Bipolar Disorder
KEY CONCEPTS
![]() Bipolar disorder is a cyclic mental illness with recurrent mood episodes that occur over a person’s lifetime. The symptoms, course, severity, and response to treatment differ among individuals.
Bipolar disorder is a cyclic mental illness with recurrent mood episodes that occur over a person’s lifetime. The symptoms, course, severity, and response to treatment differ among individuals.
![]() Bipolar disorder is likely caused by genetic factors, environmental triggers, and the dysregulation of neurotransmitters, neurohormones, and second messenger systems in the brain.
Bipolar disorder is likely caused by genetic factors, environmental triggers, and the dysregulation of neurotransmitters, neurohormones, and second messenger systems in the brain.
![]() Clinicians should be sure to obtain a detailed history, including potential substance use and medical illness, to avoid a delay in the diagnosis and treatment of bipolar disorder.
Clinicians should be sure to obtain a detailed history, including potential substance use and medical illness, to avoid a delay in the diagnosis and treatment of bipolar disorder.
![]() The goal of therapy for bipolar disorder should be to improve patient functioning by reducing mood episodes. This is accomplished by maximizing adherence to therapy and limiting adverse effects.
The goal of therapy for bipolar disorder should be to improve patient functioning by reducing mood episodes. This is accomplished by maximizing adherence to therapy and limiting adverse effects.
![]() Patients and family members should be educated about bipolar disorder and treatments. Long-term monitoring and adherence to treatment are major factors in obtaining stabilization of the disorder.
Patients and family members should be educated about bipolar disorder and treatments. Long-term monitoring and adherence to treatment are major factors in obtaining stabilization of the disorder.
![]() Lithium and valproate are the mainstays of treatment for both acute mania and prophylaxis for recurrent manic and depressive episodes. Anticonvulsants (such as lamotrigine, carbamazepine, and oxcarbazepine) and second-generation antipsychotics (such as aripiprazole, olanzapine, risperidone, quetiapine, and ziprasidone) are alternative or adjunctive treatments for bipolar disorder. Anticonvulsants may be more effective than lithium in several mood subtypes (e.g., mixed states and rapid cycling). The use of lithium, valproate, or quetiapine for acute bipolar depression should be considered as a first-line treatment option.
Lithium and valproate are the mainstays of treatment for both acute mania and prophylaxis for recurrent manic and depressive episodes. Anticonvulsants (such as lamotrigine, carbamazepine, and oxcarbazepine) and second-generation antipsychotics (such as aripiprazole, olanzapine, risperidone, quetiapine, and ziprasidone) are alternative or adjunctive treatments for bipolar disorder. Anticonvulsants may be more effective than lithium in several mood subtypes (e.g., mixed states and rapid cycling). The use of lithium, valproate, or quetiapine for acute bipolar depression should be considered as a first-line treatment option.
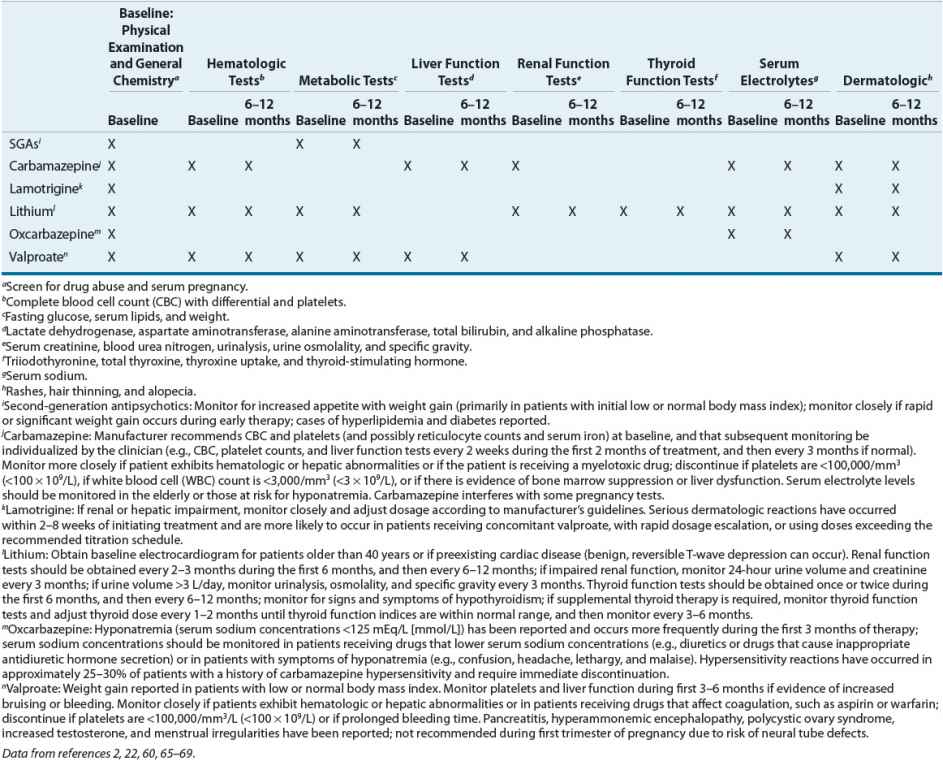
![]() Baseline and followup laboratory tests are required for some medications to monitor for adverse effects.
Baseline and followup laboratory tests are required for some medications to monitor for adverse effects.
![]() Some patients can be stabilized on one mood stabilizer, but others may require combination therapies or adjunctive agents during an acute mood episode. If possible, adjunctive agents should be tapered and discontinued when the acute mood episode remits and the patient is stabilized. Adjunctive agents may include benzodiazepines, additional mood stabilizers or antipsychotics, and/or antidepressants.
Some patients can be stabilized on one mood stabilizer, but others may require combination therapies or adjunctive agents during an acute mood episode. If possible, adjunctive agents should be tapered and discontinued when the acute mood episode remits and the patient is stabilized. Adjunctive agents may include benzodiazepines, additional mood stabilizers or antipsychotics, and/or antidepressants.
![]() Bipolar disorder is a common, chronic, and often severe cyclic mood disorder characterized by recurrent fluctuations in mood, energy, and behavior.1–3 It differs from recurrent major depression (or unipolar depression) in that a manic, hypomanic, or mixed episode occurs during the course of the illness.1 Bipolar disorder is a lifelong illness with a variable course and requires both nonpharmacologic and pharmacologic treatments for mood stabilization.1,2
Bipolar disorder is a common, chronic, and often severe cyclic mood disorder characterized by recurrent fluctuations in mood, energy, and behavior.1–3 It differs from recurrent major depression (or unipolar depression) in that a manic, hypomanic, or mixed episode occurs during the course of the illness.1 Bipolar disorder is a lifelong illness with a variable course and requires both nonpharmacologic and pharmacologic treatments for mood stabilization.1,2
EPIDEMIOLOGY
The overall prevalence of bipolar disorder was 4.5% in a U.S. comorbidity study: 1% meeting criteria for bipolar I, 1.1% for bipolar II, and 2.4% of patients with subthreshold recurrent mood cycling (i.e., cyclothymia, bipolar disorder not otherwise specified [NOS]).4 Symptom onset for depression or (hypo)mania in bipolar disorder typically occurs in late adolescence or early adulthood, with greater than two thirds developing symptoms before 18 years of age.5 Bipolar I disorder occurs equally in men and women, whereas bipolar II disorder is more common in women.1,2 Depression and mixed presentations may occur more frequently in women.6–8
ETIOLOGY AND PATHOPHYSIOLOGY
![]() The exact etiology of bipolar disorder is unknown. Bipolar disorder is thought to be a complex disease that is influenced by developmental, genetic, neurobiologic, and psychological factors.9 Many theories have been proposed regarding the pathophysiology of mood disorders. Family, twin, and adoption studies report an increased lifetime prevalence risk of having mood disorders among first-degree relatives of patients with bipolar disorder.10,11 Genetic linkage studies suggest multiple gene loci can be involved in the heredity of mood disorders.12–14 Neuroimaging studies have found neurochemical, anatomic, and functional abnormalities in bipolar patients.15 Many researchers suspect that altered synaptic and circuit functioning accounts for mood and cognitive changes seen in bipolar disorder, rather than dysfunction of individual neurotransmitters.16 Environmental or psychosocial stressors, immunologic factors, and sleep dysregulation all have been associated with bipolar disorder and can negatively influence the course of illness.17–21
The exact etiology of bipolar disorder is unknown. Bipolar disorder is thought to be a complex disease that is influenced by developmental, genetic, neurobiologic, and psychological factors.9 Many theories have been proposed regarding the pathophysiology of mood disorders. Family, twin, and adoption studies report an increased lifetime prevalence risk of having mood disorders among first-degree relatives of patients with bipolar disorder.10,11 Genetic linkage studies suggest multiple gene loci can be involved in the heredity of mood disorders.12–14 Neuroimaging studies have found neurochemical, anatomic, and functional abnormalities in bipolar patients.15 Many researchers suspect that altered synaptic and circuit functioning accounts for mood and cognitive changes seen in bipolar disorder, rather than dysfunction of individual neurotransmitters.16 Environmental or psychosocial stressors, immunologic factors, and sleep dysregulation all have been associated with bipolar disorder and can negatively influence the course of illness.17–21
CLINICAL PRESENTATION AND DIAGNOSIS
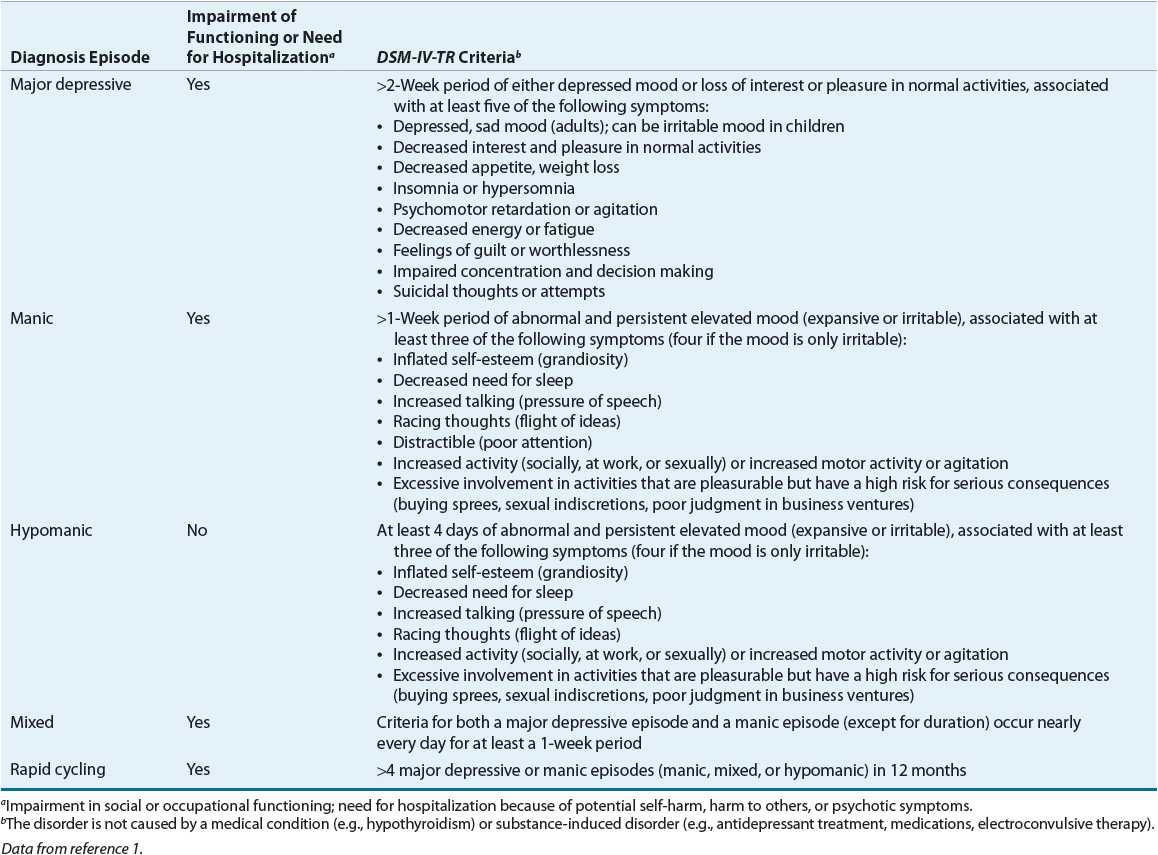
![]() The essential feature of bipolar spectrum disorders is a history of mania or hypomania that is not caused by any other medical condition, substance, or psychiatric disorder.1,2 The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) of the American Psychiatric Association (APA) details the present understanding of mood disorders.1 Bipolar disorder is divided into four subtypes based on the identification of specific mood episodes: bipolar I, bipolar II, cyclothymic disorder, and bipolar disorder NOS. See Table 52-1 for a definition of mood disorders by type of episode. Bipolar I and II can further be specified to reflect the most recent mood state (i.e., hypomanic or major depressive episode). See Table 52-2 for the evaluation and diagnostic criteria of mood episodes. Bipolar disorder is a cyclic mood disorder, and patients may sequentially experience different types of episodes with or without a period of normal mood (euthymia) between. Persons with bipolar disorder can have mood fluctuations that continue for months, or after one episode they can sometimes go years without recurrence of any type of mood episode. Comorbid conditions associated with bipolar disorder include, but are not limited to, substance abuse, personality disorders, anxiety disorders, eating disorders, and a higher incidence of several medical conditions.1–3,22–26
The essential feature of bipolar spectrum disorders is a history of mania or hypomania that is not caused by any other medical condition, substance, or psychiatric disorder.1,2 The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) of the American Psychiatric Association (APA) details the present understanding of mood disorders.1 Bipolar disorder is divided into four subtypes based on the identification of specific mood episodes: bipolar I, bipolar II, cyclothymic disorder, and bipolar disorder NOS. See Table 52-1 for a definition of mood disorders by type of episode. Bipolar I and II can further be specified to reflect the most recent mood state (i.e., hypomanic or major depressive episode). See Table 52-2 for the evaluation and diagnostic criteria of mood episodes. Bipolar disorder is a cyclic mood disorder, and patients may sequentially experience different types of episodes with or without a period of normal mood (euthymia) between. Persons with bipolar disorder can have mood fluctuations that continue for months, or after one episode they can sometimes go years without recurrence of any type of mood episode. Comorbid conditions associated with bipolar disorder include, but are not limited to, substance abuse, personality disorders, anxiety disorders, eating disorders, and a higher incidence of several medical conditions.1–3,22–26
TABLE 52-1 Mood Disorders Defined by Episodes
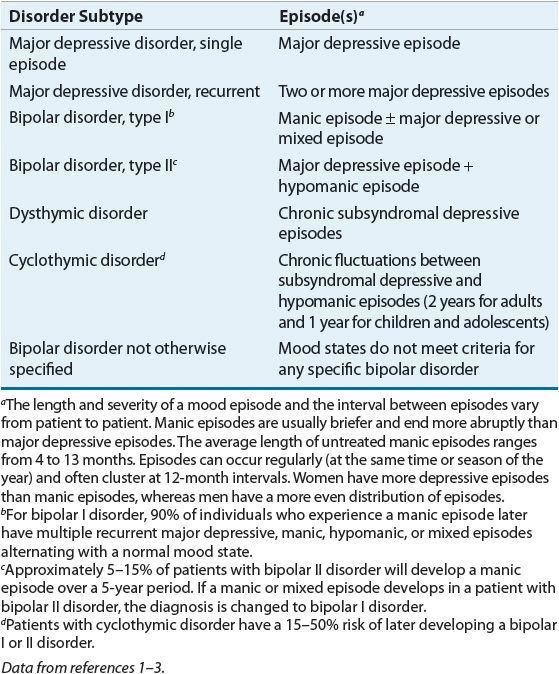
TABLE 52-2 Evaluation and Diagnosis of Mood Episodes
DIAGNOSTIC DIFFICULTY
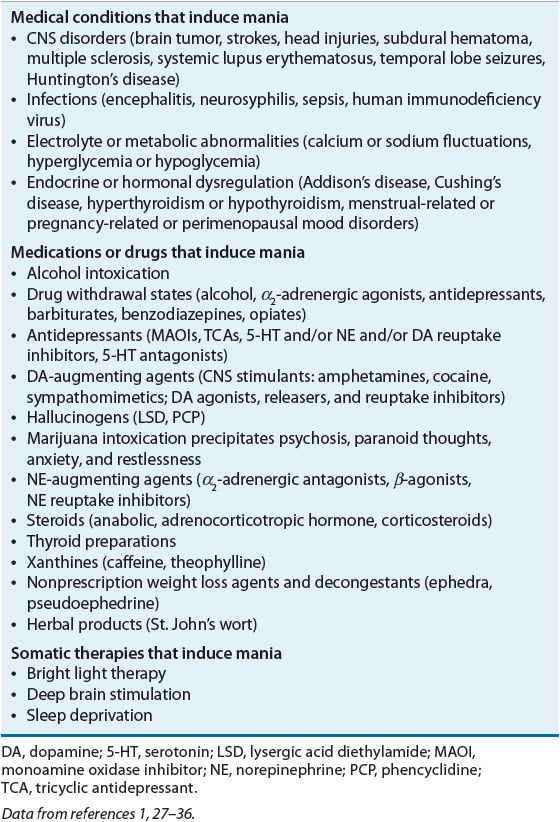
Episodes of mania or depression may be induced or caused by medical illness, medications, or substance intoxication or withdrawal (see Table 52-3 for causes of mania and Table 51-1 for causes of depression).1,2 A complete medical, psychiatric, and medication history; physical examination; and laboratory testing are necessary to rule out any organic causes of mania or depression.2 An accurate diagnosis is important because some psychiatric and neurologic disorders present with manic-like or depressive-like symptoms.2,3 Bipolar disorder commonly co-occurs with substance use disorders and may be difficult to diagnose in the presence of cocaine use.37 When making the diagnosis of new-onset bipolar disorder in a geriatric population, clinicians should be particularly aware of secondary causes of mania and depression that may impact treatment.38
TABLE 52-3 Secondary Causes of Mania
Another disease state that has a similar presentation to bipolar disorder is schizoaffective disorder. This disease is a mix between schizophrenia and bipolar disorder. Patients with schizoaffective disorder have mood episodes, but the distinguishing factor from bipolar disorder is that these patients experience psychosis even between mood episodes during periods of euthymia. Clinicians must rely on family members or others who know the patient well to determine if the patient is psychotic between mood episodes. It can be difficult for clinicians to obtain a full psychiatric history on patients, thus making schizoaffective disorder widely diagnosed. Schizoaffective disorder is treated with mood stabilizers and antipsychotics as maintenance therapy.
COURSE OF ILLNESS
![]() Bipolar disorder is frequently not recognized and treated for many years because of its fluctuating course and episodic mood states.2,3 Patients may have delays in treatment ranging 8 to 13 years from onset of index mood episode until initiation of mood stabilizer.39 This delay confers a risk of poor social functioning, increased hospitalizations, and a greater likelihood of lifetime suicide attempts.40 Onset of illness in early childhood tends to be associated with increased mood episodes, rapid cycling, and comorbid psychiatric conditions as well as a stronger family history of mood disorders.41 Gender differences may influence a patient’s course of illness, tolerability of medication, and response to treatment. Women are more likely to have increased depressive symptoms, older age of onset, better compliance, complex management in pregnancy, and higher association with physical illness such as thyroid abnormalities than men are. In men there may be increased incidence of mania and substance use.42
Bipolar disorder is frequently not recognized and treated for many years because of its fluctuating course and episodic mood states.2,3 Patients may have delays in treatment ranging 8 to 13 years from onset of index mood episode until initiation of mood stabilizer.39 This delay confers a risk of poor social functioning, increased hospitalizations, and a greater likelihood of lifetime suicide attempts.40 Onset of illness in early childhood tends to be associated with increased mood episodes, rapid cycling, and comorbid psychiatric conditions as well as a stronger family history of mood disorders.41 Gender differences may influence a patient’s course of illness, tolerability of medication, and response to treatment. Women are more likely to have increased depressive symptoms, older age of onset, better compliance, complex management in pregnancy, and higher association with physical illness such as thyroid abnormalities than men are. In men there may be increased incidence of mania and substance use.42
The kindling theory is used to explain why bipolar disorder progresses over one’s life and why preventative treatment is imperative. Episodes can become longer in duration and more frequent with aging.2 Usually there is a period of normal functioning between episodes, but approximately 20% to 30% of patients with bipolar I disorder and 15% with bipolar II disorder have no period of euthymia because of mood lability, residual mood symptoms, or a direct switch to the opposite polarity.1
Rapid cycling (more than four mood episodes per year) is more common in females and occurs in approximately 10% to 20% of bipolar I and II disorder patients.2,3,43,44 Frequent and severe episodes of depression appear to be the most common hallmark of rapid cycling. Use of alcohol, stimulants, antidepressants, sleep deprivation, hypothyroidism, and seasonal changes can play a role in rapid cycling.3,44,45 Seasonal patterns of mania in the summer and depression during the winter have been observed. Rapid-cycling patients have a poorer long-term prognosis and often require combination therapies.3
Fluctuations in hormones and neurotransmitters during the luteal phase of the menstrual cycle, postpartum period, and perimenopause (starting ~10 years before menopause) can precipitate mood changes and increase cycling.1,43,46 Women with bipolar I disorder are at greater risk for relapse into mania or depression during the postpartum period.2 If a severe mood episode occurs postpartum, there is an increased risk for recurrences during subsequent postpartum periods.2
Alcohol and substance abuse is common among patients with bipolar disorder and can have a significant impact on the age of onset, course of the illness, and response to treatment.3,22,23 Alcohol and drug abuse or dependence has been reported in 46% and 41% of bipolar patients, respectively.2,22 Patients with substance use disorders are more likely to have an earlier onset of their illness, mixed states, higher rates of relapse, a poorer response to treatment, comorbid personality disorders, increased suicide risk, and more psychiatric hospitalizations.3 Bipolar patients often self-medicate with substances such as alcohol or cocaine during episodes, resulting in further impairment of judgment, poor impulse control, treatment nonadherence, and a worsening of the clinical course.2,3,47
More than one half (55% to 65%) of bipolar I patients have some degree of functional disability after the onset of their illness, and approximately 10% to 20% of bipolar patients have severe impairment in their psychosocial and occupational functioning.2,3,48 In a 1-year longitudinal study in 258 bipolar patients, two thirds had four or more mood episodes a year despite comprehensive pharmacologic treatment, and approximately 33.2% of the year was spent being depressed compared with 10.8% of the time in a manic phase.48
Compared with the general population, individuals with bipolar disorder have a 2.3 times higher mortality rate. Suicide attempts occur in up to 50% of patients with bipolar disorder, and approximately 10% to 19% of individuals with bipolar I disorder commit suicide.1–3,49 Studies suggest patients with bipolar II disorder have more suicide attempts than bipolar I patients.49
The best predictor for level of functioning during a person’s lifetime is adherence with medication treatment. Medication discontinuation occurs in up to 50% of patients secondary to intolerance of drug-induced side effects.50 Failure to recognize the disorder, reluctance to acknowledge it, or poor adherence with treatment are reasons an estimated two thirds of patients with bipolar disorder do not receive appropriate treatment. Nonadherence with pharmacologic treatment and substance abuse are major factors in relapse and hospitalizations.2,3
TREATMENT
Desired Outcome
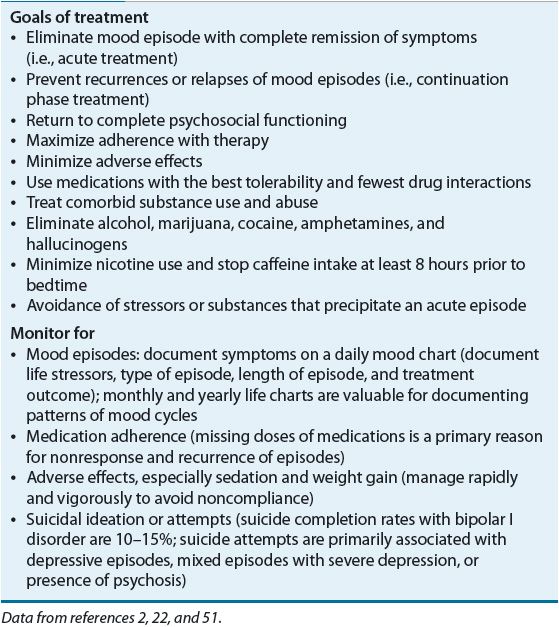
![]() The desired outcome in treating bipolar disorder is to effectively resolve acute manic, hypomanic, and depressive episodes, prevent further episodes, maintain good functioning, promote treatment adherence, and minimize side effects.2,3 The general principles and goals for the management of bipolar disorder are found in Table 52-4.
The desired outcome in treating bipolar disorder is to effectively resolve acute manic, hypomanic, and depressive episodes, prevent further episodes, maintain good functioning, promote treatment adherence, and minimize side effects.2,3 The general principles and goals for the management of bipolar disorder are found in Table 52-4.
TABLE 52-4 General Principles for the Management of Bipolar Disorder
General Approach to Treatment
![]() Treatment of bipolar disorder must be individualized because the clinical presentation, severity, and frequency of episodes vary widely among patients. Treatment approaches should include both nonpharmacologic and pharmacologic strategies.3 Patients and family members should be educated about bipolar disorder (e.g., symptoms, causes, and course) and treatment options. Long-term adherence to treatment is the most important factor in achieving stabilization of the disorder.
Treatment of bipolar disorder must be individualized because the clinical presentation, severity, and frequency of episodes vary widely among patients. Treatment approaches should include both nonpharmacologic and pharmacologic strategies.3 Patients and family members should be educated about bipolar disorder (e.g., symptoms, causes, and course) and treatment options. Long-term adherence to treatment is the most important factor in achieving stabilization of the disorder.
![]() The treatment of bipolar disorder can vary depending on what type of episode the patient is experiencing. Once diagnosed with bipolar disorder, patients should remain on a mood stabilizer (e.g., lithium, valproate) for their lifetime. During acute episodes, medications can be added and then tapered once the patient is stabilized and euthymic. For example, when treating a patient for mania with psychotic features, the patient should be on a mood stabilizer and an antipsychotic. If the antipsychotic is the patient’s maintenance therapy, the dose should be increased or perhaps the medication should be changed altogether if the patient goes into a manic episode. If treating a patient for a severe depressive episode, a clinician may need to maximize the dose of the mood stabilizer or add another medication (e.g., quetiapine).
The treatment of bipolar disorder can vary depending on what type of episode the patient is experiencing. Once diagnosed with bipolar disorder, patients should remain on a mood stabilizer (e.g., lithium, valproate) for their lifetime. During acute episodes, medications can be added and then tapered once the patient is stabilized and euthymic. For example, when treating a patient for mania with psychotic features, the patient should be on a mood stabilizer and an antipsychotic. If the antipsychotic is the patient’s maintenance therapy, the dose should be increased or perhaps the medication should be changed altogether if the patient goes into a manic episode. If treating a patient for a severe depressive episode, a clinician may need to maximize the dose of the mood stabilizer or add another medication (e.g., quetiapine).
Nonpharmacologic Therapy
The basics of nonpharmacologic approaches should address issues of adequate nutrition, sleep, exercise, and stress reduction.3 Sleep deprivation, high stress, and deficiencies in dietary essential amino acids, fatty acids, vitamins, and minerals can exacerbate mood episodes and result in poorer outcomes.3 Mood charting is an effective strategy in detecting early signs and symptoms of mania and depression. Another effective treatment is to combine medications with adjunctive psychoeducational programs, supportive counseling, insight-oriented psychotherapy (individual or group), couples or family therapy, cognitive behavioral therapy, and communication enhancement training.2,3,22,52
Pharmacologic Therapy
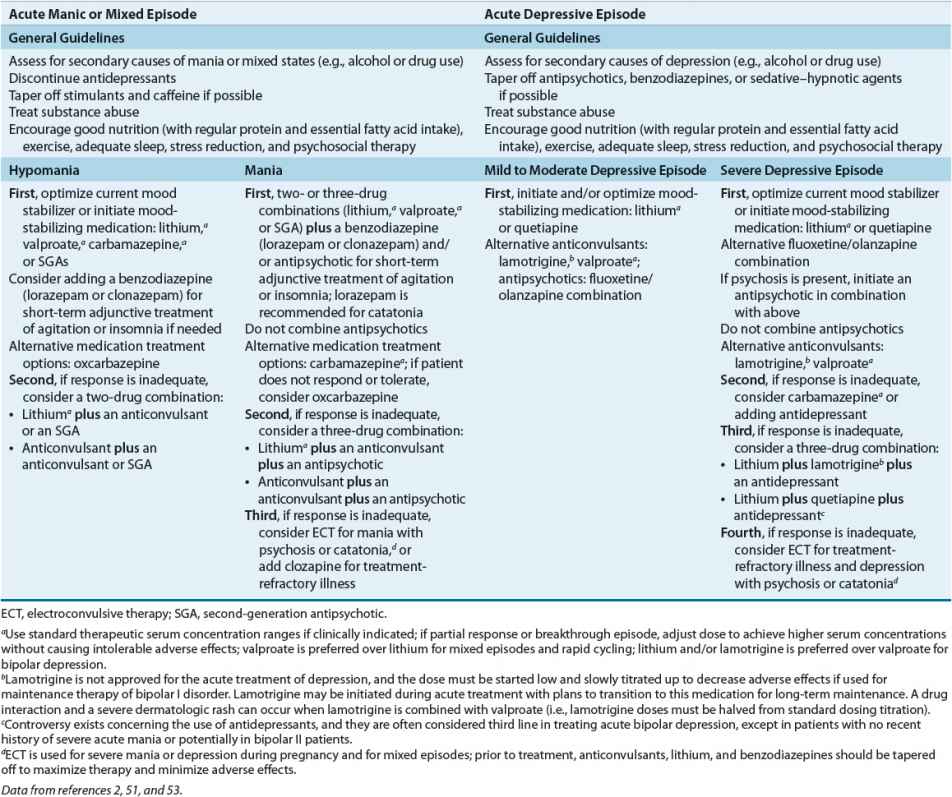
![]() Pharmacotherapy is crucial for the acute and maintenance treatment of bipolar disorder and includes lithium, valproate, carbamazepine, lamotrigine, first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs), and adjunctive agents such as antidepressants and benzodiazepines. General treatment guidelines for the acute treatment of mood episodes in patients with bipolar I disorder are found in Table 52-5.
Pharmacotherapy is crucial for the acute and maintenance treatment of bipolar disorder and includes lithium, valproate, carbamazepine, lamotrigine, first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs), and adjunctive agents such as antidepressants and benzodiazepines. General treatment guidelines for the acute treatment of mood episodes in patients with bipolar I disorder are found in Table 52-5.
TABLE 52-5 Algorithm and Guidelines for the Acute Treatment of Mood Episodes in Patients with Bipolar I Disorder
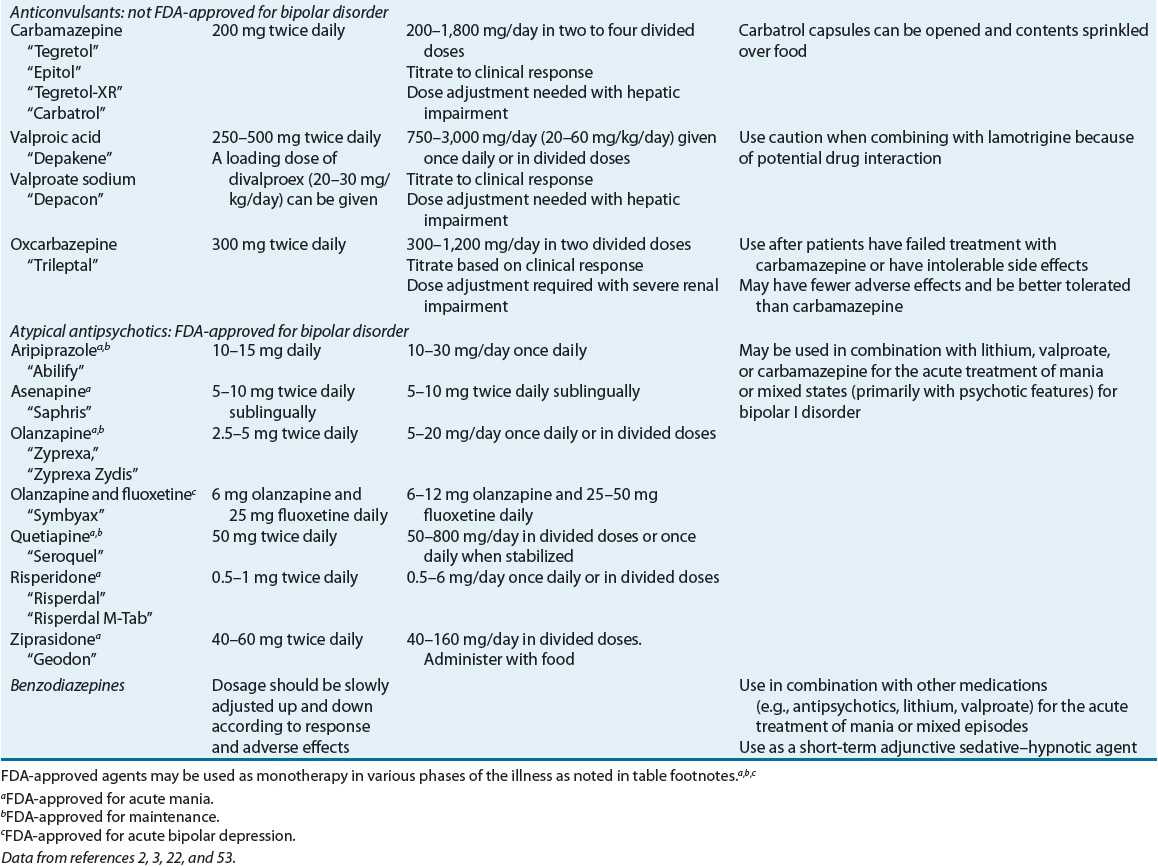
Product information, dosing, and administration of agents used in the treatment of bipolar disorder are found in Table 52-6.
