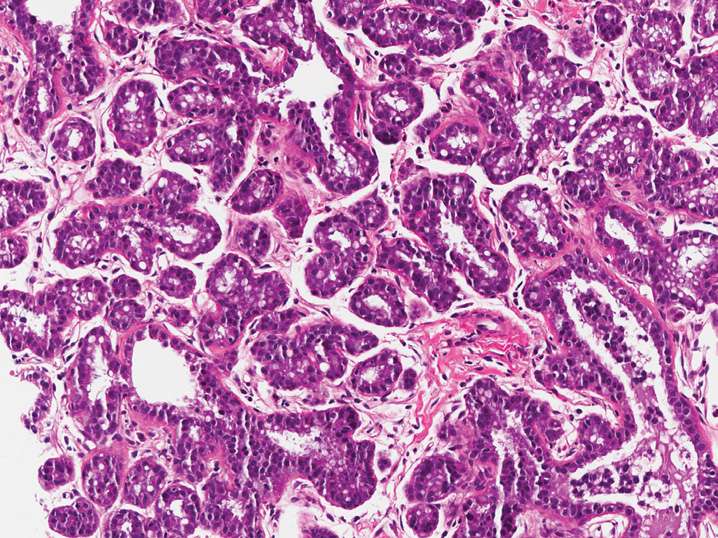
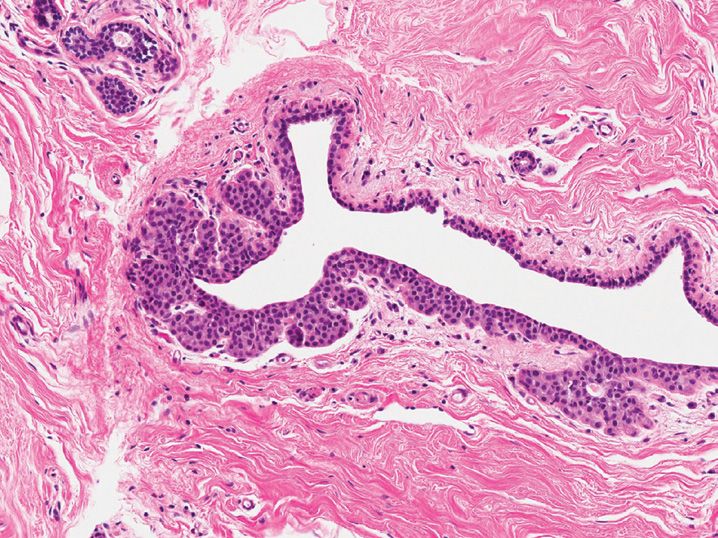
2. A 47-year-old woman has a breast biopsy, which shows the following change within a large duct (see Figure 6-2). Which of the following statements regarding this process is accurate?
(A) Excision is not required
(B) Fibrovascular cores are well developed and thick
(C) Immunohistochemical staining for myoepithelial cells will be negative
(D) Most patients present with a nipple discharge
(E) Usual-type epithelial hyperplasia is common
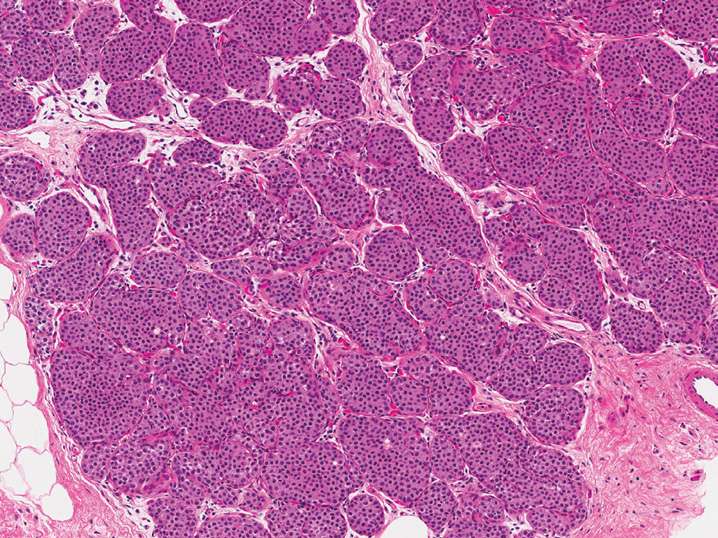
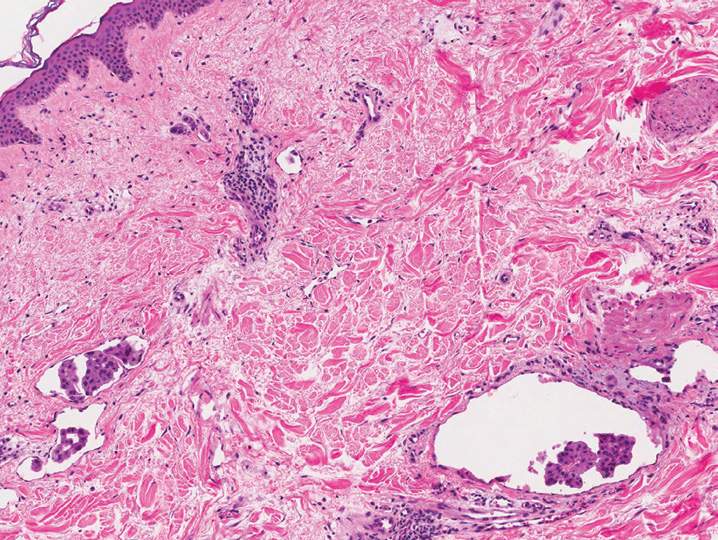
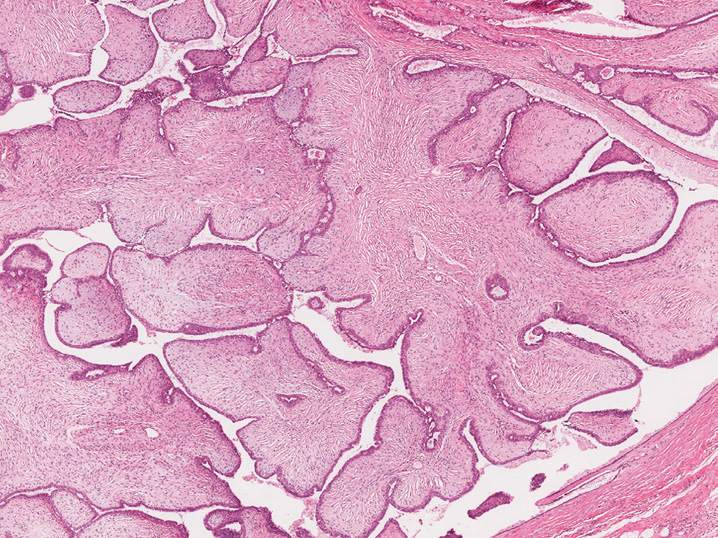
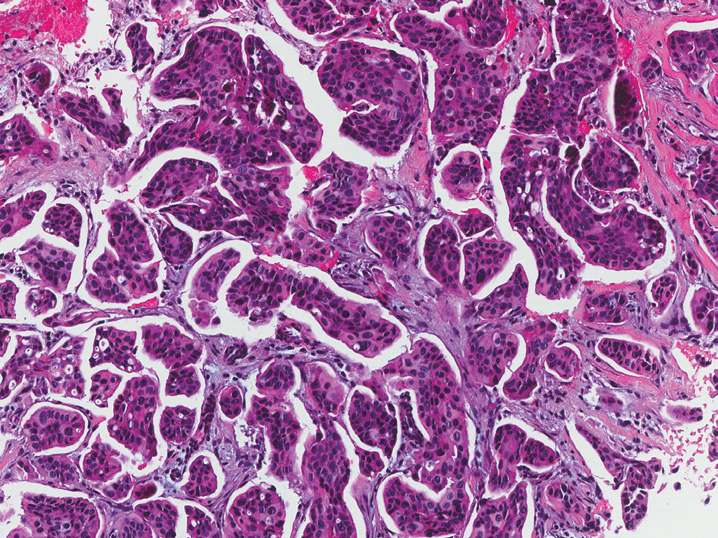
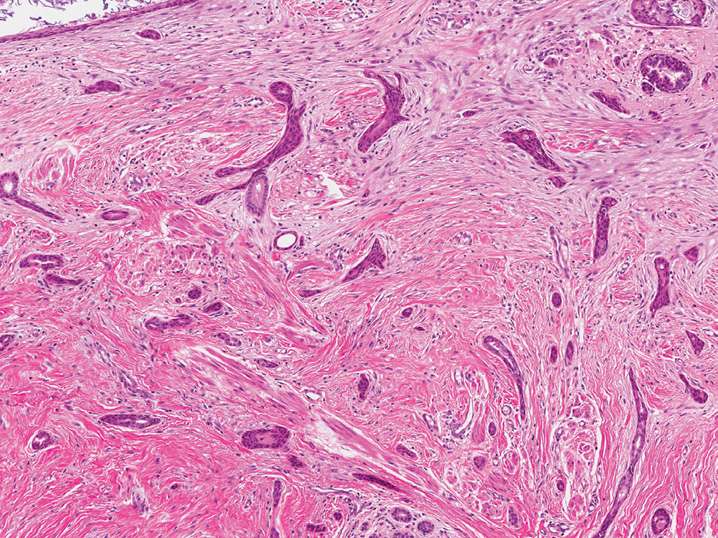
3. A 61-year-old woman has a breast biopsy (see Figure 6-3). Which of the following features would favor an interpretation of usual ductal hyperplasia rather than low-grade ductal carcinoma in situ?
(A) Attenuated or incomplete myoepithelial layer
(B) Distinct epithelial cell margins
(C) Nuclei parallel to the direction of the epithelial bridge
(D) Rounded spaces within the epithelial proliferation
(E) Spaces evenly distributed throughout the epithelial proliferation
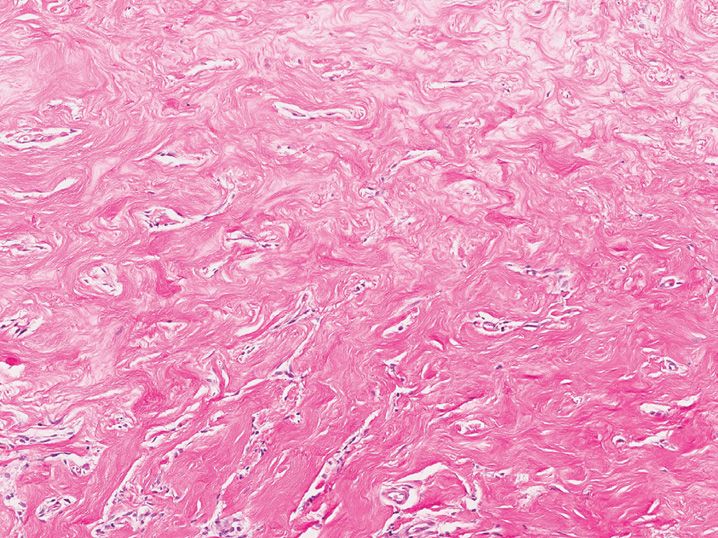
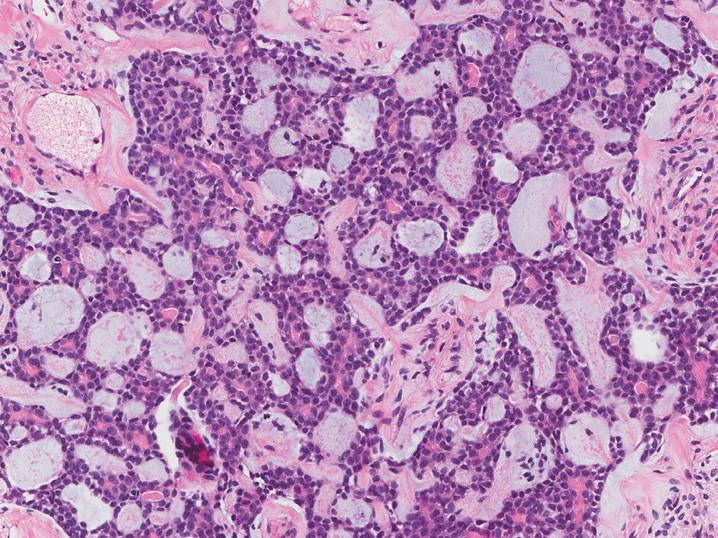
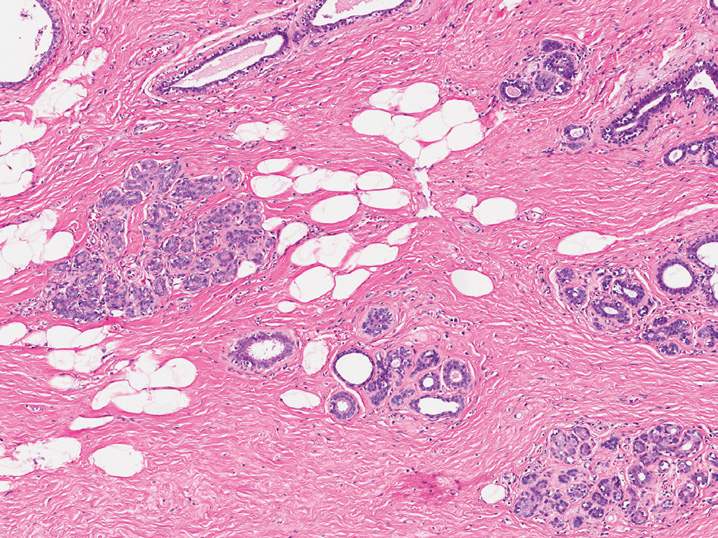
4. A 43-year-old woman has a right breast biopsy (see Figure 6-4). What is her lifetime risk of developing invasive carcinoma in the contralateral (left) breast?
(A) She is not at risk for developing breast cancer
(B) The risk is identical to her right breast
(C) The risk is 20% higher compared with her right breast
(D) The risk is 20% less compared with her right breast
(E) The risk is 40% less compared with her right breast
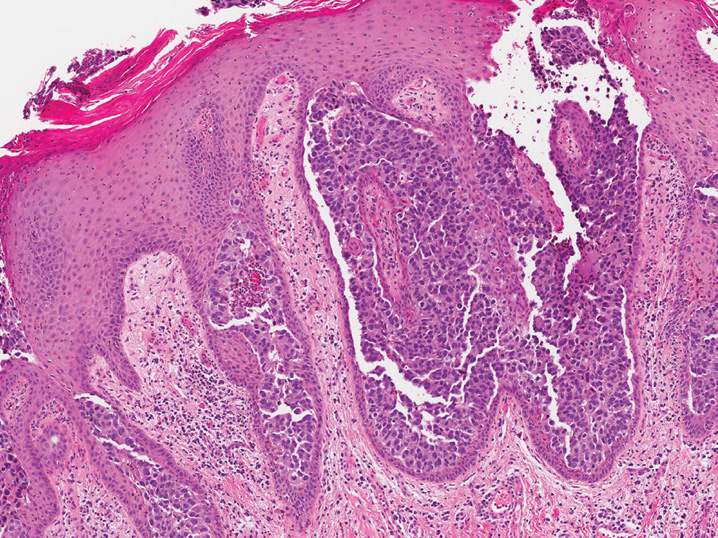
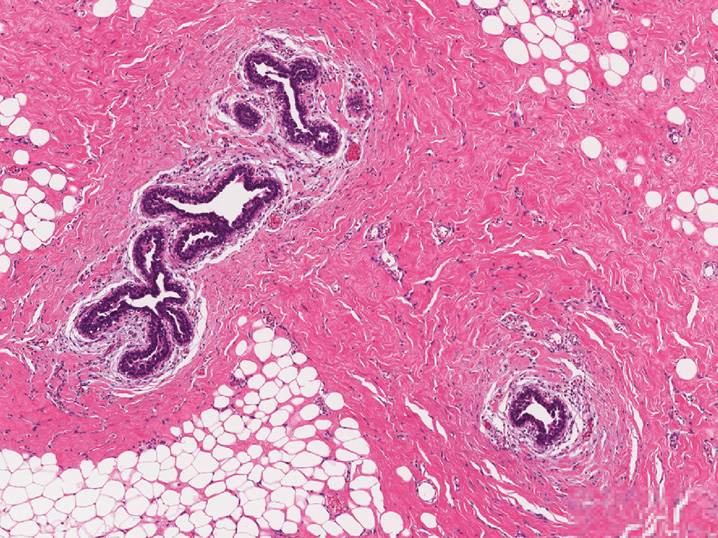
5. A 57-year-old woman presents to her physician for a unilateral red nipple with a scale crust. A biopsy of the nipple is performed (see Figure 6-5). Which of the following is accurate regarding this process?
(A) A patient with ductal carcinoma in situ and this finding is staged as pT4 disease due to skin involvement
(B) Less than 50% of cases are associated with an underlying invasive or in situ mammary carcinoma
(C) Melanocytic markers are usually positive in these lesions
(D) Occurs in approximately 10% of patients with breast cancer
(E) The neoplastic cells are positive for HER2 immunohistochemical expression
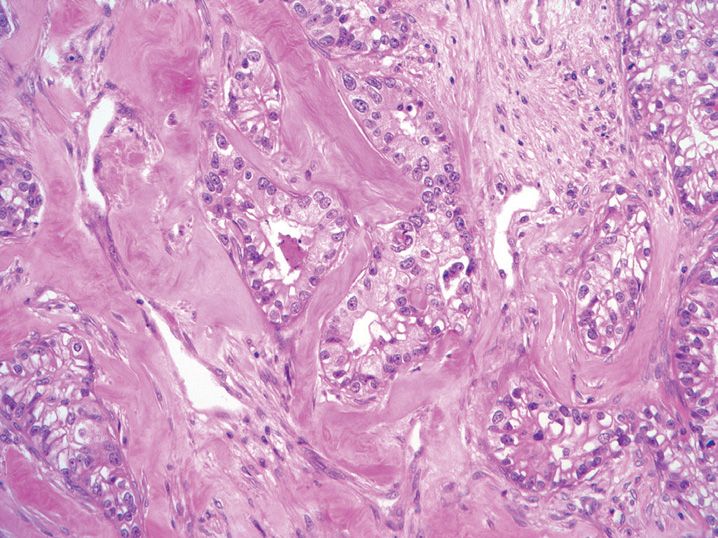
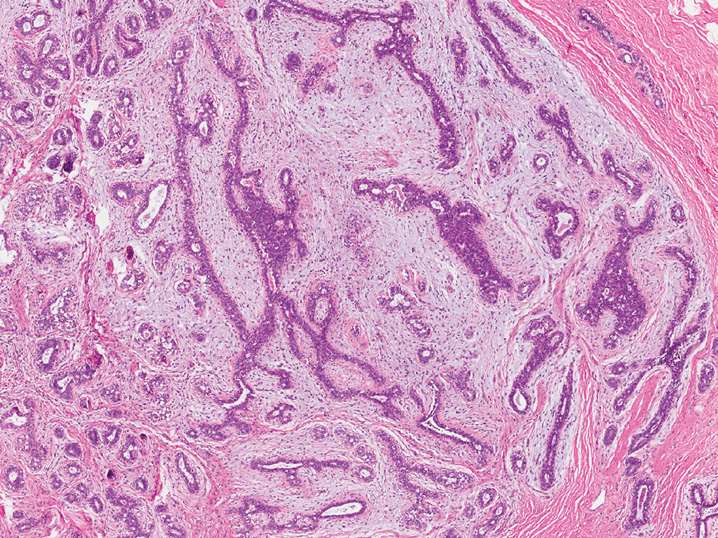
6. A 53-year-old woman has a breast biopsy performed (see Figure 6-6). At local excision, which of the following features is most important in predicting recurrence in this breast?
(A) Distance to margin <1 mm
(B) Estrogen receptor positivity
(C) Greatest dimension of the lesion
(D) High nuclear grade
(E) Necrosis
7. A 61-year-old woman has a punch biopsy of the skin of her breast performed, which shows the following change (see Figure 6-7). What clinical exam finding is typical in patients with this process?
(A) Bilateral milky nipple discharge
(B) Black-brown nodule with irregular borders
(C) Puckered skin involved by a firm exophytic mass
(D) Red swollen breast that has an irregular surface, resembling the surface of an orange
(E) Scaly white plaques and patches
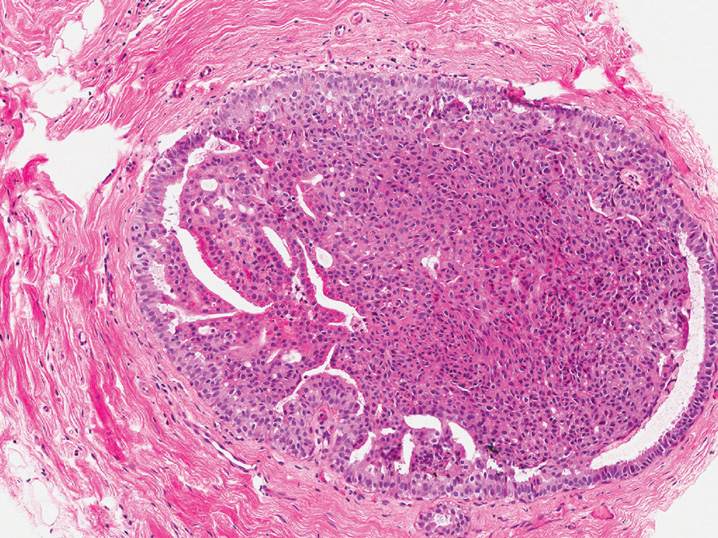
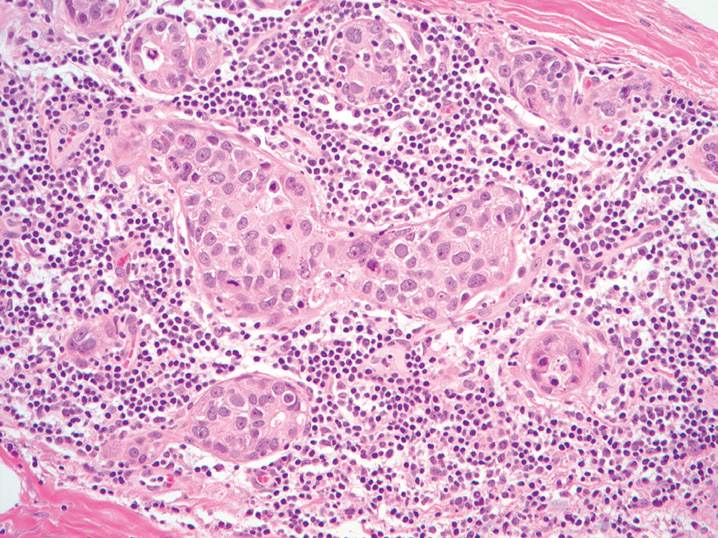
8. A woman undergoes a breast excision (see Figure 6-8). Which of the following findings would favor an interpretation of lobular carcinoma in situ (LCIS) over cancerization of the lobules by ductal carcinoma in situ (DCIS)?
