Brachiocephalic Reconstruction
John F. Eidt
Venkat R. Kalapatapu
Introduction
Reconstructions of the innominate, common carotid, and proximal subclavian arteries are relatively uncommon surgical procedures. Few current vascular surgery training programs provide significant operative experience with direct aortic arch reconstruction, and these operations are rarely reported by vascular surgeons recertifying in vascular surgery. Despite their rarity, direct reconstructive procedures of the aortic arch vessels represent an appealing option in selected patients for their durability and efficacy. In this chapter, the indications for reconstruction of the branches of the aortic arch will be reviewed and specific techniques for undertaking these varied and complex procedures will be presented.
With the exception of endarterectomy of isolated lesions at their origins and in situ repair of arch branch aneurysms, virtually all brachiocephalic reconstructions are “extra-anatomic” in that the bypass graft does not mimic normal anatomy. The primary question facing a vascular surgeon confronted with disease of the aortic arch branches is whether the aortic arch itself must be exposed directly or whether an extrathoracic vessel, typically the subclavian or carotid, can be used for inflow.
The declining operative experience with direct reconstruction of aortic arch branches is due to multiple factors. First, obstructive and/or aneurysmal disease of the proximal branches of the aortic arch occurs much less frequently than at other sites such as the carotid bifurcation. At the Texas Heart Institute, for example, surgical therapy of the innominate artery accounts for fewer than 2% of all operations performed for extracranial cerebrovascular occlusive disease. Second, the relative rarity of these lesions means that their natural history is uncertain. While it is appealing to apply the principles that have been established for the treatment of internal carotid artery occlusive disease to the branches of the aortic arch, there exist few data to support such a policy. Third, the outcome following direct surgical reconstruction is poorly established since long-term results have been reported by only a handful of surgical groups with a wide range of results. There are no prospective or randomized comparisons of the direct reconstruction of aortic arch with other alternatives. The choice of direct reconstruction over extra-anatomic or endovascular alternatives remains highly subjective depending on the training, experience, technical skills, and bias of the individual surgeon. Fourth, transternal reconstruction of the aortic arch branches has historically been associated with significant morbidity and mortality. Despite improvements in anesthetic technique and perioperative management, direct reconstruction of the branches of the aortic arch remains associated with significant risks including cardiopulmonary complications, stroke, and graft infection. Currently, extra-anatomic bypass is performed much more frequently and with lower perioperative risk than transthoracic approaches. Fifth, the application of endovascular techniques to lesions of the aortic branches has substantially reduced the apparent need for direct surgical reconstruction. In summary, the disease process is uncommon, the natural history of asymptomatic disease is uncertain, training opportunities are scarce, and the success of endovascular treatments have all contributed to the decline in direct reconstruction of the aortic arch branches. The recent development of a variety of so-called debranching procedures to extend the proximal landing zone of thoracic endografts has resulted in renewed interest in arch vessel surgery.
Atherosclerosis is by far the most common cause of occlusive disease of branches of the aortic arch in Europe and North America, followed by Takayasu’s arteritis, and radiation-induced arteritis. Occlusive lesions outnumber aneurysmal lesions approximately 10 to 1. Occlusive lesions of the aortic arch branches occur in a younger age group than is typical of carotid artery disease, with the mean age from 50 to 60 years. The reported surgical series of direct
reconstruction of aortic arch branches usually include a higher proportion of women than might be expected in series of lower extremity arterial disease. Coronary artery disease is present in 25% to 65% of patients with aortic branch vessel occlusive disease. This review will focus primarily on the treatment of atherosclerotic occlusive disease with parenthetic reference to other conditions as appropriate.
reconstruction of aortic arch branches usually include a higher proportion of women than might be expected in series of lower extremity arterial disease. Coronary artery disease is present in 25% to 65% of patients with aortic branch vessel occlusive disease. This review will focus primarily on the treatment of atherosclerotic occlusive disease with parenthetic reference to other conditions as appropriate.
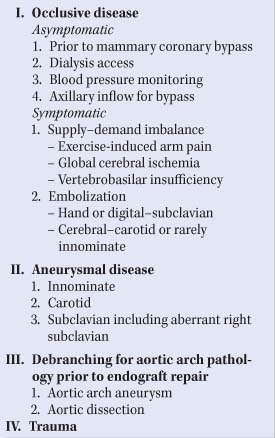
Brachiocephalic reconstruction is usually undertaken in one of four situations (Table 1): (a) the presence of occlusive disease in the arch branches; (b) aneurysms of the innominate, common carotid, and proximal subclavian arteries; (c) “debranching” of the aortic arch to extend the proximal landing zone prior to endovascular treatment of aneurysm and/or dissection, and (d) brachiocephalic trauma.
Clinical Presentation of Brachiocephalic Occlusive Disease
Innominate Artery
Occlusive lesions of the innominate artery are relatively uncommon. They may be asymptomatic or symptomatic. Asymptomatic lesions are usually discovered in the evaluation of asymmetric upper extremity pulses or blood pressures or during aortic arch imaging for unrelated indications. The natural history of asymptomatic innominate artery occlusive lesions is unknown. The treatment of asymptomatic lesions of the innominate artery has typically been indicated by the need for an associated vascular reconstruction dependent on the innominate artery such as the use of the right internal mammary artery for coronary bypass or prior to axillofemoral bypass.
Table 1 Indications for Brachiocephalic Reconstruction | |
|---|---|
|
Symptoms may be due to either atheroembolism or globally insufficient blood flow to the two vascular beds supplied by the innominate artery, the right arm and/or the right brain. Typically, atheroembolism is associated with ulcerated, less stenotic lesions, while hypoperfusion is typically due to high-grade stenosis or occlusion of the innominate artery often in combination with obstructive lesions in other arch vessels and reductions in cardiac output.
Cerebral symptoms associated with innominate artery lesions may be due to atheroembolism or global cerebral hypoperfusion. Symptoms may be focal and reproducible, suggesting recurrent microatheroembolism, or may be vague, nonspecific, and poorly lateralized. It may be impossible to determine the precise source of cerebral atheroemboli in the presence of tandem lesions in the innominate artery and the right internal carotid artery. Vague symptoms such as dizziness or sensations of instability or orthostatic weakness may be caused by a variety of metabolic, cardiac, and neurologic conditions other than innominate artery disease. Neurologic consultation may be helpful in the assessment of complex symptoms, and sophisticated imaging of the brain may be appropriate.
Right upper extremity symptoms should be assessed in all patients with innominate artery disease. Insufficient blood flow to the arm may be manifest as easy fatigability, pain with exertion, paresthesias, or a sensation of coolness. Because of its similarity to exercise-induced pain in the legs, pain in the arm with exertion is often, though inaccurately, called arm “claudication” (from the Latin root “to limp”). Atheroembolism from an innominate lesion can present with subungual splinter hemorrhages or bluish discoloration of the fingertips, which can progress to ulceration.
Common Carotid Artery
Obstructive lesions at the origin of the common carotid arteries may mimic the presentation of lesions at the carotid bifurcation but occur less frequently. Atherosclerosis, radiation injury, and giant cell arteritis are the most common pathologies in the common carotid arteries. Ipsilateral focal neurologic symptoms due to atheroembolism are often referred to as the four Ss: alterations in speech, sight, strength, or sensation. Cerebral atheroembolic events are more common in the setting of high-grade common carotid stenosis as opposed to complete occlusion. It is important to note that even in the setting of complete common carotid occlusion the internal carotid artery may remain patent through reversed flow in external carotid collaterals and may be the source of ipsilateral cerebral atheroemboli. In one recent case of common carotid occlusion, patency of the left internal carotid artery was maintained through collaterals from the ipsilateral thyrocervical trunk to the inferior thyroid artery to the superior thyroid artery to the carotid bifurcation. If the carotid bifurcation remains patent distal to an occluded common carotid artery, reconstruction may be accomplished with the relatively straightforward subclavian-to-carotid bifurcation bypass. Though synthetic grafts have wide acceptance in this location, we prefer to use an autogenous conduit such as the saphenous vein or (superficial) femoral deep vein in this location because of its resistance to kinking. If the common and internal carotid arteries are occluded, cerebral revascularization may require bypass to the intracranial internal carotid or middle cerebral arteries.
Subclavian Artery
Atherosclerotic obstruction is usually confined to the origin or first few centimeters of the subclavian artery. Arterial disease located in the distal subclavian and axillary arteries is more commonly caused by giant cell arteritis. Proximal subclavian occlusive disease usually presents in one of three clinical patterns: upper extremity pain with use, thromboembolism in the hand and fingers, or rarely vertebrobasilar insufficiency. Symptoms in the arm include early fatigue, pain with exercise, and a sensation of heaviness. Patients often complain of limitations with routine daily activities such as combing their hair. Less commonly, patients present with evidence of microembolism to the hand and fingers. Finally, occasional patients describe a variety of vague neurological symptoms including dizziness, vertigo, unsteadiness or imbalance, drop attacks, lightheadedness, visual disturbances, and hemiparesis or hemisensory dysfunction in association with subclavian disease. The term “subclavian steal” was first used by C.M. Fisher in 1961 in a discussion of two such patients reported in the New England Journal of Medicine. Today, subclavian steal
is used quite commonly to describe the finding of reversed flow in the vertebral artery ipsilateral to proximal subclavian stenosis or occlusion. Based on cerebral blood flow studies, the actual incidence of hemodynamically relevant “steal” is rare. The increased utilization of color flow Doppler in the investigation of cerebrovascular disease has resulted in more frequent detection of unsuspected subclavian steal. Isolated, asymptomatic subclavian steal is usually not clinically relevant, represents a stable and physiologically appropriate collateral pattern of blood flow, and does not warrant invasive diagnostic procedures or treatment. Subclavian steal does not appear to increase the risk of stroke. Carotid artery occlusive disease is present in approximately a quarter of patients with subclavian steal and is probably responsible for most focal hemispheric symptoms. Though described as a classical presentation, the onset of vertebrobasilar symptoms during arm exercise is distinctly uncommon. Due to the rather obscure nature of the symptoms in many patients with subclavian steal, it may be difficult to establish a definite link between the anatomic finding of reversed flow in a vertebral artery and the cerebral symptoms. Other causes of posterior cerebral symptoms include cervical spondylosis or injury, intrinsic vertebral or basilar artery disease, posterior fossa tumors, vestibular dysfunction, and systemic causes of cerebral hypoperfusion such as transient dysrhythmias or hypotension.
is used quite commonly to describe the finding of reversed flow in the vertebral artery ipsilateral to proximal subclavian stenosis or occlusion. Based on cerebral blood flow studies, the actual incidence of hemodynamically relevant “steal” is rare. The increased utilization of color flow Doppler in the investigation of cerebrovascular disease has resulted in more frequent detection of unsuspected subclavian steal. Isolated, asymptomatic subclavian steal is usually not clinically relevant, represents a stable and physiologically appropriate collateral pattern of blood flow, and does not warrant invasive diagnostic procedures or treatment. Subclavian steal does not appear to increase the risk of stroke. Carotid artery occlusive disease is present in approximately a quarter of patients with subclavian steal and is probably responsible for most focal hemispheric symptoms. Though described as a classical presentation, the onset of vertebrobasilar symptoms during arm exercise is distinctly uncommon. Due to the rather obscure nature of the symptoms in many patients with subclavian steal, it may be difficult to establish a definite link between the anatomic finding of reversed flow in a vertebral artery and the cerebral symptoms. Other causes of posterior cerebral symptoms include cervical spondylosis or injury, intrinsic vertebral or basilar artery disease, posterior fossa tumors, vestibular dysfunction, and systemic causes of cerebral hypoperfusion such as transient dysrhythmias or hypotension.
The increasing use of the internal mammary artery for coronary bypass grafting has led to the identification of so-called coronary subclavian steal. Coronary subclavian steal syndrome presents as angina due to subclavian stenosis or occlusion proximal to the origin of an internal mammary coronary artery bypass graft. Bilateral brachial blood pressures should be checked in all patients prior to internal mammary bypass and reassessed if angina recurs in follow-up. Percutaneous, endovascular, and direct surgical reconstruction may be appropriate in selected cases of coronary subclavian steal syndrome.
Subclavian obstruction should be suspected in any patient with asymmetric radial pulses on physical examination or a 20 mm Hg difference between brachial systolic blood pressures. Subclavian steal is two to three times more common on the left side than the right, perhaps owing to the short distance between the innominate and right vertebral artery. Symptoms are rare in the setting of isolated single-vessel disease due to the adequacy of cerebellar collateral circulation.
Isolated Aneurysmal Disease of the Brachiocephalic Vessels
The presence of isolated aneurysms of the brachiocephalic vessels in the absence of aortic arch aneurysm represents a much less common indication for surgical reconstruction. There is no consensus regarding the size threshold supporting repair of asymptomatic aneurysms but consideration should be given to aneurysm repair when the aneurysm is two to three times the diameter of the normal native vessel. Surgical treatment is clearly indicated for all enlarging and symptomatic aneurysms. Aneurysms involving an aberrant right subclavian artery represent a unique condition that may occasionally require complex surgical intervention. Aberrant right subclavian artery is one of the most common aortic arch anomalies, with a prevalence of approximately 1/200. Patients may present with hoarseness, odynophagia, and dysphagia. Direct reconstruction is complicated by the course of the aberrant artery posterior to the oropharynx and esophagus. A variety of novel hybrid endovascular options have been described.
Aortic Arch Pathology
Increasingly, reconstruction of the aortic arch branches is performed in preparation or in conjunction with endovascular treatment of a variety of conditions affecting the aortic arch. The most common conditions include degenerative aneurysm involving the aortic arch, aortic dissections, and blunt aortic injury results in focal aortic pseudoaneurysm. Progressive debranching of the aortic arch is designed to increase the effective proximal landing zone for the placement of thoracic endografts. By far the most common debranching procedure is a left carotid–subclavian bypass. Right common carotid to left common carotid bypass, in either a pretracheal or retropharyngeal tunnel, can be used to extend the proximal landing zone up the innominate artery. In its most extreme configuration, debranching of the innominate, left common carotid, and left subclavian arteries allows the placement of the endograft in the ascending aorta.
Trauma
Penetrating trauma of the aortic arch branches may necessitate direct reconstruction. In cases of hemodynamic instability, it may be preferable to perform simple suture ligation of catastrophic hemorrhage but the surgeon must be familiar with both direct and extra-anatomic reconstructive options.
Noninvasive Evaluation of Aortic Arch Branch Vessel Disease
The vascular laboratory may be helpful in the evaluation of aortic arch branch vessel occlusive disease. Normally, the upper extremity blood pressures should be approximately equal. Noninvasive evaluation of innominate artery lesions may demonstrate reduced blood pressure at rest in the right arm if the stenosis exceeds approximately 50% in diameter. Similar findings may occur in the setting of isolated occlusive disease in either subclavian artery. Less severe (<50 diameter reduction), clinically occult stenoses may be detected by increasing the flow across the diseased segment. Blood flow may be increased by arm exercise or by the induction of arm ischemia with a suprasystolic tourniquet inflated for 3 to 5 minutes. Microatheroembolism in the fingers may be manifest as reduced amplitude of plethysmographic waveforms and decreased finger blood pressure. Reduced pulsatility in the right common carotid artery is an indirect sign of innominate artery disease. In experienced hands, color flow Doppler is extremely accurate in the diagnosis of subclavian steal as manifest by reversal of flow in the ipsilateral vertebral artery. Flow reversal in the vertebral artery can sometimes be induced by arm ischemia. Cerebrovascular duplex examination may be useful to detect occult carotid bifurcation disease as well as reversal of flow in the vertebral arteries.
Imaging of the Aortic Arch
Accurate imaging of the aortic arch is essential to planning operative intervention. In most hospitals at the present time, catheter-based arch aortography with selective catheterization of the arch branches remains the confirmatory diagnostic test of choice. Coronary imaging should be obtained to eliminate the possibility of occult, severe coronary disease. Unfortunately, complete diagnostic cervicocerebral angiography carries a risk of stroke of up to 1%. Multislice computed tomography (CT) angiography with three-dimensional reconstruction has replaced catheter-based angiography in many institutions and avoids the small but measurable risk of embolism associated with catheter-based angiography. Although magnetic resonance angiography (MRA) has been used successfully in selected institutions, it has generally not achieved widespread acceptance as a solitary preoperative study by most surgeons.
Selection of Patients for Direct Reconstruction of the Aorta
In general, direct reconstruction of the aortic arch branches should be considered in younger patients with good cardiopulmonary function who have not had a previous sternotomy. Occlusive disease in a single branch of the aortic arch rarely warrants direct reconstruction, whereas multiple lesions argue in favor of the transsternal approach. Lesions that recur following either percutaneous or extra-anatomic treatment should be considered for definitive direct repair. Finally, direct reconstruction is preferred in cases of multiple branch vessel disease, particularly if extra-anatomic or endovascular alternatives are anatomically impossible due to the absence of an appropriate donor vessel, or are unappealing (e.g., in the presence of open cervical wounds or tracheostomy) or contraindicated. For example, axilloaxillary bypass should probably be avoided if a subsequent sternotomy for coronary disease is likely. While percutaneous angioplasty and stenting has assumed a prominent role in the initial management of aortic lesions, there are a variety of conditions that argue against percutaneous techniques. For example, percutaneous angioplasty of unstable or mobile innominate lesions that present with signs of peripheral atheroembolism should be undertaken with caution since angioplasty of these lesions may be more likely to embolize. The use of cerebral protection should be strongly considered in these cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree