(1)
Department of Pathology, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
Keywords
JawBone TumorsOsteosarcomaOsteoblastoma9.1 Introduction
Bone forming tumors that occur in the jaw are osteoblastoma and osteosarcoma, both histologically similar to those located in other parts of the skeleton. However, when occurring in the jaw, both entities have some specific, site-related aspects. Osteoblastoma has to be differentiated from cementoblastoma. The epitheloid osteoblastoma mimicks epithelial odontogenic tumors and osteosarcoma shows differential diagnostic problems related to ossifying fibroma. In this Chapter, clinicopathologic features of osteoblastoma and osteosarcoma are discussed with emphasis on these site-specific issues.
9.2 Osteoblastoma
Osteoblastoma is a neoplasm characterized by interconnecting trabeculae of woven bone and rimmed by prominent osteoblasts. Histologically, the lesion resembles osteoid osteoma and a size of 1.5 cm has been mentioned as border, larger lesions being osteoblastoma and smaller ones osteoid osteoma [1] but in the literature on jaw cases, this distinction is not always made and therefore, osteoid osteoma will be considered as similar to osteoblastoma in this context [2]. Approximately 10–15 % of osteoblastomas arise within the craniofacial skeleton, in most cases the mandible. As can be expected from a neoplasm, patients with osteoblastoma present with an expanding mass; radiographically, osteoblastomas show a mixed radiodense and radiolucent appearance, depending on the extent of intra-lesional mineralization (Figs. 9.1 and 9.2).
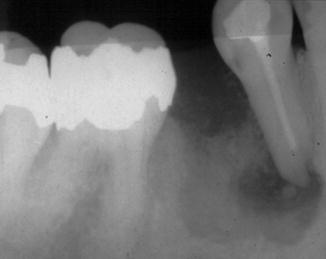
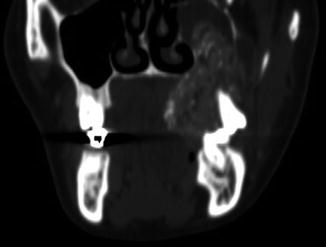
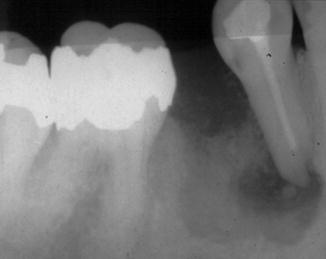
Fig. 9.1
Dental radiograph showing small osteoblastoma presenting as a radiolucent lesion with radiodense core. Strictly spoken, this picture could be interpreted as typical for an osteoid osteoma but for jaw lesions, osteoid osteoma and osteoblastoma are taken together
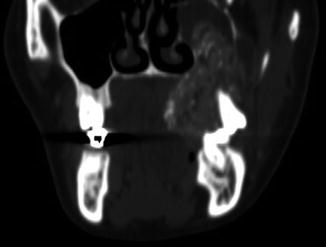
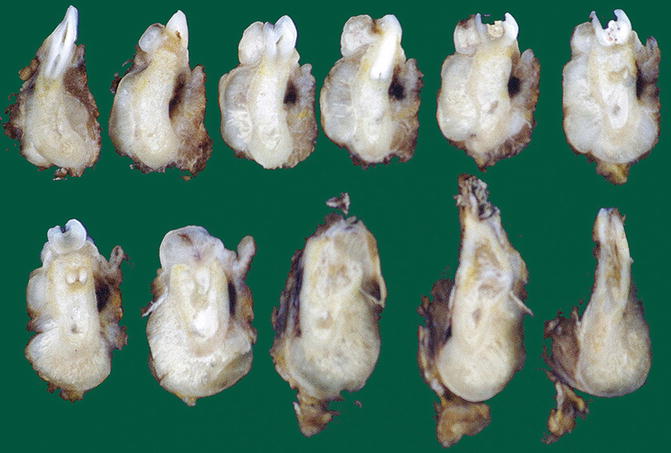
Fig. 9.2
Radiograph showing maxillary osteoblastoma extending into the maxillary sinus. Such lesions may be mistaken for a primary sinonasal tumor
Microscopically, osteoblastomas are composed of trabeculae of neoplastic woven bone that are rimmed prominently by osteoblasts with scattered osteoclasts (Figs. 9.3 and 9.4). The intertrabecular space contains a vascular loose connective tissue with foci of extravasated red blood cells (Fig. 9.5) and prominent osteoclasts also form part of the histomorphology (Fig. 9.6). Mitoses may occur but are not numerous (Fig. 9.7). Occasionally, spikes lined with swollen osteoblasts may form at the periphery of larger bony deposits (Fig. 9.8). If lesions with the morphology of an osteoblastoma show continuity with the root surface of an adjacent tooth, they should be diagnosed as cementoblastoma (see Chap. 4); osteoblastoma may lie adjacent to the root of a teeth but is not attached to its surface (Fig. 9.9).
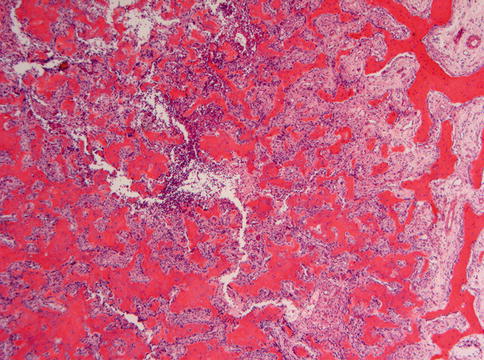
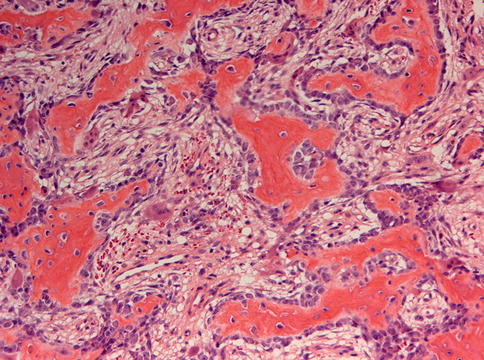
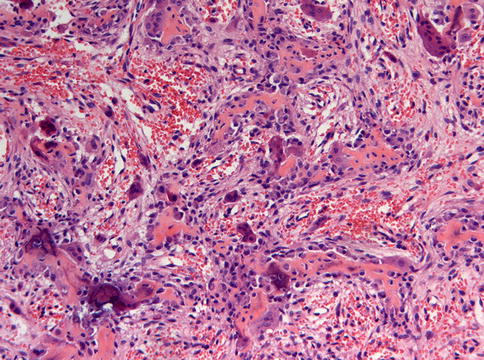
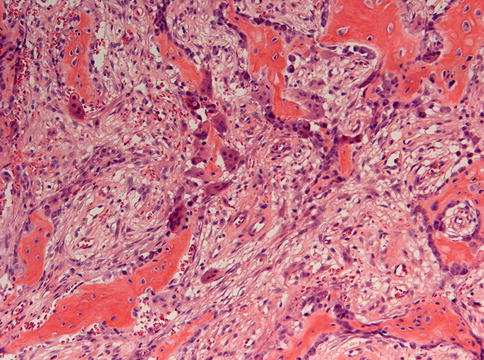
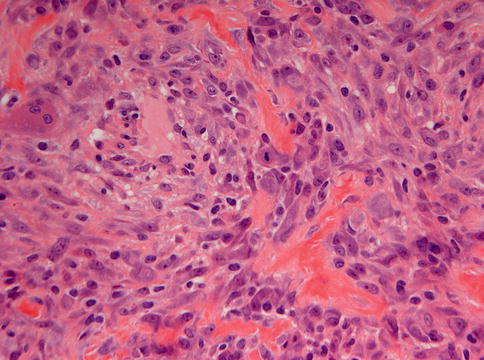
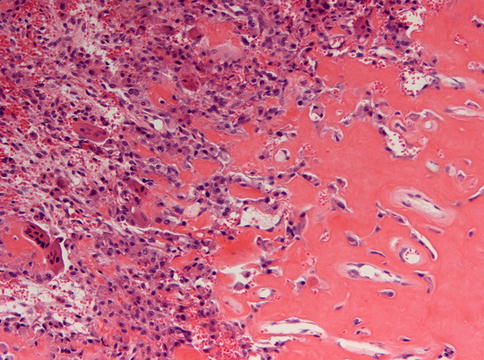
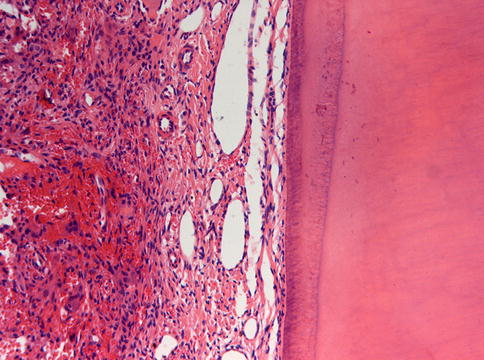
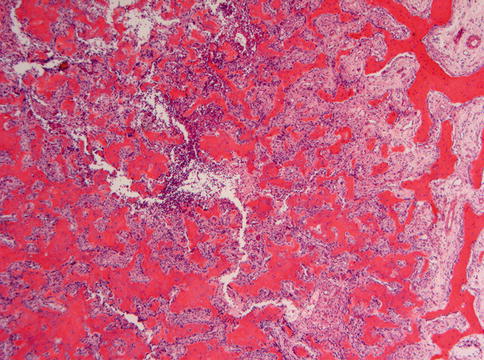
Fig. 9.3
Low power view of osteoblastoma to show the irregular bony spiculae in a loose fibrovascular stroma
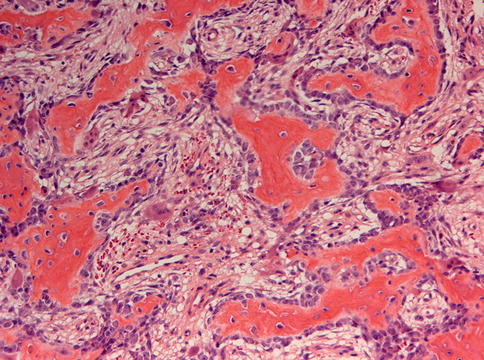
Fig. 9.4
At higher magnification, the dense osteoblastic rimming in osteoblastoma is obvious
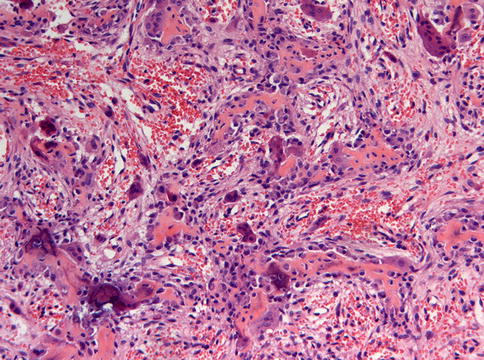
Fig. 9.5
The increased vascularity in osteoblastoma may lead to extravasation of erythrocytes
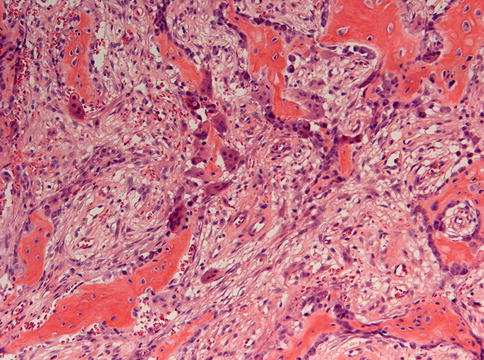
Fig. 9.6
A high number of osteoclasts also may be encountered in osteoblastoma
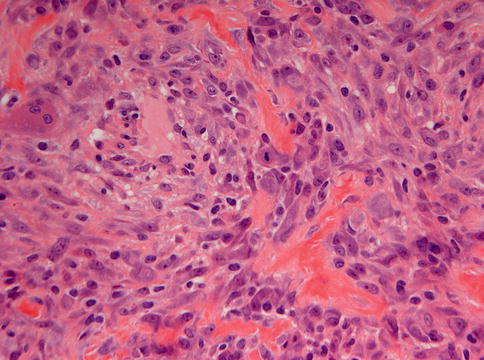
Fig. 9.7
At higher magnification, the bony trabeculae are rimmed with swollen osteoblasts in which occasionally, a mitotic figure may be encountered
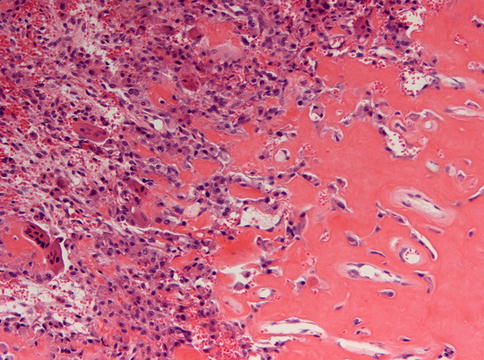
Fig. 9.8
Occasionally, spikes lined with osteoblasts form at the periphery of larger bony deposits which may mimic the peripheral rim of an osteosarcoma
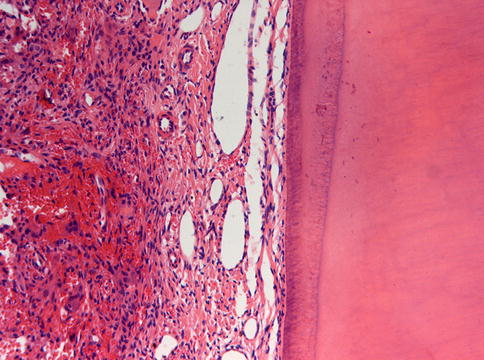
Fig. 9.9
In contrast with cementoblastoma, osteoblastoma may lie adjacent to the root surface of a tooth but is not connected to the tooth
A variant of osteoblastoma warrants a more extensive discussion because it has the jaws as a predilection site [3]. This concerns the so-called epitheloid multinodular osteoblastoma that is characterized by multiple nodules of epitheloid cells, most with a lacy, blue-bone matrix, occasionally sheets and nodules without matrix at (Figs. 9.10 and 9.11). This histological variant has the jaw bones as most common site [3]. Occasionally, similar cases have also been described under the designation aggressive osteoblastoma [4, 5]. The epitheloid morphology of this lesion is rather striking (Figs. 9.12 and 9.13).
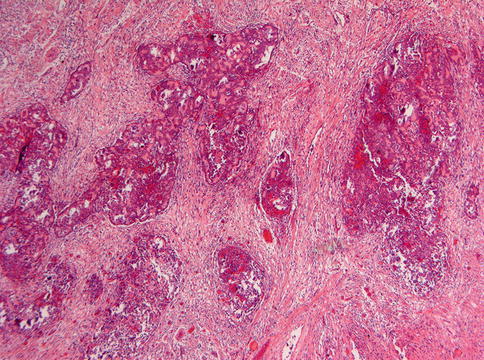
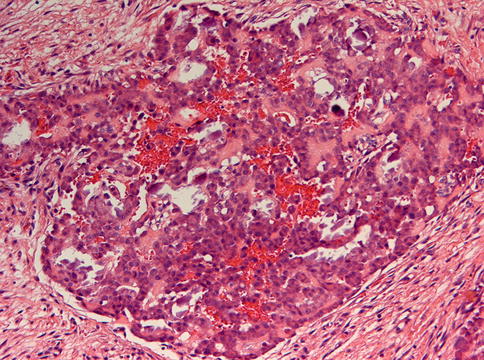
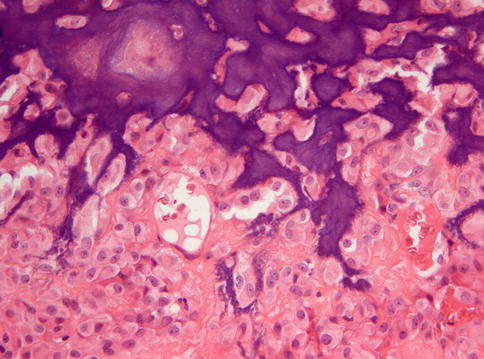
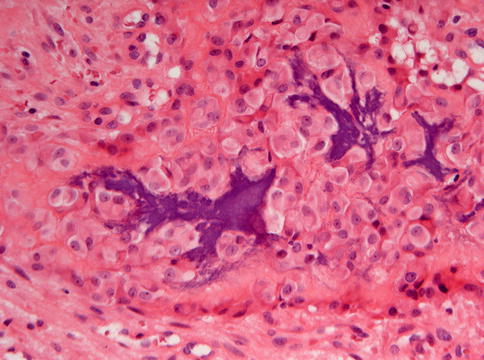
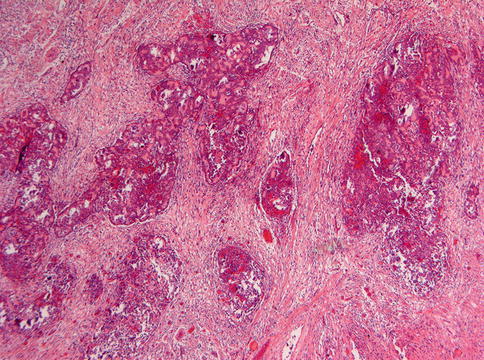
Fig. 9.10
Low power view of epitheloid multinodular osteoblastoma. Cellular nodules are lying in a more fibrous background
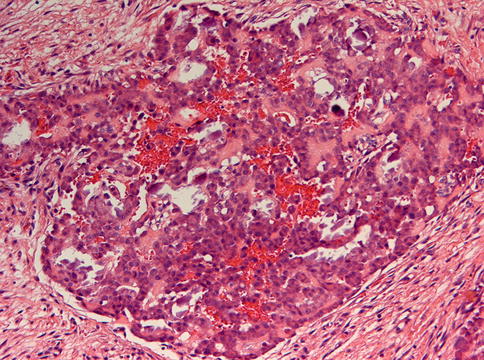
Fig. 9.11
The transition between the osteoblastoma nodules and the surrounding fibrous stroma in epitheloid osteoblastoma is rather abrupt, mimicking the histomorphology of an epithelial neoplasm
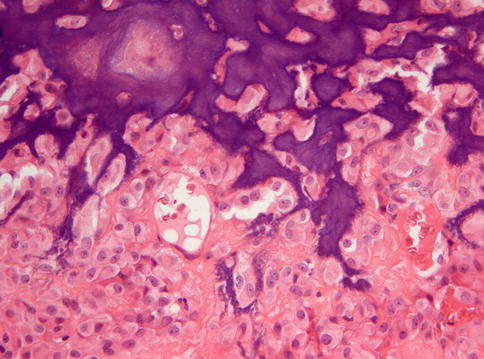
Fig. 9.12
At higher magnification, similarity between epitheloid osteoblastoma and an epithelial neoplasm is also reflected at the cellular level
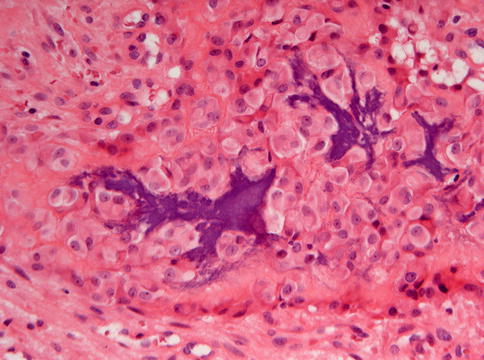
Fig. 9.13
Occasionally, cell clusters in epitheloid osteoblastoma almost completely lack any matrix production
The differential diagnosis of osteoblastoma includes osteosarcoma and fibro-osseous lesions. Osteosarcomas demonstrate invasive growth by which adjacent jaw bone is engulfed. This type of bone involvement has to be differentiated from the nodular growth pattern of the epitheloid (aggressive) osteoblastoma type in which there may be tumor nodules separated from each other by broad fibrous septa with reactive bone, a morphology that should not be mistaken for invasion but represents reactive jaw bone remodeling. Moreover, osteosarcoma shows cortical perforation and spread in adjacent soft tissues whereas osteoblastomas are separated from the soft tissues by a rim of cortical bone (Fig. 9.14).
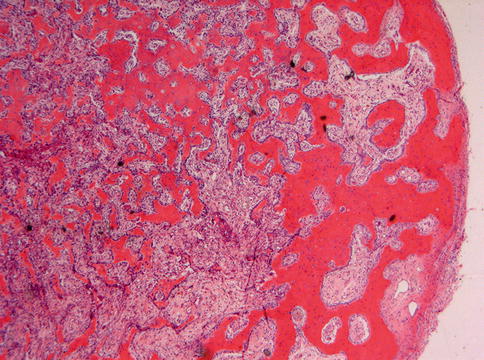
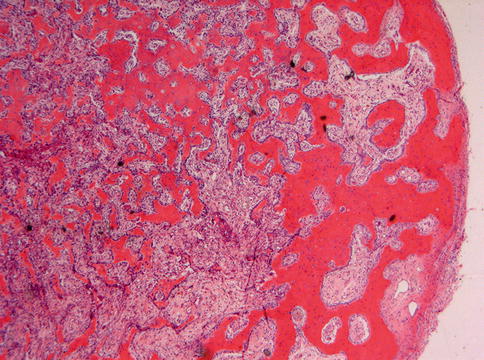
Fig. 9.14
At the periphery, a rim of cortical bone separates osteoblastoma from adjacent soft tissues. Such a rim is absent in osteosarcoma that invades the soft tissues
The fibro-osseous lesions demonstrate a fibroblastic stroma that lacks the vascularity and hemorrhage typical of osteoblastoma and although osteoblastic rimming may occur in some ossifying fibromas, especially in the juvenile trabecular subtype, the stromal features as mentioned above allow distinction between both entities, stroma in osteoblastoma being loose and vascular and fibroblastic in ossifying fibroma. Moreover, osteoblastoma lacks the garlands composed of osteoclastic giant cells, pseudocystic stroma degeneration, and hemorrhage as typical for this ossifying fibroma variant that is described in detail in Chap. 7.
Occasionally, the epitheloid (aggressive) osteoblastoma may mimic a calcifying epithelial odontogenic tumor, due to the presence of matrix deposits surrounded by large aggregates of epitheloid osteoblasts [4]. In doubtful cases, immunohistochemistry will solve the diagnostic problem by demonstrating the expression of epithelial markers in the former lesion. Moreover, the matrix in the calcifying epithelial odontogenic tumor stains positive for amyloid with Congo Red whereas in osteoblastoma, it is of collagenous nature.
The treatment of osteoblastoma is surgical excision. En bloc resection is usually curative; curettage may occasionally result in local recurrence [6, 7]. Malignant transformation of osteoblastoma to osteosarcoma is rare [8, 9]. Prognosis of the epitheloid (aggressive) osteoblastoma does not appear to be different from the more common classical type [3].
9.3 Osteosarcoma
Osteosarcoma is composed of neoplastic cells that deposit a collagenous matrix, which may transform into bone through deposition of calcium salts. Approximately 10 % of all cases occurs in the maxillofacial skeleton, most frequently the jaw bones but the sinonasal bony walls may also be involved [10]. Jaw osteosarcomas tend to occur approximately a decade later than the more common osteosarcomas of the long bones, with the majority of patients being older than 30 years of age [6]. Radiographs show a poorly defined mixed radiodense and radiolucent lesion, usually with soft tissue extension (Figs. 9.15 and 9.16). For those familiar with dental radiograps, the symmetrical widening of the periodontal ligament space shown by jaw osteosarcomas in tooth-bearing areas may be an extremely helpful diagnostic sign (Fig. 9.17) [11].