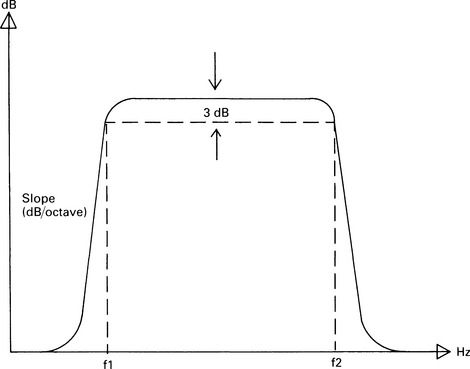
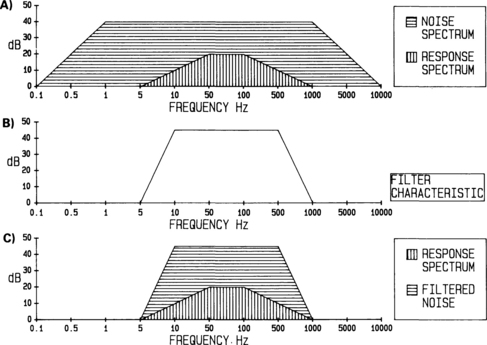
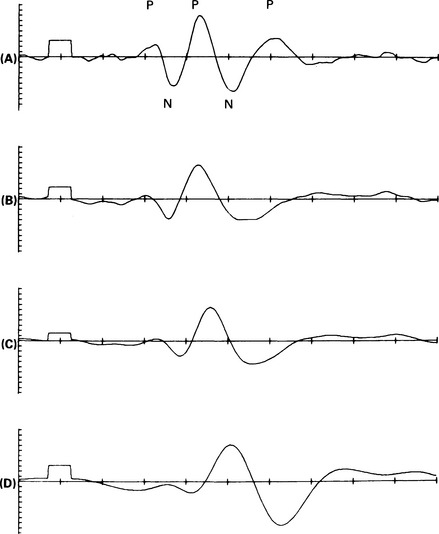
3 The electrode contact with the skin should be tested with an alternating-current impedance meter. This measure is one that varies with the frequency at which it is taken, and so a ‘good contact’ can be represented by an impedance of 2000 Ω measured at 1000 Hz, or by an impedance of 4000 Ω measured at 20 Hz. Both of these figures can represent the same degree of contact between the electrode and the skin. It is important, therefore, to be aware of the frequency at which the impedance meter tests the electrodes. Many commercial systems have built-in impedance meters, and, in general, these use a frequency of around 50 Hz. For reasons that will be given in the next section, it is important that the impedances of each electrode pair should be as similar as possible. It is better to achieve balanced impedances than to have only one electrode with a very low impedance. Direct-current test meters should never be used to measure electrode contact. This can polarize the electrodes, adding to the noise they produce, and, more significantly, currents in excess of the present safety limits could be passed through the patient. It is common practice to place the recording electrodes in the standard position defined by the international 10–20 system for electroencephalography (Jasper 1958). Currently, there is no generally accepted form for presenting the waveform recorded from an electrode pair. For many of the auditory-evoked potentials, both electrodes are ‘active’ and will register some of the response. The choice of which electrode represents the positive input to the amplifier is therefore an arbitrary one, and examples of both the possible waveform polarities may be found in the literature. It should be recognized that changes in electrode position can result in changes in waveform morphology, latency, and amplitude. The electrode/skin junction provides a capacitive connection between the signal generated on the scalp and that passed to the differential amplifier. This capacitance, combined with the input impedance of the differential amplifier, can create a filter which will distort the recorded waveform. To ensure that any such distortion occurs only at a frequency that is outside the frequency range of the response, the input impedance of the amplifier should be very high; generally, of the order of 10 MΩ. A filter, as its name implies, is a device which permits some frequencies to pass through unattenuated while filtering out others. A band-pass filter is one that will allow through frequencies lying within a certain range. The high and low cut-off frequencies of the band are described by the frequency at which the attenuation of the filter has reached 3 dB. Figure 3.1 shows a typical band-pass filter characteristic. The lower cut-off frequency is marked as f1, and the higher as f2. For frequencies lower than f1 or higher than f2, an increasing amount of attenuation is created by the filter. The steepness of the filter characteristic in these regions is known as the filter slope and is expressed in dB/octave. Fig. 3.1 A band-pass filter transfer function. Gain, in dB, is shown on the vertical axis and frequency on the horizontal axis. The ‘3-dB-down’ cut-off points are shown for the lower frequency (f1) and the higher frequency (f2). The slope of the skirts of the filter is measured in dB/octave. In general, the spectrum of the background noise is wider than that of the response. This is illustrated in Figure 3.2(A), in which the signal-to-noise ratio is represented by the ratio of the area delineated by the vertical lines to that delineated by the horizontal lines. Thus, there are frequency regions which contain only noise and no significant response-components. If the signal is passed through a band-pass filter whose characteristics are set such that the spectrum of the response is not modified, then those frequency regions containing only noise can be eliminated and the S/N ratio improved. Figure 3.2(B) shows a filter characteristic, and the resultant spectra which appear at the output of the filter are shown in Figure 3.2(C). The ratio of the areas of the response spectrum to the noise spectrum has now been significantly increased. Fig. 3.2 Improvement of signal-to-ratio by band-pass filtering. (A) shows the general case in which the spectrum of the noise covers a greater frequency range than does the spectrum of the response. The signal-to-noise ratio is represented by the area delineated by the vertical lines divided by that delineated by the horizontal lines. After being passed through a band-pass filter with the characteristics shown in (B), the resultant spectra are shown in (C). The signal-to-noise ratio is now clearly improved. As the filter bandwidth is narrowed, the S/N ratio for the response improves. However, at some frequency, the band limits begin to filter out the response spectrum, eliminate components of the response, and hence distort the waveform and reduce response amplitude. Figure 3.3 shows the effects of different recording bandwidths on the post-auricular muscle (PAM) response, and it can be seen that the response is markedly altered. Clearly, the band limits have to be chosen with considerable care. Fig. 3.3 Effects of filter bandwidth on the postauricular muscle response. The change in waveforms with various high-frequency limits is shown. The limits are (A) 4 kHz, (B) 500 Hz, (C) 200 Hz, and (D) 100 Hz (x axis = 5 ms/div.; y axis = 0.5 μV/div.). Physicists are often concerned with setting filter limits to preserve waveform fidelity. However, clinically, one does not have to be unduly concerned with this idea. In clinical practice, maximum waveform fidelity is an arbitrary concept involving considerations of what is the ‘true’ response and whether the eliminated frequency components are a clinically significant part of the response. If the response is to be used for threshold estimation, then maximum response detectability is required, and waveform distortion is not important. Thus, for this application, filter limits should be chosen to maximize response detectability rather than for any other reason. Only if there is diagnostic information to be obtained from the waveform of the response should the filter limits be set such that the waveform is not distorted.
Basic principles of instrumentation and signal-processing
BASIC RECORDING TECHNIQUES
Differential amplification
Band-pass filtering
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