TABLE 52-6 Products, Dosage and Administration, and Clinical Use of Agents Used in the Treatment of Bipolar Disorder
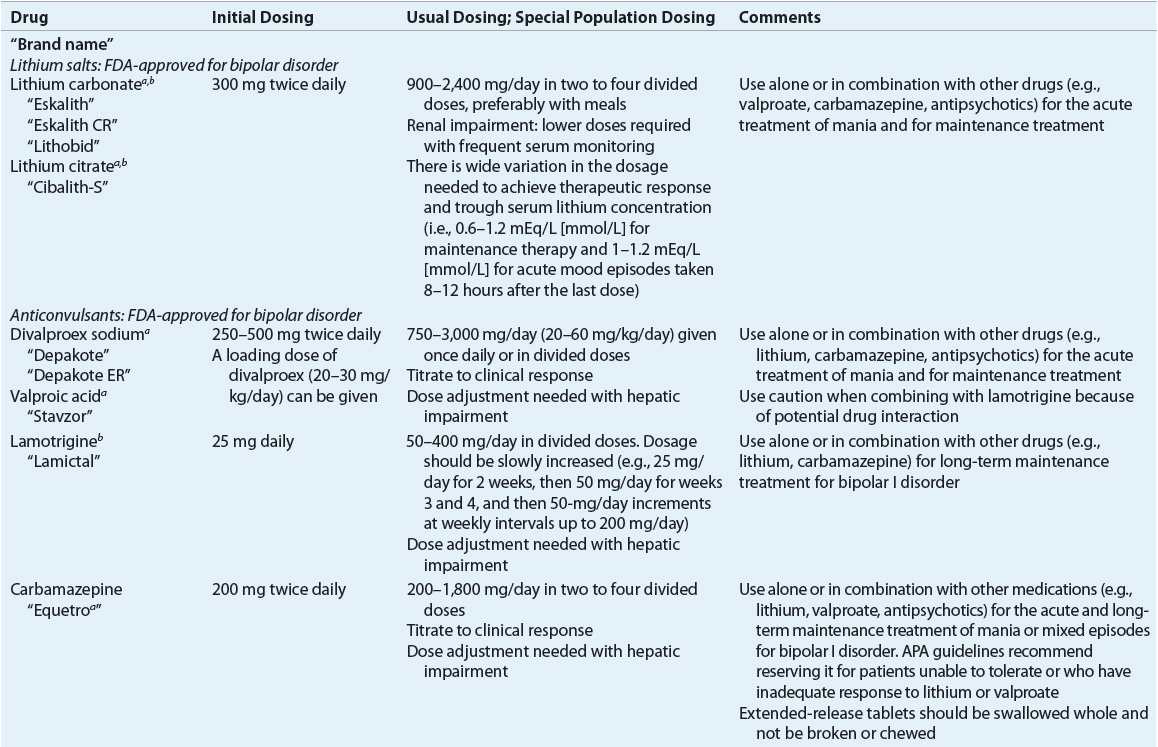
![]() The term mood stabilizer is often used to describe the class of medications used in the treatment of bipolar disorder, but this may not be accurate as some medications are more effective for acute mania, some for the depressive episode, and others for the maintenance phase.54 Lithium, valproate (or divalproex sodium), extended-release carbamazepine, aripiprazole, asenapine, olanzapine, quetiapine, risperidone, and ziprasidone are currently approved by the U.S. FDA for the treatment of acute mania in bipolar disorder; only lithium, divalproex sodium, aripiprazole, olanzapine, and lamotrigine are approved for the maintenance treatment of bipolar disorder. Quetiapine is the only monotherapy antipsychotic that is FDA-approved for bipolar depression. Lithium is the drug of choice for bipolar disorder with euphoric mania, whereas valproate has better efficacy for mixed states and irritable/dysphoric mania compared with lithium.2
The term mood stabilizer is often used to describe the class of medications used in the treatment of bipolar disorder, but this may not be accurate as some medications are more effective for acute mania, some for the depressive episode, and others for the maintenance phase.54 Lithium, valproate (or divalproex sodium), extended-release carbamazepine, aripiprazole, asenapine, olanzapine, quetiapine, risperidone, and ziprasidone are currently approved by the U.S. FDA for the treatment of acute mania in bipolar disorder; only lithium, divalproex sodium, aripiprazole, olanzapine, and lamotrigine are approved for the maintenance treatment of bipolar disorder. Quetiapine is the only monotherapy antipsychotic that is FDA-approved for bipolar depression. Lithium is the drug of choice for bipolar disorder with euphoric mania, whereas valproate has better efficacy for mixed states and irritable/dysphoric mania compared with lithium.2
Combination therapies (e.g., lithium plus valproate or carbamazepine; lithium or valproate plus a SGA) can provide better acute response and long-term prevention of relapse and recurrence than monotherapy in some bipolar patients, particularly those with mixed states or rapid cycling.2,54 The majority of patients hospitalized for an acute episode will be on combination therapy.
Several guidelines and algorithms have been published regarding the treatment of bipolar disorder, and these are generally based on the best available data and clinical consensus of experts. The Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) published updated treatment guidelines in 2009.53 In addition, an international task force of the World Federation of Societies of Biological Psychiatry (WFSBP) has published guidelines for the treatment of acute bipolar depression and mania.55,56 The WFSBP mania and depression guidelines were updated in 2009 and 2010, respectively; maintenance (2003) guidelines have yet to be updated.
Based on the CANMAT and ISBD guidelines and available research, an example treatment algorithm and guidelines for acute mood episodes in adult patients with bipolar I disorder are listed in Table 52-5. Because newer anticonvulsants, SGAs, and combination therapies are under investigation for bipolar disorder, published guidelines, algorithms, and decision trees can quickly become out of date as new scientific knowledge evolves. Selection of treatments for acute mood episodes (e.g., manic or mixed, depressive, or rapid cycling) and for maintenance strategies to prevent relapses of mood episodes should be individualized. Treatment plans should be based on patient-specific characteristics, comorbid psychiatric and medical conditions, and avoidance of drug interactions and adverse effects.2
Specific Pharmacologic Therapies
Lithium Lithium was first used in 1949 as a treatment for mania and was approved in 1972 in the United States for the treatment of acute mania and for maintenance therapy. Despite numerous investigations into the biologic and clinical properties of lithium, there is no unified theory for its mechanism of action.22,57–59 Chronic lithium administration may modulate gene expression and have neuroprotective effects. Lithium has unique pharmacokinetics because it is a monovalent cation. It is rapidly absorbed, is widely distributed with no protein binding, is not metabolized, and is excreted unchanged in the urine and in other body fluids.60
Efficacy Lithium was the first established mood stabilizer, and is still considered a first-line agent for acute mania, acute bipolar depression, and maintenance treatment of bipolar I and II disorders.53 Early placebo-controlled studies with lithium reported up to a 78% response rate in aborting an acute manic or hypomanic episode, but more recent studies suggest a slower onset of action and a more moderate effectiveness when compared with other agents.2,3,61 In placebo-controlled studies in bipolar depression, lithium has been found to have efficacy, but there can be a 6- to 8-week delay for its antidepressant effects.2 Lithium is more effective for pure or elated (classic) mania, and can be less effective for mania with psychotic features, mixed episodes, rapid or continuous cycling, alcohol and drug abuse, and in organic-induced mood states.2,3,62
Long-term lithium therapy is more effective in patients with fewer prior episodes, with a history of euthymia or good functioning between episodes, and with a family history of bipolar illness with a positive response to lithium. Lithium produces a prophylactic response in up to two thirds of patients and reduces suicide risk by 8- to 10-fold.2,61–63
Clinical Controversy
Patients maintained on standard serum concentrations of lithium (0.8 to 1 mEq/L [mmol/L]) may have fewer relapses than patients maintained on lower serum concentrations (0.4 to 0.6 mEq/L [mmol/L]).2,3 Abrupt discontinuation or noncompliance with lithium therapy can increase the risk of relapse.2,3 Discontinuation-induced refractoriness has been reported in approximately one fifth of patients who previously were stabilized on lithium.2,3
Lithium augmentation of carbamazepine, lamotrigine, and valproate can improve treatment response in bipolar I disorder.2,64 Concomitant use of lithium with valproate or carbamazepine appears to be well tolerated but can increase the risk of sedation, weight gain, GI complaints, and tremor.
Lithium is frequently combined with either FGAs or SGAs for treatment of euphoric acute mania with psychotic features. Case reports of neurotoxicity (e.g., delirium, cerebellar dysfunction, extrapyramidal symptoms, and severe tremors) have been published in elderly patients receiving lithium and FGAs.60 Combining lithium with calcium channel blockers is not recommended because of reports of neurotoxicity and severe bradycardia with verapamil or diltiazem.60 Acute neurotoxicity and delirium have been reported in patients receiving electroconvulsive therapy (ECT) with lithium (even at reduced dosages); therefore, lithium should be withdrawn and discontinued at least 2 days before ECT and should not be resumed until 2 to 3 days after the last treatment.
Adverse Effects Approximately 35% to 93% of patients treated with lithium will experience adverse effects. These are divided into those that occur early in therapy but are generally innocuous and transient, those that occur with long-term therapy and are usually not dose-related, and toxic effects that occur with high serum concentrations.2,60
Initial side effects are often dose-related and are worse at peak serum concentrations (1 to 2 hours postdose).2 Standard approaches for minimizing adverse effects include lowering the dose, taking smaller doses with food, using extended-release products, and trying once-daily dosing at bedtime.2 GI distress (e.g., nausea, vomiting, dyspepsia, and diarrhea) can be minimized by the standard approaches or by adding antacids or antidiarrheal agents.2 Diarrhea can sometimes be managed by switching from tablet or capsule formulation to liquid formulation. Diarrhea produced by lithium is commonly an osmotic diarrhea, and therefore switching to a formulation that clears the gut quickly can ameliorate symptoms. Muscle weakness and lethargy develop in about 30% of patients, but these symptoms are usually transient. Polydipsia with polyuria and nocturia occurs in up to 70% of patients and can be managed by changing to once-daily bedtime dosing.
A fine hand tremor can be evident in up to 50% of patients. Stress, concomitant use of antidepressants or antipsychotics, caffeine, sympathomimetics, and impending toxicity can exacerbate the tremor. Strategies to reduce the tremor include standard approaches (e.g., switch to long-acting preparation, lower dose if possible) or adding a β-adrenergic antagonist (e.g., propranolol 20 to 120 mg/day).
Lithium reduces the kidney’s ability to concentrate urine and can cause a nephrogenic diabetes insipidus characterized by low urine specific gravity and a low osmolality polyuria (urine volumes greater than 3 L/day).2,60 Lithium-induced nephrogenic diabetes insipidus is treated with loop diuretics, thiazide diuretics, or triamterene. If a thiazide diuretic is used (e.g., hydrochlorothiazide 50 mg/day), lithium doses should be decreased by 50%, and potassium levels should be monitored.2 Amiloride, a potassium-sparing diuretic, has weaker natriuretic effects than thiazides and appears to be relatively safe with minimal effect on lithium clearance. Potassium supplements have been suggested as another treatment for lithium-induced polyuria.22 Fluid restriction is not recommended because dehydration increases the risk of lithium toxicity. If edema occurs, treatment approaches include lowering sodium intake or using a diuretic (e.g., spironolactone); close monitoring for lithium toxicity is necessary because these treatments often increase lithium concentrations.
Patients on long-term lithium therapy have a 10% to 20% risk of developing morphologic renal changes (e.g., glomerular sclerosis, tubular atrophy, and interstitial nephritis) that is associated with impairment of water resorption and increased serum creatinine concentrations.2 Lithium rarely causes nephrotoxicity if patients are maintained on the lowest effective dose, if once-daily dosing is used, if adequate hydration is maintained, and if toxicity is avoided.22 Lithium should be avoided in patients with preexisting renal disease unless there is frequent monitoring.
Lithium is concentrated in the thyroid gland, interferes with thyroid hormone synthesis, and can induce the formation of thyroid antibodies.60 Up to 30% of patients on maintenance lithium therapy develop transiently elevated thyroid-stimulating hormone concentrations, and 5% to 35% of patients develop a goiter and/or hypothyroidism.2 Lithium-induced hypothyroidism is not dose-related, is observed 10 times more frequently in women (particularly in those with rapid cycling), and usually occurs after 6 to 18 months of therapy.2 Hypothyroidism does not require discontinuation of lithium, because exogenous thyroid hormone (i.e., levothyroxine) can be added to the regimen. When lithium is discontinued, the need for exogenous thyroid hormone should be reassessed, because hypothyroidism can be reversible.
Lithium can cause a variety of benign and reversible cardiac effects, particularly T-wave flattening or inversion (in up to 30% of patients), atrioventricular block, and bradycardia.2,22,60 If a patient has significant preexisting cardiac disease, consultation with a cardiologist and an electrocardiogram is recommended at baseline and during lithium therapy.
Other late-appearing lithium side effects include benign reversible leukocytosis and a variety of dermatologic effects (e.g., acne and acneiform eruptions, exacerbation of psoriasis, pruritic dermatitis).3 Weight gain is common (~20% of patients gain >10 kg [22 lb]) and can be related to fluid retention, the consumption of high-calorie beverages as a result of polydipsia, or a decreased metabolic rate because of hypothyroidism.22,62 Severe neurologic disturbances such as coarse hand tremors, ataxia, slurred speech, myasthenia gravis, extrapyramidal syndrome, pseudotumor cerebri, and papilledema are occasionally observed.
Lithium is an extremely toxic drug if accidentally or intentionally taken in overdose. Lithium toxicity can occur with blood levels greater than 1.5 mEq/L (mmol/L), but elderly patients can have symptoms of toxicity at therapeutic levels.2 Severe lithium intoxication occurs when concentrations are higher than 2 mEq/L (mmol/L), and there is a worsening in several key symptoms: GI (e.g., vomiting, diarrhea, or incontinence), coordination (e.g., severe fine to coarse hand tremor, unstable gait, slurred speech, and muscle twitching), and cognition (e.g., poor concentration, drowsiness, disorientation, apathy, and coma).2 Several reports of seizures, cardiac dysrhythmia, permanent neurologic impairments with ataxia and deficits in memory, and kidney damage with reduced glomerular filtration rate have been reported after lithium intoxication.2
Situations that predispose patients to lithium toxicity include sodium restriction, dehydration, vomiting, diarrhea, age greater than 50, heart failure, cirrhosis, and drug interactions that decrease lithium clearance. Heavy exercise, sauna baths, hot weather, and fever can promote sodium loss. Patients should be cautioned to maintain adequate sodium and fluid intake (2.5 to 3 qt [~2.5 to 3 L] per day of fluids) and to avoid the excessive use of coffee, tea, cola, and other caffeine-containing beverages and alcohol.
If lithium toxicity is suspected, the person should go to an emergency room to be monitored, and lithium should be discontinued.2 Gastric lavage and IV fluids may be needed, and the patient should be monitored for fluid balance, renal and electrolyte status, and neurologic changes. When lithium concentrations are above 3.5 to 4 mEq/L (mmol/L), intermittent hemodialysis (12 hours on and 12 hours off) can be started and continued until the lithium concentration is below 1 mEq/L (mmol/L) when taken 12 hours after the last dialysis.
Drug–Drug Interactions Thiazide diuretics, nonsteroidal antiinflammatory drugs, cyclooxygenase-2 inhibitors, angiotensin-converting enzyme inhibitors, and salt-restricted diets can elevate lithium levels.2 Neurotoxicity can occur when lithium is combined with carbamazepine, diltiazem, losartan, methyldopa, metronidazole, phenytoin, and verapamil.2,60 Analgesics such as acetaminophen or aspirin and loop diuretics are less likely to interfere with lithium clearance. Caffeine and theophylline can enhance the renal elimination of lithium. Because lithium has no effect on hepatic metabolizing enzymes, it has fewer drug–drug interactions compared with carbamazepine, oxcarbazepine, and valproate.
Dosing and Administration Lithium dosing depends on the patient’s age and weight, tolerance to adverse effects, and the acuity of the illness. Dosing is generally titrated up to achieve steady-state serum lithium concentrations of 0.6 to 1.2 mEq/L (mmol/L).2 Lithium therapy is usually initiated with low to moderate doses (600 mg/day) for prophylaxis and higher doses (900 to 1,200 mg/day) for acute mania, using a two- to three-times daily dosing regimen.2,60 Immediate-release lithium preparations should be given in two or three divided daily doses, whereas extended-release products can be given once or twice daily. In clinical practice many clinicians dose the immediate-release and extended-release preparations once daily. It can be best to initially begin a patient on divided dosing, but once stabilized many patients are able to switch to once-daily dosing without decompensating.
Lithium levels are considered to be at steady state at approximately day 5, and serum samples should be drawn 12 hours postdose. Once a desired serum concentration has been achieved, levels should be drawn in 2 weeks and then if stable every 3 to 6 months or as clinically indicated. Maintenance lithium serum concentrations are usually measured every 3 months, but can be adjusted to every 6 months for stabilized patients, and every 1 to 2 months for patients with frequent mood episodes.2 Lithium clearance rates increase by 50% to 100% during pregnancy and return to normal postpartum; thus, lithium levels should be determined monthly during pregnancy and weekly the month before delivery. At delivery, rapid fluid changes can significantly increase lithium levels; thus, a reduction to prepregnancy lithium doses and adequate hydration are recommended.2
The recommended guidelines for baseline and routine laboratory testing for lithium are listed in Table 52-7. The dose should be adjusted based on the steady-state serum concentration drawn 12 hours (±30 minutes) after the last dose.61 A therapeutic trial for outpatients should last a minimum of 4 to 6 weeks with lithium serum concentrations of 0.6 to 1.2 mEq/L (mmol/L). Acutely manic patients can require serum concentrations of 1 to 1.2 mEq/L (mmol/L), and some need up to 1.5 mEq/L (mmol/L) to achieve a therapeutic response. Although serum concentrations less than 0.6 mEq/L (mmol/L) are associated with higher rates of relapse, some patients can do well at 0.4 to 0.7 mEq/L (mmol/L).2 For bipolar prophylaxis in elderly patients, serum concentrations of 0.4 to 0.6 mEq/L (mmol/L) are recommended because of increased sensitivity to adverse effects.2
TABLE 52-7 Guidelines for Baseline and Routine Laboratory Tests and Monitoring for Agents Used in Treatment of Bipolar Disorder