(A) Fibroplasia in the surrounding stroma
(B) Large pleomorphic cells with significant atypia
(C) No staining for high-molecular weight cytokeratin
(D) Presence of DCIS in surrounding ducts
(E) Strong staining for E-cadherin
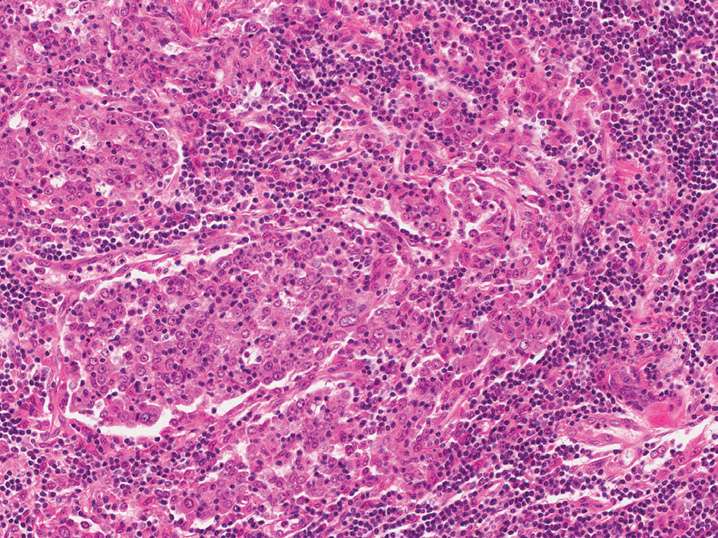
9. A 58-year-old woman undergoes a modified radical mastectomy for breast cancer (see Figure 6-9). Which of the following features, if present, would likely mitigate the more favorable prognosis typically associated with this lesion?
(A) Absent lymphoplasmacytic infiltrate
(B) >75% syncytial growth pattern
(C) High mitotic rate
(D) Pleomorphic (high grade) nuclei
(E) Well-circumscribed microscopically
10. A 67-year-old woman has a breast biopsy (see Figure 6-10). All of the following statements regarding this lesion are true except
(A) E-cadherin immunohistochemistry is negative
(B) Intracytoplasmic mucin droplets are characteristic
(C) Margin assessment is problematic due to “skip” lesions
(D) Retained normal breast structures is common
(E) Typically presents as microcalcifications on mammography
11. A 56-year-old woman undergoes local excision of a breast lesion (see Figure 6-11). All of the following statements regarding this lesion are true except
(A) Absence of epithelial elements in a low-power field is a worrisome feature for malignancy
(B) Heterologous elements (liposarcoma) can be seen
(C) Hypercellular stroma is a worrisome feature for malignancy
(D) Metastases are most commonly composed of the stromal component
(E) Surgical excision with wide margins is required
12. A 41-year-old woman undergoes excisional biopsy of a breast mass (see Figure 6-12). What immunohistochemical staining profile will the lesional cells demonstrate?
(A) Positive for CD31 and factor VIII; negative for smooth muscle actin, cytokeratin
(B) Positive for cytokeratin and E-cadherin; negative for CD31, smooth muscle actin, factor VIII
(C) Positive for cytokeratin; negative for CD31, E-cadherin, smooth muscle actin, factor VIII
(D) Positive for S-100; negative for CD31 and cytokeratin
(E) Positive for smooth muscle actin; negative for CD31, factor VIII, cytokeratin
13. A breast biopsy shows the following features (see Figure 6-13). What is the most likely clinical history associated with this process?
(A) A 13-year-old boy with breast enlargement
(B) A 23-year-old woman with a rubbery well-circumscribed mass
(C) A 45-year-old woman with bloody nipple discharge
(D) A 54-year-old woman with microcalcifications on mammography
(E) A 71-year-old woman with a spiculated mass on magnetic resonance imaging
14. A 36-year-old woman presents with a palpable breast lump. A biopsy is performed (see Figure 6-14). What clinical history is she most likely to provide upon additional questioning?
(A) Family history of early breast cancer and uterine cancer
(B) Recent pregnancy and breastfeeding
(C) Recent trauma to the breast
(D) Swollen red breast with peau d’orange-like texture
(E) Variable breast tenderness that follows her menstrual cycle
15. A 58-year-old woman has a breast biopsy performed (see Figure 6-15). Which of the following statements is true regarding this lesion?
(A) Almost always a “pure” tumor morphology
(B) Better prognosis than invasive ductal carcinoma, no specific type
(C) Epithelial membrane antigen immunohisto-chemical staining shows “inside out” apical staining
(D) Less than 40% of cases have lymph node metastasis at presentation
(E) Majority of cases are negative for estrogen receptor immunohistochemistry
16. A 66-year-old woman undergoes biopsy of a breast mass (see Figure 6-16). What is the most appropriate management of this tumor?
(A) Complete excision with axillary lymph node dissection
(B) Complete excision with optional sentinel lymph node biopsy
(C) Complete excision with subsequent estrogen receptor-antagonist therapy (e.g., tamoxifen)
(D) Modified radical mastectomy with adjuvant chemotherapy
(E) No excision is necessary due to the benign natural history of this disease
17. A 14-year-old girl presents with a breast mass near the areola. A biopsy is performed (see Figure 6-17). What genetic abnormality is associated with this lesion?
(A) BRCA1 mutation
(B) HER2 amplification
(C) TP53 mutation
(D) t(X;18) SYT–SSX translocation
(E) t(12;15) ETV6–NTRK3 translocation
18. A 75-year-old woman presents with red nodules on the skin of her breast. A biopsy was performed (see Figure 6-18). What clinical history is most likely to be associated with this lesion?
(A) Chronic sun damage and atypical nevus
(B) Swelling and enlargement of the breast with a deep ill-defined mass
(C) Previous contralateral invasive lobular carcinoma and mastectomy
(D) Previous ipsilateral invasive ductal carcinoma and lumpectomy
(E) Weeping, crusted nipple and underlying spiculated lesion on mammography
19. A 36-year-old woman is found to have a well-circumscribed lesion involving the nipple (see Figure 6-19). All of the following statements regarding this process are true except
(A) Complete excision is recommended to prevent recurrence
(B) Haphazard architecture can mimic infiltrating carcinoma
(C) Highly associated with an underlying breast carcinoma
(D) Often associated with papillary proliferations in adjacent ducts
(E) The glands are lined by two cell layers (epithelial and myoepithelial)
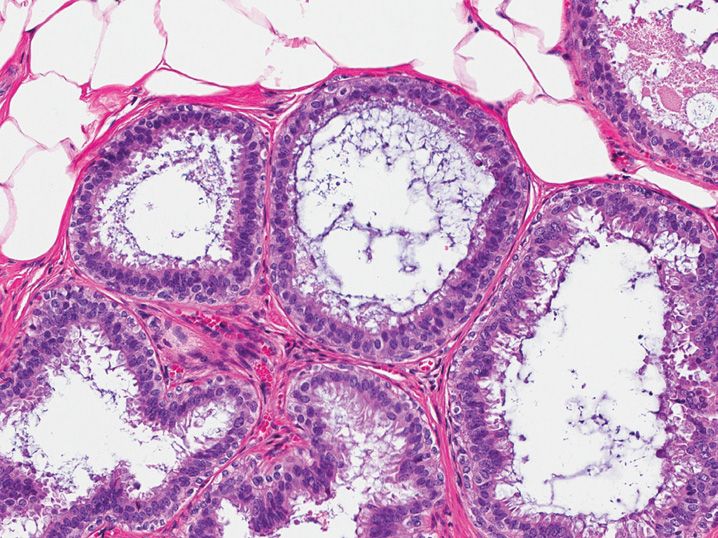
20. A 41-year-old woman undergoes breast reduction surgery, and the following finding is present in one duct profile (see Figure 6-20). What is the origin of the eosinophilic hyaline material present?
(A) Basement membrane proteins produced by myoepithelial cells
(B) Foreign material secondary to prior surgery
(C) Mucin produced by signet ring carcinoma
(D) Organizing fibrin formed secondary to intraductal hemorrhage
(E) Secretory product produced by apocrine epithelial cells
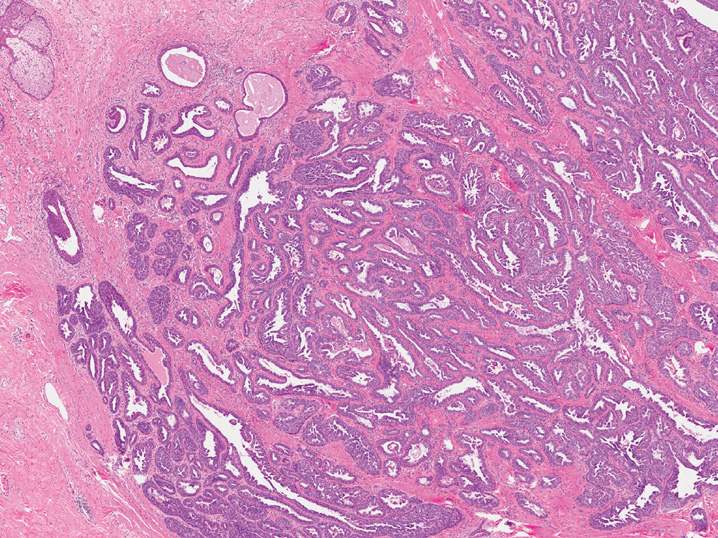
21. A 52-year-old woman undergoes breast core biopsy that shows several dilated ducts lined by the following epithelium (see Figure 6-21). What is the most appropriate management based on the findings present in this core biopsy?
(A) Local excision of this area to exclude malignancy
(B) Repeat core biopsy
(C) Return to routine screening
(D) Sentinel lymph node biopsy and wide local excision
(E) Simple mastectomy
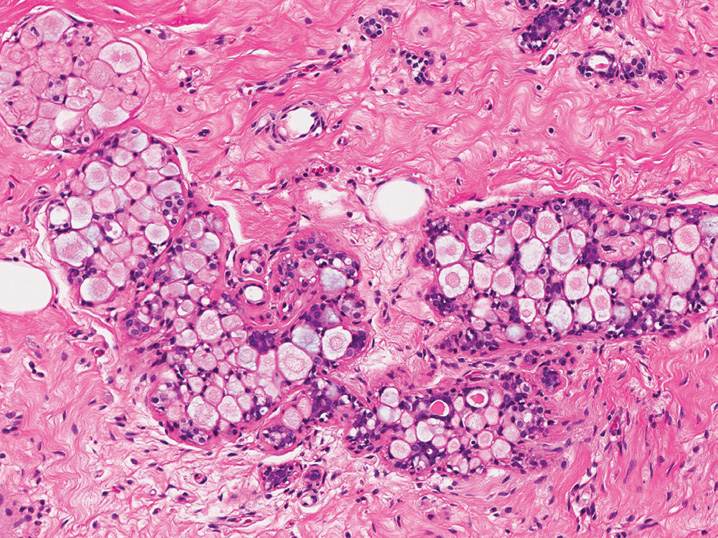
22. A 53-year-old woman undergoes breast excision (see Figure 6-22). What is the expected estrogen receptor (ER), progesterone receptor (PR), and E-cadherin immunohistochemical profile of this proliferation?
(A) Negative for ER, PR, and E-cadherin
(B) Positive for E-cadherin and negative for ER and PR
(C) Positive for ER and negative for PR and E-cadherin
(D) Positive for ER and PR and negative for E-cadherin
(E) Positive for ER, PR, and E-cadherin
23. A 49-year-old woman has a palpable mass in the subareolar region. A biopsy is performed (see Figure 6-23). What the best interpretation?
(A) Nipple adenoma
(B) Solitary intraductal papilloma
(C) Syringomatous adenoma
(D) Subareolar mastitis
(E) Tubular carcinoma
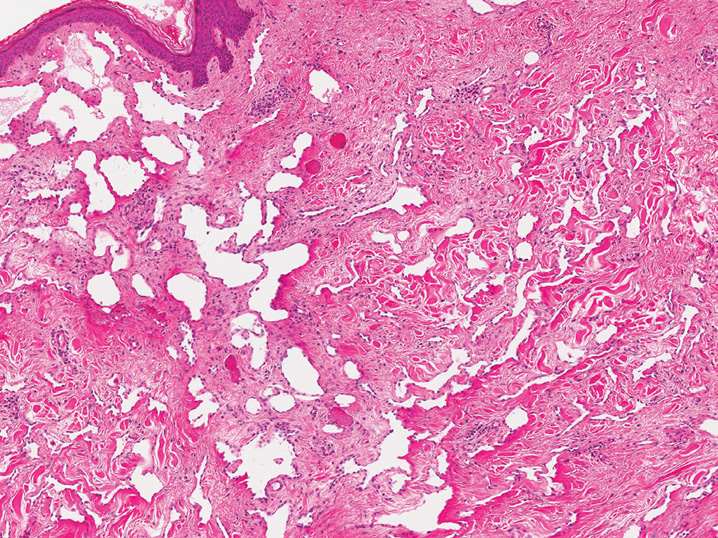
24. A 47-year-old woman is found to have a discrete, well-circumscribed radiodensity on mammography, which the surgeon enucleates easily at local excision. However, on histopathologic examination, the lesion has the following appearance (see Figure 6-24). What is the best interpretation based on the clinical findings?
(A) Fibroadenoma
(B) Invasive ductal carcinoma
(C) Mammary hamartoma
(D) Normal breast
(E) Phyllodes tumor
25. A 53-year-old woman undergoes a breast biopsy, which demonstrates microglandular adenosis. All of the following are true regarding this lesion except
(A) Complete excision is recommended to exclude malignancy
(B) Luminal material is periodic acid Schiff positive, diastase resistant
(C) Solitary glands within fibroadipose tissue are indicative of invasion
(D) Strong S-100 staining is typical
(E) The gland profiles lack myoepithelial cells
26. What is the current recommended handling protocol for the evaluation of clinically negative sentinel lymph nodes in the workup of invasive breast cancer according to the College of American Pathologists?
(A) Section at 1-mm intervals and submit every other section
(B) Section at 1-mm intervals and submit the entire node
(C) Section at 2-mm intervals and submit every other section
(D) Section at 2-mm intervals and submit the entire node
(E) Section at 5-mm intervals and submit the entire node
27. A 72-year-old woman presents with a breast mass. On core biopsy, abundant mucinous material is seen. Which of the following features would favor a diagnosis of mucocele-like lesion over mucinous (colloid) carcinoma?
(A) Adjacent ducts containing ductal carcinoma in situ
(B) Cribriform clusters of epithelial cells lacking calponin staining
(C) Immunohistochemical staining for synaptophysin
(D) Rare epithelial cells present within the mucin
(E) Strips of epithelial cells positive for p63
28. A woman undergoes breast biopsy and is found to have ductal carcinoma in situ (DCIS). A small focus of invasion is identified along the profile of one large duct. What size must this area be in order to qualify as microinvasion?
(A) ≤0.5 mm
(B) ≤1.0 mm
(C) ≤3.0 mm
(D) ≤5.0 mm
(E) There is no definition for microinvasion in the breast
29. Which of the following lesions, if present on a breast biopsy, is associated with a mildly increased risk of developing invasive carcinoma over a woman’s lifetime when compared with a woman without any other risk factors?
(A) Apocrine metaplasia
(B) Duct ectasia
(C) Fibroadenoma
(D) Nonproliferative fibrocystic change
(E) Sclerosing adenosis
30. A 35-year-old woman has a strong family history of breast cancer, and genetic testing demonstrates a BRCA1 gene mutation. All of the following statements regarding this genetic alteration are true except
(A) Associated with poorly differentiated breast cancers
(B) Between 20% and 40% of women with this mutation will develop ovarian cancer
(C) High association with HER2 positive breast cancers
(D) Lifetime risk of breast cancer is 40–90%
(E) Prevalence is higher in Ashkenazi Jewish women
31. Which of the following is not associated with an increased risk of developing breast cancer?
(A) First-degree relative with breast cancer
(B) Non-Hispanic white ethnicity
(C) Postmenopausal hormone replacement therapy
(D) Younger age at first live birth (20 years or younger)
(E) Younger age at menarche (11 years or younger)
32. A 39-year-old woman is diagnosed with bilateral invasive ductal carcinomas. Her history is notable for a previous osteosarcoma of the humerus at age 23 years. What genetic syndrome and mutation are most likely present in this woman?
(A) Cowden syndrome, PTEN mutation
(B) Hereditary breast and ovarian carcinoma syndrome, BRCA1 mutation
(C) Li–Fraumeni syndrome, TP53 mutation
(D) Lynch syndrome, MLH1 mutation
(E) von Hippel–Lindau syndrome, VHL mutation
33. Recent studies using gene expression profiling of breast carcinomas have identified five major patterns of gene expression, the most common of which is “luminal A.” Which of the following best describes luminal A type breast cancers’ morphologic appearance and immunohistochemical staining pattern for estrogen receptor (ER), progesterone receptor (PR), and HER2?
(A) Moderately differentiated HER2 positive invasive ductal carcinoma
(B) Poorly differentiated triple negative (ER, PR, HER2) invasive ductal carcinoma
(C) Poorly differentiated triple positive (ER, PR, HER2) invasive ductal carcinoma
(D) Well-differentiated ER-positive invasive ductal carcinoma
(E) Well-differentiated ER-positive invasive lobular carcinoma
34. Which of the following special types of invasive breast carcinoma is associated with a worse prognosis than infiltrating ductal carcinoma, not otherwise specified?
(A) Adenoid cystic carcinoma
(B) Basal-like carcinoma
(C) Colloid carcinoma
(D) Medullary carcinoma
(E) Tubular carcinoma
35. Which of the following findings on breast needle core biopsy can be followed without surgical excision?
(A) Acellular stromal mucin pools
(B) Atypical lobular hyperplasia in a woman with a mass
(C) Columnar cell lesion with atypia (flat epithelial atypia)
(D) Fibroadenoma without atypia and with an appropriate clinical exam
(E) Papillary lesion
36. Which of the following factors is the most important predictor of death in women with invasive carcinoma of the breast?
(A) Estrogen receptor status
(B) Histologic grade
(C) Mitotic rate
(D) Sentinel lymph node status
(E) Tumor size
37. The Nottingham Grading System (NGS) is used to determine the grade of invasive carcinomas of the breast and is an important independent prognostic factor. Which of the following tumor descriptions is appropriately graded [assume a high-power field (HPF) diameter of 0.50 mm]?
(A) Invasive ductal carcinoma with 20% tubule formation, marked pleomorphism, and 25 mitotic figures per 10 HPF—grade 2
(B) Invasive ductal carcinoma with 50% tubule formation, moderate nuclear atypia, and 11 mitotic figures per 10 HPF—grade 3
(C) Invasive ductal carcinoma with 90% tubule formation, marked pleomorphism, and 2 mitotic figures per 10 HPF—grade 1
(D) Invasive lobular carcinoma with 5% tubule formation, marked pleomorphism, and 3 mitotic figures per 10 HPF—grade 1
(E) Invasive lobular carcinoma with 5% tubule formation, minimal atypia, and 1 mitotic figure per 10 HPF—grade 2
38. A woman has a breast biopsy that shows a marked epithelial proliferation within a duct profile. The differential diagnosis includes low-grade ductal carcinoma in situ (DCIS), lobular carcinoma in situ involving a duct, or usual ductal hyperplasia. Which immunohistochemical staining profile would favor an interpretation of low-grade DCIS?
(A) 34BE12 (cytokeratin 903) and cytokeratin 5/6 (CK5/6) cannot distinguish between usual ductal hyperplasia and in situ carcinoma
(B) Negative for 34BE12 (cytokeratin 903) and CK5/6
(C) Positive for 34BE12 (cytokeratin 903) and CK5/6
(D) Positive for 34BE12 (cytokeratin 903), negative for CK5/6
(E) Positive for CK5/6 and negative for 34BE12 (cytokeratin 903)
39. A 43-year-old woman who has a germline BRCA1 gene mutation presents with pulmonary insufficiency and is found to have a large pleural effusion. Her history is significant for an invasive ductal carcinoma of the breast and high-grade ovarian serous carcinoma. Which panel of immunohistochemical stains would be most useful in determining the site of origin of her pleural metastasis?
(A) Cytokeratin 7 and cytokeratin 20
(B) Cytokeratin 20 and estrogen receptor
(C) Estrogen receptor and progesterone receptor
(D) Gross cystic disease fluid protein (GCDFP) and TTF-1
(E) Gross cystic disease fluid protein (GCDFP) and WT1
40. A woman with invasive ductal carcinoma of the breast undergoes sentinel lymph node biopsy, and after careful hematoxylin and eosin examination, no tumor cells are seen. Immunohistochemical staining with cytokeratin is performed. All of the following statements regarding immunohistochemical staining of sentinel lymph nodes for breast cancer are true except
(A) Benign nodal reticulum cells can be positive for cytokeratin
(B) Immunohistochemistry for the detection of metastatic breast carcinoma in sentinel lymph nodes is controversial
(C) Morphology and location of cytokeratin positive cells are important in final evaluation
(D) Rare single cells identified by immunohisto-chemistry alone are classified as pN0(i+)
(E) Tumor cells measuring 1.0 mm identified by IHC alone are classified as pN1mi(i+)
41. A woman undergoes breast core biopsy for micro-calcifications on mammogram, and an interpretation of flat epithelial atypia (columnar cell lesion with atypia) is rendered. What is the most likely neoplasm to be present in association with this process?
(A) Apocrine carcinoma
(B) High-grade ductal carcinoma in situ
(C) Invasive ductal carcinoma, grade 3
(D) Invasive tubular carcinoma
(E) Medullary carcinoma
42. A breast biopsy shows an atypical epithelial cell proliferation forming small nests in a background of radial-scar-like fibrosis. Which of the following immunohistochemical stains would be most helpful in determining the presence or absence of invasion?
(A) Cytokeratin 903 (34BE12)
(B) E-cadherin
(C) Estrogen receptor
(D) Smooth muscle myosin heavy chain
(E) S-100
43. According to the American Society of Clinical Oncology and the College of American Pathologists, standard fixation and tissue handling are needed to optimize HER2 status evaluation in breast cancer tissue. Which of the following scenarios is optimal for HER2 evaluation by immunohistochemistry?
(A) Core biopsy of ductal carcinoma in situ fixed in 10% neutral buffered formalin for 10 hours
(B) Core biopsy of invasive ductal carcinoma fixed in 10% neutral buffered formalin for 8 hours
(C) Core biopsy of invasive ductal carcinoma fixed in 10% neutral buffered formalin for 41 minutes
(D) Excisional biopsy of invasive ductal carcinoma fixed in 10% neutral buffered formalin for 50 hours
(E) Excisional biopsy of invasive ductal carcinoma fixed in Carnoy’s solution for 15 hours
44. HER2 testing in breast cancer can be performed using either immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH). Which of the following would be considered a positive result for the purposes of trastuzumab therapy?
(A) FISH HER2 average copy number of 5 signals per nucleus
(B) FISH HER2/CEP17 ratio of 3.1
(C) FISH polysomy of chromosome 17 (5 copies)
(D) IHC staining for HER2 with continuous membranous staining of 10% of cells
(E) IHC staining for HER2 with incomplete weak membranous staining in 80% of cells
45. A woman with clinical stage I invasive ductal carcinoma is given options of mastectomy, wide local excision (WLE) with postoperative radiation, or WLE without postoperative radiation to the ipsilateral breast. She asks her oncologist for more information regarding the difference in overall survival and local recurrence between these two options. Assuming her lymph nodes and margins will be negative, what do you tell her?
(A) Mastectomy has a significantly higher risk of local recurrence than WLE with or without radiation
(B) Mastectomy has a significantly lower risk of death than WLE with or without radiation
(C) There is no significant difference in overall survival and local recurrence between these three therapies
(D) WLE without radiation has a significantly higher risk of local recurrence than WLE with radiation
(E) WLE with radiation has a significantly higher risk of local recurrence than WLE without radiation
46. A woman undergoes breast core biopsy for suspicious microcalcifications identified on mammography. However, the core biopsy shows only normal breast tissue without calcifications. All of the following are appropriate next steps except
(A) Clinical and radiologic correlation of the mammogram and specimen radiograph
(B) Deeper levels to examine for a lesion
(C) Polarization of the slides for calcium oxalate crystals
(D) Radiologic examination of the tissue block for residual calcifications
(E) Repeat core biopsy, since the lesion was missed on first biopsy
47. A woman undergoes an excisional biopsy of a breast lesion (see Figure 6-25). What is the most likely clinical presentation of this lesion?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree