Blastic Plasmacytoid Dendritic Cell Neoplasm
Kaaren K. Reichard, MD
Key Facts
Terminology
a.k.a. CD4(+)/CD56(+) hematodermic neoplasm, blastic NK-cell lymphoma
Etiology/Pathogenesis
Cell of origin: Plasmacytoid dendritic cell
Clinical Issues
Multiple tissues involved: Skin, peripheral blood and bone marrow, lymph node
Biologic factors: Rare disease, affects mainly adults, M:F = 3-4:1
Treatment: Multiagent chemotherapy
Disease course: Aggressive; median survival: 12-14 months
Microscopic Pathology
Blastic neoplasm: Often lymphoblast-like
Ancillary Tests
Cytochemistry: Negative for MPO and NSE
Immunophenotype
Positive for CD4, CD56, CD123, TCL1, BDCA2, TdT (50% weak, subset)
(-) for CD34, B-, T-, myeloid cell markers, EBV
Occasionally positive for CD33, CD2, CD7
Genetics
Complex karyotype
TCR and IGH@ germline configuration
Top Differential Diagnoses
Acute leukemia, myeloid or lymphoid
Aggressive NK-cell leukemia/lymphoma
Reporting Considerations
Diagnosis of exclusion
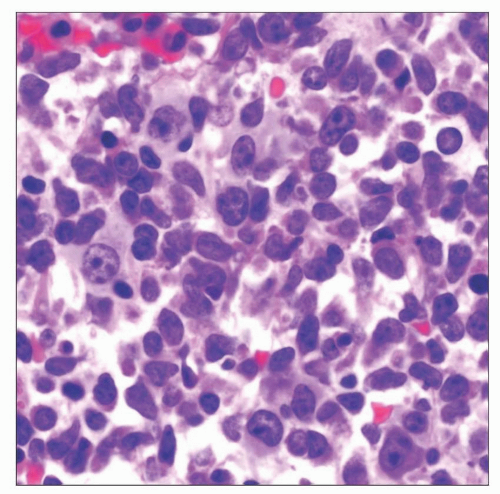
 Bone marrow aspirate smear from a patient with blastic plasmacytoid dendritic cell neoplasm shows typical lymphoblast-like cytology. This case also shows pseudopod formation. |
TERMINOLOGY
Abbreviations
Blastic plasmacytoid dendritic cell neoplasm (BPDCN)
Synonyms
CD4(+)/CD56(+) hematodermic neoplasm
Blastic NK-cell lymphoma
CD4(+)/CD56(+) lineage-negative malignancy
Agranular CD4(+) natural killer-cell leukemia
Definitions
Malignancy of plasmacytoid dendritic cells
Neoplasm with typical cutaneous and bone marrow involvement (“hematodermic”)
ETIOLOGY/PATHOGENESIS
Environmental Exposure
None clearly identified
Infectious Agents
No link with Epstein-Barr virus infection
Postulated Normal Cell Counterpart
Plasmacytoid dendritic cell
a.k.a. interferon-producing cell, dendritic cell type 1 (DC1)
a.k.a. (previously) plasmacytoid monocyte, plasmacytoid T cell
Produces high amounts of α-interferon
Innate immunity
Derives from either common lymphoid or myeloid precursor in bone marrow
Some Cases Associated with Myeloid Neoplasia
BPDCN and myelodysplasia
BPDCN and myelomonocytic leukemia
CLINICAL ISSUES
Epidemiology
Incidence
Exceedingly rare
Age
Mainly adults
Average age range: 60-67 years
Children and young adults also
Gender
Male predominant; M:F ratio = 3-4:1
Ethnicity
No known ethnic predisposition
Site
BPDCN involves multiple tissues
Skin
> 95% of cases
Often initial site of disease
Peripheral blood and bone marrow
60-90% of cases
May be involved at diagnosis (˜ 30-40%) or at relapse
Lymph nodes
30-40%
Presentation
Skin lesions
Abnormal CBC
Circulating neoplastic cells
Cytopenias
Blastic bone lesions
Treatment
Options, risks, complications
Definitive treatment unclear with so few cases
Multiagent chemotherapy
Some advocate acute leukemia-type regimen
Some advocate high-grade lymphoma-type regimen
Prognosis
Aggressive clinical course
Median survival: 12-14 months
Most cases initially respond to multiagent chemotherapy (> 80%)
Subsequent relapse in treatment resistant
Rare reports of long-term survival
MACROSCOPIC FEATURES
General Features
Skin lesions
Splenomegaly (< 20%)
Hepatomegaly (< 20%)
MICROSCOPIC PATHOLOGY
Predominant Pattern/Injury Type
Infiltrative
Predominant Cell/Compartment Type
Dendritic cell
Histologic Features
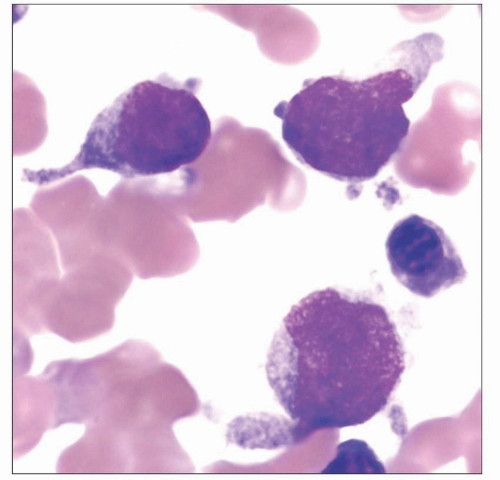
Peripheral blood
Variably sized cells with blastic cytomorphology
Agranular
Most often lymphoblast-like
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree