Benign Metastasizing Leiomyoma
Key Facts
Clinical Issues
30-50 years of age
Exclusively observed in women
Lesions are usually multiple and may be bilateral, suggesting metastatic disease
Macroscopic Features
Well-circumscribed, tan-white nodule
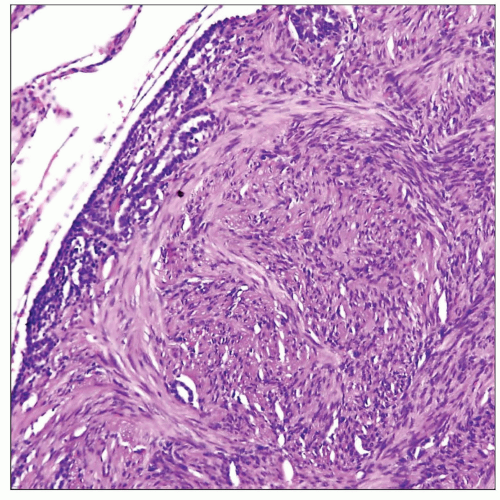
Microscopic Pathology
Fascicles of monotonous, bland-appearing spindle cells that are sharply separated from the surrounding lung parenchyma
Lesions may entrap normal respiratory mucosa and airspaces in the vicinity of the lesions (adenomyomatous hamartoma)
Spindle cells have blunt-ended nuclei showing dispersed chromatin pattern and small or inconspicuous nucleoli
Spindle cells are surrounded by a scant rim of fibrillary eosinophilic cytoplasm
No evidence of nuclear pleomorphism, mitoses, or tumor cell necrosis
Ancillary Tests
Spindle cells are positive for smooth muscle actin (SMA), desmin, calponin, and H-caldesmon
Stain positive with Bcl-2 (a feature shared with müllerian-derived smooth muscle)
May show expression of estrogen and progesterone receptors
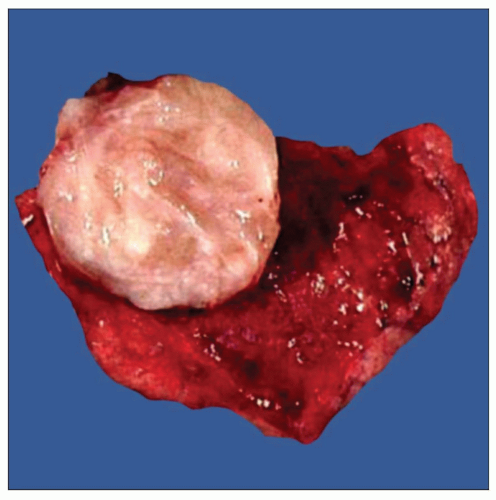 Gross appearance of benign metastasizing leiomyoma of the lung in a 50-year-old woman shows a well-circumscribed, fleshy nodule that bulges above the cut surface. |
TERMINOLOGY
Abbreviations
Benign metastasizing leiomyoma (BML)
Synonyms
Adenomyomatous hamartoma
Definitions
Benign smooth muscle proliferation of the lung arising in women with history of previously resected uterine leiomyoma
ETIOLOGY/PATHOGENESIS
Pathogenesis
Remote implantation of benign cells released into circulation during surgery
True metastases from very low-grade, well-differentiated leiomyosarcomas
Recent studies have demonstrated a clonal origin by molecular-genetic analysis
CLINICAL ISSUES
Epidemiology
Incidence
Very rare condition
Age
30-50 years of age
Gender
Exclusively observed in women
Site
No site predilection in the lungs
Lesions are usually multiple and may be bilateral, suggesting metastatic disease
Presentation
Mostly asymptomatic and discovered incidentally on chest x-rays
Natural History
Lesions may regress spontaneously or following hormonal manipulation
Growth of nodules typically ceases with onset of menopause
Nodules may be discovered after removal of uterine leiomyomas or concurrent with them
Treatment
Surgical approaches
Nodulectomy or lobectomy, depending on size of lesion
Hormonal therapy
Prognosis
Excellent prognosis following surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree