Chapter 52 Blunt Chest Trauma (Case 35)
Case: A 67-year-old male appeared to sustain blunt trauma to the chest in a head-on collision.
PATIENT CARE
Clinical Thinking
• Airway: Along with standard airway assessment for patency and protection, one must carefully look for tracheal injury. Is there an obstruction or injury due to blunt disruption? Are there associated facial or neck injuries that would preclude endotracheal intubation and might indicate the need for a surgical airway?
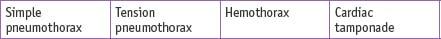
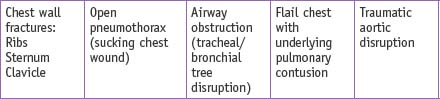
• Breathing: Assess for breath sounds. If the airway is intact and breath sounds are absent, does the patient need immediate needle decompression or chest tube to treat a tension pneumothorax? This decision should be made on auscultation examination alone rather than waiting for an x-ray if the patient is unstable. Does the patient have a flail segment or sucking chest wound that needs coverage?
• Circulation: After large-bore IVs are placed and resuscitation initiated, is the patient still in shock? Have all body areas been examined for bleeding sites?
• Disability: Perform a neurological examination, assess the Glasgow Coma Scale score, and evaluate rectal tone.
History
• If a motor vehicle collision, what details can be obtained from paramedics? VS in the field and en route?
Physical Examination
• Evaluate and reevaluate the VS and pulse oximetry. Look for JVD and observe chest wall motion, flail segments, or sucking wounds. Check for pulsus paradoxus.
• Interrupt the physical examination if a life-saving procedure such as airway or chest tube placement is needed.