Biochemistry
GENERAL PRINCIPLES
Describe the general steps of protein synthesis:
- DNA transcribed into mRNA
- mRNA modified and/or translated into a peptide
- Protein folding
- Post-translational modification
What is the significance of the R-group of an amino acid?
Amino acids present in proteins in humans are classified by their R-group, which is the unique functional side-chain moiety. The physical and chemical properties of the R-groups (aliphatic, aromatic, neutral polar, acidic, basic, or sulfur-containing) will influence protein solubility as well as stabilize tertiary protein structure. R-groups also play an important role as buffers by accepting protons under more acidic conditions and donating protons under more basic conditions.
What is an enzyme? What do enzymes do?
An enzyme is a protein that functions to accelerate the rate of a biological reaction by decreasing the activation energy of the reaction. Regulation of enzyme activity allows for adaptation to changing physiologic conditions.
What parameters can influence enzymatic reactions?
Enzyme activity can be affected by changes in temperature, salinity, pH, active site structure, and the presence of competitive and noncompetitive inhibitors.
What are the differences between competitive and noncompetitive enzyme inhibition?
Competitive inhibitors bind reversibly to the active site while noncompetitive inhibitors may bind the active site or distant sites. Competitive inhibition can be overcome by high substrate concentrations whereas noncompetitive inhibition cannot.
What are the general mechanisms of enzyme regulation?
Gene transcription controlling protein synthesis; activation or inactivation by proteolytic enzymes; activation or inactivation by covalent modification (phosphorylation); allosteric regulation by small molecules binding sites distant from the active site; degradation of enzymes by intracellular proteases or in proteasomes
What enzymes participate in DNA replication?
DNA polymerase, DNA ligase, primase
What is the name given to segments of DNA which are spliced out of primary mRNA transcripts?
Introns
Give examples of posttranscriptional RNA modification:
5′ capping, 3′ poly-A tail, splicing
What is a Southern blot?
A technique where electrophoresed DNA is transferred to a membrane, which is probed with a “reporter” – labeled DNA sequence. The hybridized membrane is exposed to film to determine the specific size of the targeted DNA (eg, to identify restriction fragment length polymorphisms).
What is a Northern blot?
A technique where electrophoresed RNA is transferred to a membrane, which is probed with a “reporter” – labeled DNA sequence. The hybridized membrane is exposed to film to determine if the size of the RNA transcript on the membrane corresponds to the size of a specific known gene transcript in order to measure expression levels of that gene.
A technique where electrophoresed protein is transferred to a membrane, which is probed with a “reporter” – labeled antibody. The hybridized membrane is exposed to film to determine if the size of the targeted protein corresponds to the size of a specific known protein in order to measure expression levels of that gene.
What is enzyme-linked immunosorbent assay (ELISA)?
A technique which uses antigen or antibody coupled with a chromogen-tagged enzyme to detect the presence of an antibody or antigen, respectively, in a test sample.
Describe the role of cell membranes in signal transduction:
Cell membranes are the physical barrier that serves to maintain ionic concentration gradients which facilitate nerve conduction as well as facilitated diffusion and active transport of molecules. Cell membranes also contain integral and transmembrane proteins which directly transport signal molecules or which may be involved in second messenger pathways.
What are the intracellular concentrations of Na+, K+, and Ca2+?
K+ is the predominant intracellular ion (140 mEq) while Na+ (10 mEq) and Ca2+ (1-2 mEq) are less concentrated.
What are the extracellular concentrations of Na+, K+, and Ca2+?
Na+ is the predominant extracellular ion (140 mEq) while K+ (5 mEq) and Ca2+ (10−4mEq) are less concentrated.
How are substances transported across biomembranes?
Substances are transported either via diffusion (simple or facilitated) or by active transport (primary or secondary). The important difference between these two processes is that active transport requires energy input by hydrolysis of ATP whereas diffusion requires no energy input.
What is the difference between simple diffusion and facilitated diffusion?
Simple diffusion is driven by the concentration gradient of the molecule that is moving across the membrane. Due to the nature of the lipid bilayer of cell membranes, molecules that are capable of diffusion are small and hydrophobic. Facilitated diffusion is driven by the electrochemical gradient across the membrane.
What is the difference between primary and secondary active transport?
Primary active transport relies on energy released from hydrolysis of ATP by ATPases in cell membranes to move ions and other molecules across cell membranes. Secondary active transport utilizes the electrochemical gradient established by primary active transport to move larger molecules (ie, sugars and amino acids) across cell membranes.
What is the biochemical significance of albumin?
Albumin has several important biochemical roles. It serves as a marker of nutritional depletion, is an osmotic regulator of fluid shifts between intravascular and extravascular spaces, and also functions as a transport protein. Albumin is a small, highly polar molecule, which at physiologic pH has a high capacity for nonspecific binding of ligands (ie, drugs) and for buffering changes in pH by binding protons.
In what clinical situations would a patient’s caloric needs be increased?
Extensive burns, pregnancy, increased physical activity level, postsurgery, or posttrauma
What is the purpose of glycolysis?
To anaerobically metabolize glucose to produce ATP as well as to create substrates for other biochemical pathways (ie, pentose phosphate pathway) and, especially in RBCs, to create 2,3-bisphosphoglycerate which regulates the affinity of oxygen for hemoglobin
What is the purpose of the tricarboxylic acid (TCA) cycle?
In cells that have mitochondria, the TCA cycle uses fat, carbohydrate, and protein substrates to produce reduced coenzymes (FADH2 and NADH) which are used in the generation of ATP in the electron transport chain. The TCA cycle does not use oxygen in any of its reactions, but it requires oxygen for reoxidation of reduced coenzymes. The TCA cycle is also involved in the production of substrates for storage molecules.
What is the purpose of the electron transport chain?
To produce ATP via a series of redox reactions using NADH and FADH2produced in the TCA cycle
What is gluconeogenesis and where does it occur?
Gluconeogenesis is a metabolic pathway that produces glucose from pyruvate. It can occur only in the liver, kidney, and intestinal epithelium.
What is the pentose phosphate shunt and where does it occur?
The pentose phosphate shunt is a metabolic pathway that produces ribose-5-phosphate to be used in nucleotide synthesis and NADPH to be used in fatty acid and steroid biosynthesis. This pathway occurs in the liver, adrenal cortex, and lactating mammary glands.
Which proteins are involved in movement of oxygen within the human body?
Hemoglobin is a protein responsible for oxygen transport and is found exclusively in RBCs. Myoglobin is a protein that stores oxygen in the cytoplasm of skeletal and striated muscle cells and delivers it when needed to mitochondria.
Which are considered to be “normal” variants of hemoglobin?
Adult hemoglobin is mostly HbA (α2β2) and a small percentage (4%) HbA2 (α2γ2). Fetal hemoglobin is a normal hemoglobin during fetal life and comprises <1% of adult hemoglobin.
Give examples of common pathologic hemoglobin variants:
Hemoglobin S, hemoglobin C, and hemoglobin E
What parameters influence the degree of oxygen saturation of hemoglobin?
The oxygen affinity for hemoglobin is regulated by [H+], [CO2], [2,3-BPG], temperature, and metabolic needs of the tissue.
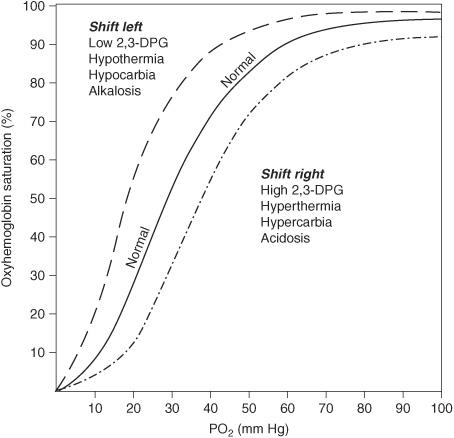
Figure 2.1 Oxygen dissociation curves.
DNA/RNA/PROTEIN PATHOLOGY
What autosomal recessive disorder results in the inability to repair thymidine dimers which form in DNA after exposure to UV light?
Xeroderma pigmentosum
What is the common abnormality in lysosomal storage diseases?
A deficiency in a lysosomal enzyme which leads to accumulation of the enzyme’s substrate in various tissues in the body (eg, Gaucher disease “crumpled tissue paper cells”)
Which vitamin is required for collagen synthesis?
Vitamin C
What syndrome is the result of defective collagen synthesis causing hyperextensible skin, hypermobile joints, and a tendency to bleed?
Ehlers-Danlos syndrome, also associated with the presence of berry aneurysms
In what syndrome is defective collagen (type I) synthesis associated with blue sclerae and multiple bone fractures due to minimal trauma?
Osteogenesis imperfecta
Which syndrome is associated with long limbs, kyphosis, cardiac abnormalities, and a mutation of the fibrillin gene?
Marfan syndrome
NUTRITIONAL DISORDERS
What is marasmus?
A nutritional deficiency of both total calories and protein
What age group is usually affected by marasmus?
Children less than 1 year
What is kwashiorkor?
A nutritional protein deficiency in the setting of adequate total calorie intake
What are the distinguishing features of kwashiorkor?
Malabsorption (atrophy of intestinal villi); Edema—most important; Anemia; Liver is fatty; Subcutaneous layer still present
*K washiorkor lacks MEALS with protein
What is the significance of the edema seen in kwashiorkor?
Due to protein deficiency and decreased oncotic pressure
What dermatologic findings are associated with kwashiorkor?
Depigmented bands in hair and skin
VITAMINS AND MINERALS
Which are the fat-soluble vitamins?
Vitamins A, D, E, K
*KADE
Why are fat-soluble vitamins potentially toxic?
Fat-soluble vitamins accumulate in body fat stores. This can lead to toxic blood levels of a substance and with additional redistribution of fat-stored substance into the blood; toxic levels are not easily correctable.
What are the symptoms associated with vitamin A deficiency?
Ocular abnormalities—xerophthalmia, night blindness, and keratomalacia (corneal softening); squamous metaplasia of respiratory tract
Describe the role vitamin A plays in producing vision:
Rhodopsin is a visual pigment found in rod cells of the retinal which contains vitamin A, specifically in the form of 11-cis-retinal. With light, 11-cis-retinal is converted to all-trans retinal which initiates transduction of a nerve impulse in the optic nerve.
Briefly describe the metabolic pathway by which vitamin A is obtained from the diet:
Vitamin A is found in animal products in the form of retinol, retinal, and retinoic acid. The provitamin form, β-carotene, is found in plant products. β-Carotene is metabolized to all-trans retinol by β-carotene dioxygenase in the small bowel. Retinol and retinoic acid are stored in the liver as retinol palmitate.
What foods contain high amounts of vitamin A in the form of retinoids?
Liver; egg yolk; butter
What foods contain β-carotene?
Carrots; leafy green vegetables
What are the changes seen in hypervitaminosis A?
Alopecia; liver damage; bone changes
What is the role of vitamin K in clotting cascades?
Vitamin K is necessary for the carboxylation of glutamyl residues in the synthesis of activated clotting factors.
Vitamin K is used for the production of which clotting factors?
Factors II, VII, IX, and X, protein C and protein S
Why are newborn infants susceptible to vitamin K deficiency?
Placental transfer of vitamin K is very limited and the fetal liver does not store significant quantities. Breast milk is a good source of vitamin K. Most infants born in hospitals are given vitamin K at birth as prophylaxis.
How do children and adults get vitamin K?
Dairy products; yellow and green vegetables; synthesized by intestinal flora
What does deficiency of vitamin E cause?
Erythrocyte fragility (hemolysis)
What symptoms are caused by vitamin D deficiency?
Rickets; Osteomalacia; Tetany (hypocalcemia)
*Bones ROT without vitamin D
What is an important source of vitamin D?
Milk and dairy products
What occurs with an excess of vitamin D?
Hypercalcemia—vitamin D regulates calcium absorption in the gut and bone reabsorption. Hypercalcemia may result in hypercalciuria and nephrolithiasis.
What are the symptoms of hypercalcemia?
Bone pain; kidney stones; constipation; central nervous system (CNS) symptoms—depression, confusion, stupor
*Stones, bones, groans (abdominal pain), and psychiatric overtones
Which form of vitamin D is the active form?
1,25-Dihydroxycholecalciferol (1,25-(OH)2 D3)
Which form is the storage form of vitamin D?
25-Hydroxycholecalciferol(25-OHD3)
Which form of vitamin D is consumed in milk?
D2 (ergocalciferol)
Which form of vitamin D is formed by sun exposure on skin?
D3 (cholecalciferol)
How does sarcoidosis affect vitamin D metabolism?
In sarcoidosis, epithelioid macrophages contribute to increased conversion to activated vitamin D leading to hypercalcemia.
Which are the water-soluble vitamins?
B vitamins; vitamin C; folic acid
Which are the B complex vitamins?
B1 B2, B3, B5, B6
*All Bs except 12
What food sources contain the B complex vitamins?
Leafy green vegetables; whole grain cereals; animal products: meat, fish, and dairy
What is the psychiatric syndrome of Bj deficiency?
Wernicke-Korsakoff syndrome
What is the usual setting for Wernicke-Korsakoff syndrome?
Alcoholics with malnutrition (lacking B1)
What are the characteristic findings of a Wernicke triad?
Mental confusion; Ophthalmoplegia/N ystagmus; Ataxia
*Wernicke patients MOAN
What symptom is characteristic of a Korsakoff psychosis?
Confabulation
What degenerative changes are seen in the brains of patients with Wernicke-Korsakoff?
Hemorrhagic lesions of mamillary bodies and paramedian gray matter
What cardiac syndrome is associated with B1 deficiency?
Wet beriberi
What is wet beriberi?
Fluid retention associated with myocardial dysfunction (high-output cardiac failure)
What type of cardiomyopathy is associated with wet beriberi and thiamine deficiency?
Dilated cardiomyopathy
What is dry beriberi (also due to thiamine [B1] deficiency)?
Peripheral neuropathy and atrophy of extremities
What biochemical pathways use B1 as a cofactor?
Oxidative carboxylation for α-keto acids (pyruvate and a-ketoglutarate); transketolase in hexose monophosphate (HMP) shunt
What biochemical pathway uses riboflavin?
Oxidation and reduction using flavin adenine dinucleotide (FAD) and flavin mononucleotide (FMN)
*2F s go with riboflavin (B2)
What is the triad of dermatitis, dementia, and diarrhea called?
Pellagra (eg, Niacin deficiency)
What are the biochemical pathways that use niacin (B3)?
Reduction and oxidation reactions with nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP)
*N reactions go with Niacin
What diseases can cause B3 deficiency and symptoms of pellagra?
Hartnup disease because of inadequate tryptophan absorption in the gut and inadequate reabsorption in the renal tubules; carcinoid syndrome because tryptophan is being used by the tumor to synthesize serotonin instead of niacin.
What is the biochemical function of vitamin B5?
Fatty acid synthesis—part of coenzyme A (CoA)
What antituberculosis medication predisposes to vitamin B6 deficiency?
Isoniazid (INH)
What biochemical pathways need vitamin B6?
γ-Aminobutyric acid (GABA) production (neurotransmitter); transamination cofactor; decarboxylation reaction cofactor
What food products contain cobalamin?
Animal products contain cobalamin, but it is exclusively synthesized by bacteria. Cobalamin is not present in plant products.
What is a likely cause of the vitamin B12 deficiency in a Japanese immigrant?
Diphyllobothrium latum (fish tapeworm)
What are the causes of B12 deficiency?
Vegan diet; D. latum; pernicious anemia; Crohn disease (terminal ileum)
What causes cobalamin deficiency in pernicious anemia?
Lack of intrinsic factor
Which test localizes cobalamin (B12) deficiency?
Shilling test
*12 Cobalt colored shillings
What biochemical pathways require vitamin B12?
Homocysteine methylation to methionine; methylmalonyl-CoA to succinyl-CoA
What neurologic complication may result from B12 deficiency?
Abnormal myelin production
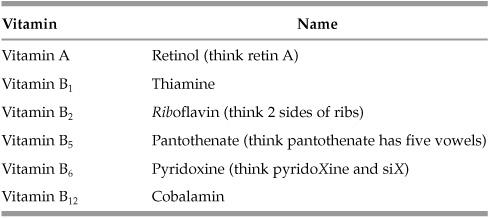
Table 2.1 Vitamin Review
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


