Basic Intravenous Therapy Calculations
Objectives
• Identify various electronic IV infusion devices.
• Calculate the amount of saline or heparin for use in keeping venous access patent.
• Calculate the grams of sodium chloride or dextrose in IV bags.
• Identify osmolarity values for IV solutions.
• Check physician’s IV order for type of solution, amount, additives, and rate.
• Set PCA pump using standard protocol.
• Analyze IV orders for safe administration using critical thinking skills.
Introduction
It is the nurse’s responsibility to calculate the milliliters per hour or drops per minute to regulate an intravenous infusion. Knowledge of electronic infusion devices is required as is knowledge of the basic hand-regulated primary sets. The nurse is responsible for calculating the intravenous piggyback (IVPB) infusions that are timed for shorter periods.
IV Infusions
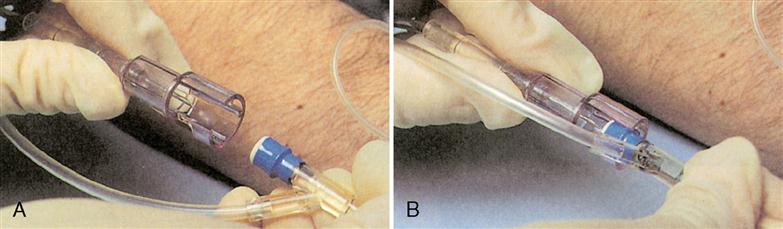
Intravenous (IV) infusions are used more frequently today than intramuscular (IM) injections. Continuous medication therapy can be delivered via an IV route, minimizing multiple injections via the IM route. Intermittent medication therapy can be delivered through a saline/heparin lock (Figure 7-1), which allows the patient free movement until the next scheduled dose. The saline lock is used for intermittent short-duration therapy in acute care, long-term care, and home care. Intermittent therapy can also be delivered as a piggyback with a continuous infusion. A heparin flush can also be used to keep the port patent.
Medications (additives) can be added to the IV by the manufacturer, pharmacist, or nurse. The physician orders the medication, strength, and amount, as well as the type and amount of diluent. It is important that the person responsible for the IV understand the actions of the medication, flow rate, adverse reactions, and antidotes. IV fluids flow directly into the vein, resulting in immediate action, and cannot be retrieved. Therefore, it is imperative that the correct calculations, medications, and flow rate be administered.
An intermittent IV lock is known by many different terms. Some terms used are saline lock, hep lock, PRN cap, intermittent IV (INT), and intermittent peripheral infusion device (IPD). All have needleless resealable valves (Figure 7-2).
Types of IV Lines
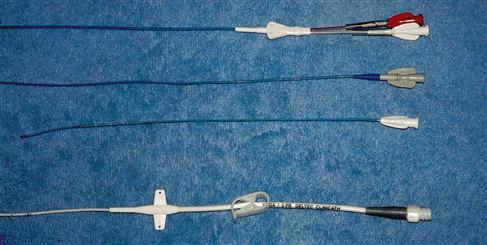
There are many types of IV tubing used for temporary and long-term access to veins and arteries.
Peripheral A peripheral line is usually used for fluid replacement and temporary intermittent medication administration. The IV line is inserted in the hand, arm, or possibly leg if the hand or arm cannot be accessed. Foot and scalp sites are used for infants.
Peripheral inserted central catheter (PICC) A PICC line (Figure 7-3) is longer than a central catheter line (approximately 22 inches in length). The insertion point is usually the vein in the antecubital region of the arm, where the line is then advanced into the superior vena cava. It is inserted by a PICC-certified RN or physician. Only solutions with a osmolarity of less than 10% should be administered via peripheral lines.
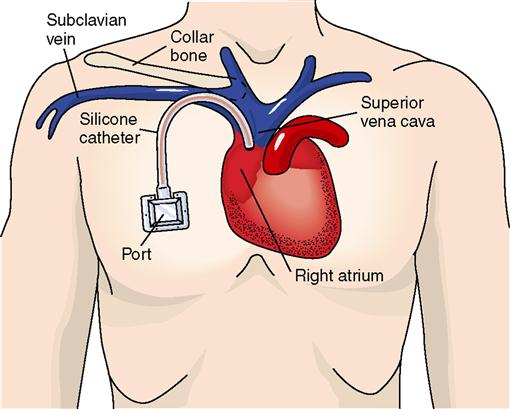
Central line A central line (Figure 7-4) is inserted by an MD or DO directly into the jugular or subclavian vein and then into the superior vena cava. This type of line is for therapy requiring a longer period of time.
 CLINICAL ALERT
CLINICAL ALERT
Only solutions with an osmolarity of less than 10% should be administered via peripheral lines.
Table 7-1 is a guide that can be used to maintain patency by flushing intermittent access locks. Always refer to hospital protocol for type of solution, volume, and frequency.
Table 7-1
| Catheter | Flush Solution | Volume (mL) |
| Peripheral | Normal saline | 1-3 mL |
| Peripherally inserted central catheter (PICC) | Normal saline | 3-5 mL |
| Central venous | Heparinized saline | 5-10 mL of saline followed with 3 mL heparin 1:100 units per mL |
 CLINICAL ALERT
CLINICAL ALERT
When flushing peripheral IV lines, a 10 mL syringe should be used. A smaller syringe creates greater pressure within the line, which may cause damage to the vein and be harmful to the patient.
IV Calculations
Check IV orders before beginning calculations. There are two steps in IV calculations. The first step is to find out how many milliliters per hour (volume) the IV is ordered to infuse. The second step is to calculate the drops per minute needed to infuse the ordered volume.
Analyze your problem. If the order says to infuse the IV for 24 hours, calculate the mL per hr by beginning with Step 1. If the order says to infuse the IV at 75 mL per hr, begin with Step 2.
Step 1
mL/hr
RULE
When the total volume is given, calculate the mL/hr.
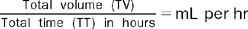
Example
Ordered: 2000 mL D5W (dextrose 5% in water) to be infused for 24 hours. The problem is to find out how many mL per hr the patient must receive for the 2000 mL to be infused in 24 hours.
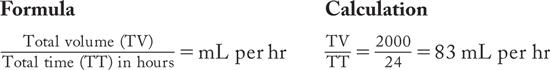
We now know that to infuse 2000 mL of fluid in 24 hours, the patient must receive 83 mL per hr. Infusion devices are calibrated for mL per hr.
Drop Factor Calculations
Step 2
Drops per min
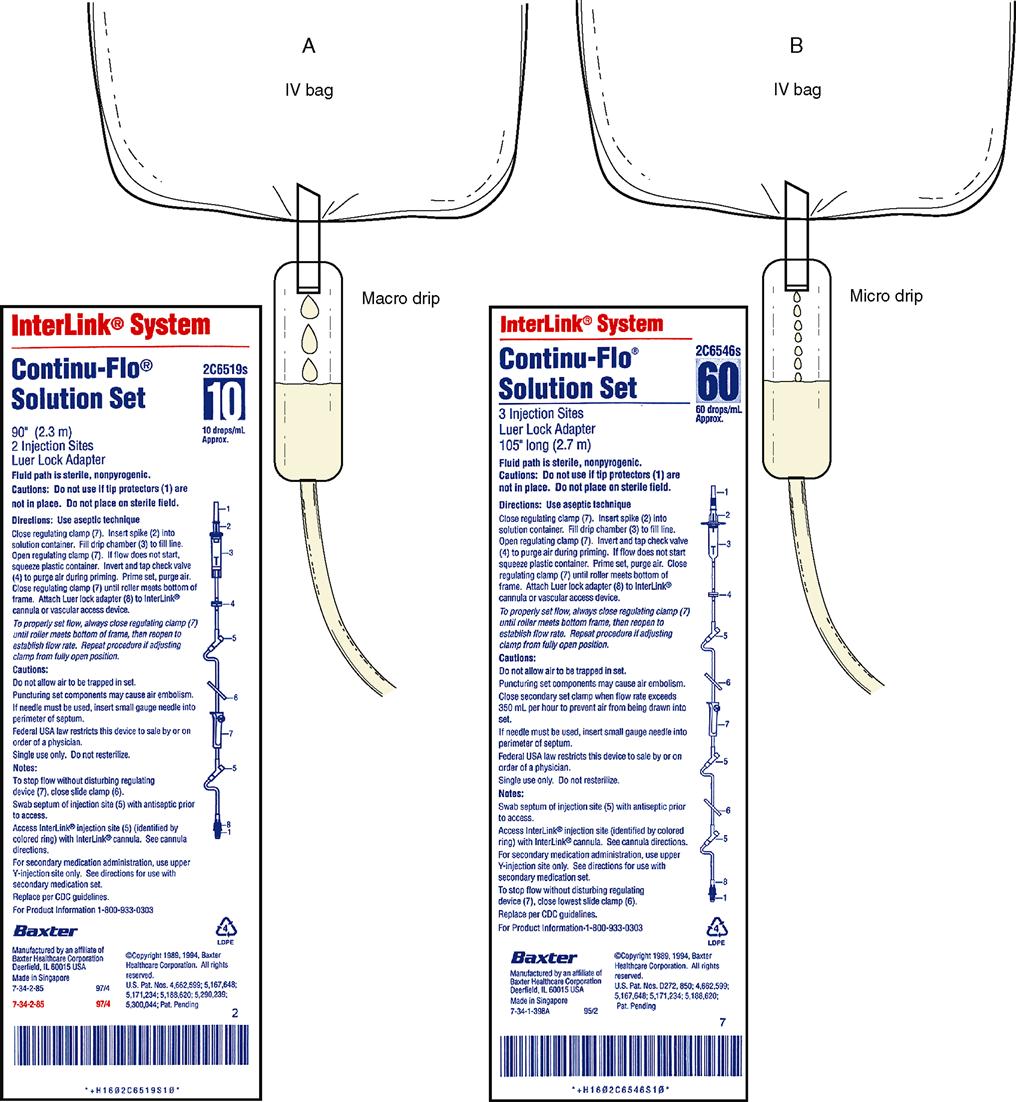
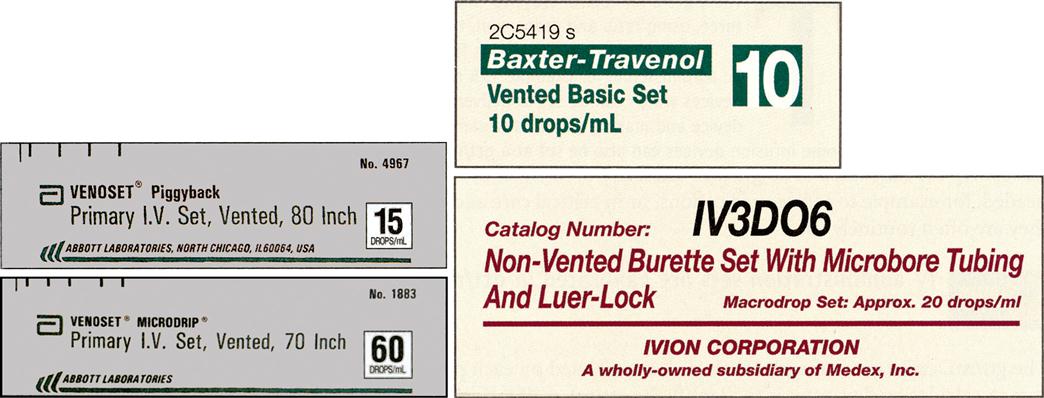
The drop factor is needed to calculate drops per min. The drop factor is the number of drops in 1 mL. The diameter of the needle where the drop enters the drip chamber varies from one manufacturer to another. The bigger the needle, the fatter the drop (Figure 7-5, A); it takes only 10 macrodrops to make a milliliter. The smallest unit is the microdrop (60 drops per mL) (Figure 7-5, B). This is used for people who can tolerate only small amounts of fluid, such as pediatric and geriatric patients and patients who require fluid restrictions. Drop factors of 10, 15, 20, and 60 (microdrip) are the most common. The drop factor is determined by the manufacturer and is found on the IV tubing package.
RULE
When the mL per hr is given, calculate the drops per min.
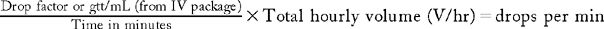
Example
Ordered: D5W to infuse at 83 mL per hr. The drop factor (Df) is 10.
Drops cannot be timed in tenths, only in whole numbers. If the decimal is greater than or equal to 0.5, round to the next higher number.
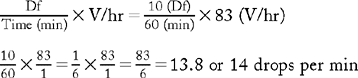
Example
Ordered: Antibiotic to infuse at 100 mL in 30 min. The drop factor is 15.
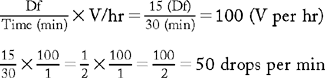
Summary
Two-step IV flow rate calculations
Step 1 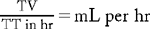
Step 2 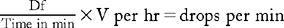
remember
Reduce the fraction Df per min before multiplying by the volume.
Example
Which would you rather calculate?
The reduced fraction is easier to calculate.
remember
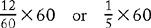
When the IV tubing is microdrip, 60 drops per mL, the drops per min will be the same as the mL per hr.
Example
1000 mL to infuse in 8 hours with a microdrip set.
Step 1 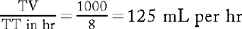
Step 2 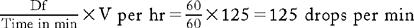
Drops per Minute by Manufacturer
A simple approach to calculate drops per min after you have determined the mL per hr is to memorize the reduced fraction numbers. Manufacturers have established rates for their products (Figure 7-6). Below is an example.
| Product Drip Rates | Minutes | Df | = | Reduced Number |
| 60 drops per mL | 60 | 60 | = | 1 |
| 20 drops per mL | 60 | 20 | = | 3 |
| 15 drops per mL | 60 | 15 | = | 4 |
| 10 drops per mL | 60 | 10 | = | 6 |
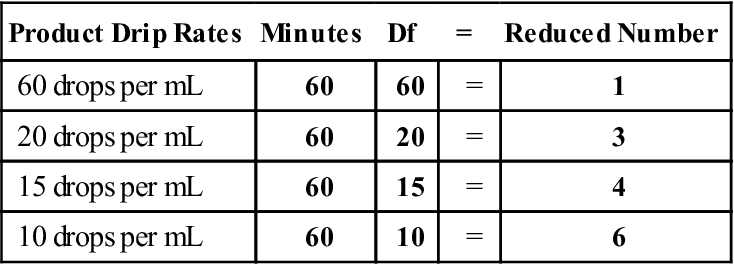
You may have to memorize only one number because most facilities purchase equipment from a single company.
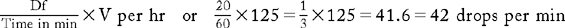
Example
If you know you are using a set that delivers 20 drops per mL, divide 3 into the mL per hr.
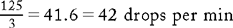
As you already know, the formula for calculating drops per min is:
Now you know two different methods for calculating drops per min.
 CLINICAL ALERT
CLINICAL ALERT
Check the IV every hour, even if an infusion device is used. Recheck drops per minute rate frequently because the IV rate can vary with position. Time taping the IV has become important as electrical blackouts and brown outs can adversely affect the device.
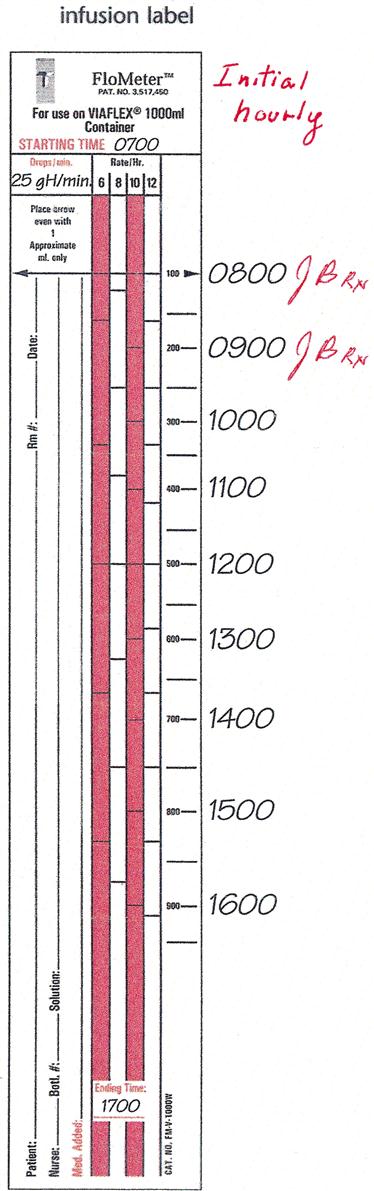
Flo Meter Tape
The order is to infuse 1000 mL in 10 hr (Figure 7-7). The infusion label shows a starting time of 0700 hr and an ending time of 1700 hr. The IV is scheduled to infuse for 10 hr. Use the 10 hr rate per hr on the tape and initital each hour at 100 mL per hour. The ending time will be 1700 hr.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree