Patient Story
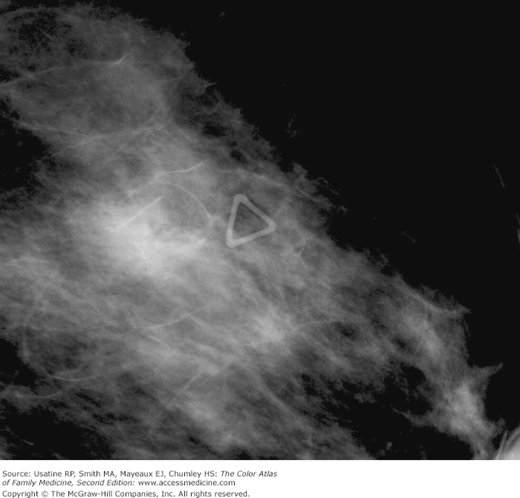
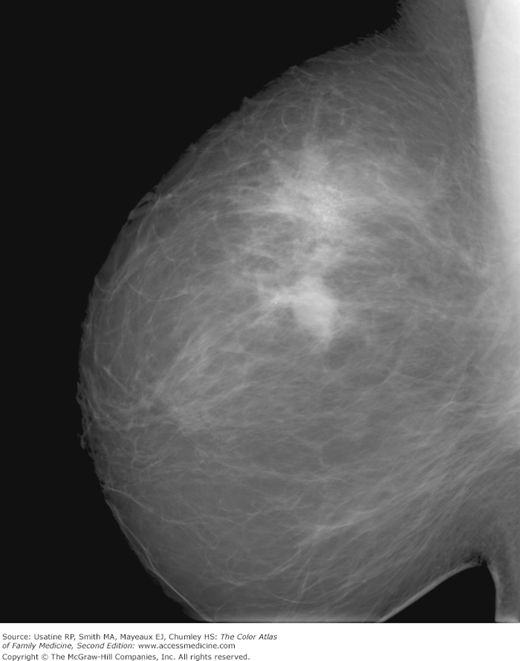
A 55-year-old woman presents for routine screening mammogram. The patient does not have any complaints but has a family history of breast cancer in a sister at age of 40 years. Her mammogram demonstrates an irregular mass with possible local spread (Figures 93-1 and 93-2). She is referred to a breast surgeon and the biopsy confirms the diagnosis of breast cancer.
Introduction
Breast cancer is a major health concern for all women. It is the most common female cancer in the United States, and the second most common cause of cancer death in women after lung cancer.1
Epidemiology
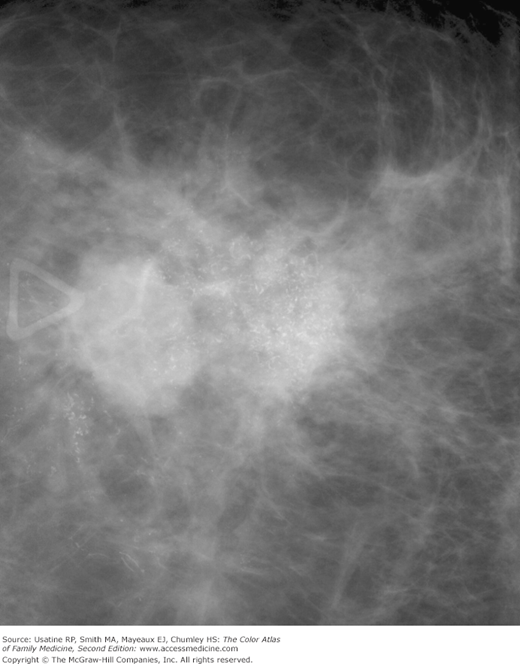
- In 2007, approximately 178,000 women in the United States were diagnosed with breast cancer.1 Breast cancer incidence in the United States has doubled over the past 60 years. Since the early 1980s, most of the increase has been in early stage and in situ cancers because of mammogram screening (Figures 93-1, 93-2, 93-3, and 93-4).
- Approximately 232,620 new cases of invasive breast cancer were expected to be diagnosed in the United States in 2011, and 39,970 were expected to die from the disease.1
- Globally, breast cancer is the most common cancer, and the leading cause of cancer death in females. Breast cancer incidence rates are highest in North America, Australia-New Zealand, and Europe, and lowest in Asia and sub-Saharan Africa.2
- Locally advanced breast cancer (LABC) has been decreasing in frequency over the past several decades, at least partially as a result of earlier diagnosis because of better screening (Figures 93-5, 93-6, 93-7, and 93-8). It represents 30% to 50% of newly diagnosed breast cancers in medically underserved populations.3
- Primary inflammatory breast cancer (IBC) is relatively rare, accounting for 0.5% to 2% invasive breast cancers.4 However, it accounts for a greater proportion of cases presenting with more advanced disease. IBC is a clinical diagnosis. At presentation, almost all women with primary IBC have lymph node involvement and approximately one third have distant metastases.5
Figure 93-4
Close-up view of the mass shown in Figure 93-3 demonstrating clear spiculations and microcalcifications. (Courtesy of John Braud, MD.)
Figure 93-6
The patient in Figure 93-5 showing breast retraction and brawny edema of the breast and arm. (Courtesy of Richard P. Usatine, MD.)
Figure 93-8
Ethiopian woman with breast cancer and five enlarged firm left axillary lymph nodes. Note the breast asymmetry and the peau d’orange skin on the left breast. The dark black area was caused by a “traditional healer” who burned the skin. Unfortunately the woman could not afford to get care at the local hospital, making her prognosis very grave. (Courtesy of Richard P. Usatine, MD.)
Etiology and Pathophysiology
- The incidence of breast cancer increases with age. White women are more likely to develop breast cancer than black women. One percent of breast cancers occur in men.
- Primary risk factors for the development of breast cancer include age older than 50 years, female sex, increased exposure to estrogen (including early menarche and late menopause), and a family history in a first-degree maternal relative (especially if diagnosed premenopausally.).
- Approximately 8% of breast cancers are hereditary and of these one-half are associated with mutations in genes BRCA1 and BRCA2. It is more common in premenopausal women, multiple family generations, and bilateral breasts.6 Typically, several family members are affected over at least three generations and can include women from the paternal side of the family.
- A history of a proliferative breast abnormality, such as atypical hyperplasia, may increase a woman’s risk for developing breast cancer.
- The selective estrogen receptor modulator tamoxifen (and possibly raloxifene) reduces the risk of developing breast cancer.
- The American Cancer Society, American College of Radiology, American Medical Association, and American College of Obstetrics and Gynecology all recommend starting routine screening at age 40 years.7
- The United States Preventive Services Task Force and the 2002 statement by the American Academy of Family Physicians recommend screening mammography every 1 to 2 years for women ages 40 years and older.8
- Women who have a family history of BRCA mutation should begin annual mammography between 25 and 35 years of age.9 SOR A
- MRI screening is more sensitive for detecting breast cancers than mammography and is being used to screen women with BRCA mutations.10 It is not proven that surveillance regimens that include MRI will reduce mortality from breast cancer in high-risk women.10
- Although the sensitivity of MRI is higher than that of conventional imaging. MRI has a lower specificity. One study suggests that unnecessary biopsies can be avoided with second-look ultrasound when MRI is positive and mammography is not. Second-look ultrasound can be used to recognize false-positive MRI results and guide biopsies.11
Risk Factors
- Positive family history of breast and/or ovarian cancer (especially with BRCA mutations).
- Personal history of breast cancer.
- Increasing age in women.
- Early age at menarche and late menopause.
- Prolonged exposure to and higher concentrations of endogenous or exogenous estrogen.
- Exposure to ionizing radiation.
- Dense breast tissue and atypical hyperplasia.
- Women who have had no children or who had their first child after age 30 have a slightly higher breast cancer risk.
- Low physical activity levels.
- High-fat diet.
- Alcohol intake of two or more drinks daily.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree