B
Babinski’s reflex
[Extensor plantar reflex]
Babinski’s reflex—dorsiflexion of the great toe with extension and fanning of the other toes—is an abnormal reflex elicited by firmly stroking the lateral aspect of the sole of the foot with a blunt object. (See How to elicit Babinski’s reflex.) In some patients, this reflex can be triggered by noxious stimuli, such as pain, noise, or even bumping of the bed. An indicator of corticospinal damage, Babinski’s reflex may occur unilaterally or bilaterally and may be temporary or permanent. A temporary Babinski’s reflex commonly occurs during the postictal phase of a seizure, whereas a permanent Babinski’s reflex occurs with corticospinal damage. A positive Babinski’s reflex is normal in neonates and in infants up to age 24 months.
HISTORY AND PHYSICAL EXAMINATION
After eliciting a positive Babinski’s reflex, evaluate the patient for other neurologic signs. Evaluate muscle strength in each extremity by having the patient push or pull against your resistance. Passively flex and extend the extremity to assess muscle tone. Intermittent resistance to flexion and extension indicates spasticity, and a lack of resistance indicates flaccidity.
Next, check for evidence of incoordination by asking the patient to perform a repetitive activity. Test deep tendon reflexes (DTRs) in the patient’s elbow, antecubital area, wrist, knee, and ankle by striking the tendon with a reflex hammer. An exaggerated muscle response indicates hyperactive DTRs; little or no muscle response indicates hypoactivity.
Then evaluate pain sensation and proprioception in the feet. As you move the patient’s toes up and down, ask him to identify the direction in which the toes have been moved without looking at his feet.
MEDICAL CAUSES
♦ Amyotrophic lateral sclerosis (ALS). In this progressive motor neuron disorder, bilateral Babinski’s reflex may occur with hyperactive DTRs and spasticity. Typically, ALS produces fasciculations accompanied by muscle atrophy and weakness. Incoordination makes carrying out activities of daily living difficult for the patient. Associated signs and symptoms include impaired speech; difficulty chewing, swallowing, and breathing; urinary frequency and urgency; and, occasionally, choking and excessive drooling. Although his mental status remains intact, the patient’s poor prognosis may cause periodic depression. Progressive bulbar palsy involves the brain stem and may cause episodes of crying or inappropriate laughter.
♦ Brain tumor. A brain tumor that involves the corticospinal tract may produce Babinski’s reflex. The reflex may be accompanied by hyperactive DTRs (unilateral or bilateral), spasticity, seizures, cranial nerve dysfunction, hemiparesis or hemiplegia, decreased pain sensation, unsteady gait, incoordination, headache, emotional
lability, and decreased level of consciousness (LOC).
lability, and decreased level of consciousness (LOC).
♦ Familial spastic paraparesis. Familial spastic paraparesis may produce bilateral Babinski’s reflex accompanied by hyperactive DTRs and progressive spasticity with ataxia and weakness.
♦ Friedreich’s ataxia. Friedreich’s ataxia is a familial disorder that may produce bilateral Babinski’s reflex. Accompanying it are higharched feet, hypoactive DTRs, hypotonia, ataxia, head tremor, weakness, and paresthesia.
♦ Head trauma. Unilateral or bilateral Babinski’s reflex may occur as the result of primary corticospinal damage or secondary injury associated with increased intracranial pressure. Hyperactive DTRs and spasticity commonly occur with Babinski’s reflex. The patient may also have weakness and incoordination. Other signs and symptoms vary with the type of head trauma and include headache, vomiting, behavior changes, altered vital signs, and decreased LOC with abnormal pupillary size and response to light.
♦ Hepatic encephalopathy. Babinski’s reflex occurs late in hepatic encephalopathy when the patient slips into a coma. It’s accompanied by hyperactive DTRs and fetor hepaticus.
♦ Meningitis. In meningitis, bilateral Babinski’s reflex commonly follows fever, chills, and malaise and is accompanied by nausea and vomiting. As meningitis progresses, it also causes decreased LOC, nuchal rigidity, positive Brudzinski’s and Kernig’s signs, hyperactive DTRs, and opisthotonos. Associated signs and symptoms include irritability, photophobia, diplopia, delirium, and deep stupor that may progress to coma.
♦ Multiple sclerosis (MS). In most patients with MS—a demyelinating disorder—bilateral Babinski’s reflex eventually follows initial signs and symptoms of paresthesia, nystagmus, and blurred or double vision. Associated signs and symptoms include scanning speech (clipped speech with some pauses between syllables), dysphagia, intention tremor, weakness, incoordination, spasticity, gait ataxia, seizures, paraparesis or paraplegia, bladder incontinence, and emotional lability. Loss of pain and temperature sensation and proprioception occur occasionally.
♦ Pernicious anemia. Bilateral Babinski’s reflex occurs late in pernicious anemia when vitamin B12 deficiency affects the central nervous
system. Anemia may eventually cause widespread GI, neurologic, and cardiovascular effects. Characteristic GI signs and symptoms include nausea, vomiting, anorexia, weight loss, flatulence, diarrhea, and constipation. Gingival bleeding and a sore, inflamed tongue may make eating painful and intensify anorexia. The lips, gums, and tongue appear markedly pale. Jaundice may cause pale to bright yellow skin.
system. Anemia may eventually cause widespread GI, neurologic, and cardiovascular effects. Characteristic GI signs and symptoms include nausea, vomiting, anorexia, weight loss, flatulence, diarrhea, and constipation. Gingival bleeding and a sore, inflamed tongue may make eating painful and intensify anorexia. The lips, gums, and tongue appear markedly pale. Jaundice may cause pale to bright yellow skin.
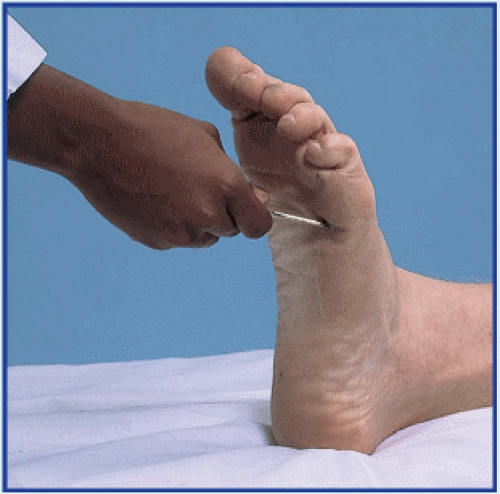
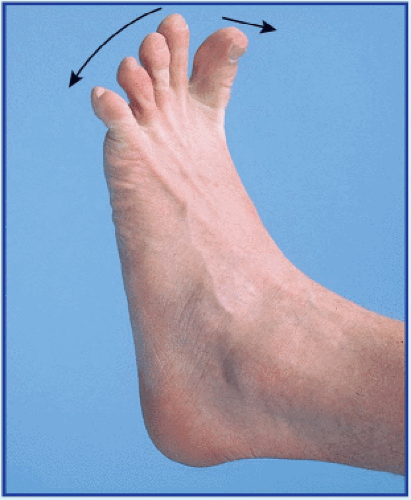
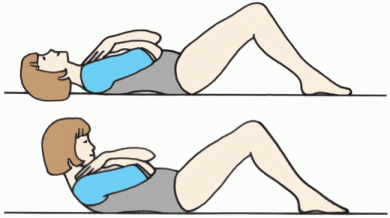
How to elicit Babinski’s reflex
To elicit Babinski’s reflex, stroke the lateral aspect of the sole of the patient’s foot with your thumbnail or another moderately sharp object. Normally, this elicits flexion of all toes (a negative Babinski’s reflex), as shown in the top illustration. In a positive Babinski’s reflex, the great toe dorsiflexes and the other toes fan out, as shown in the bottom illustration.
Characteristic neurologic signs and symptoms include neuritis, weakness, peripheral paresthesia, disturbed position sense, incoordination, ataxia, positive Romberg’s sign, lightheadedness, bowel and bladder incontinence, and altered vision (diplopia, blurred vision), taste, and hearing (tinnitus). Pernicious anemia may also produce irritability, poor memory, headache, depression, impotence, and delirium. Characteristic cardiovascular signs and symptoms include palpitations, wide pulse pressure, dyspnea, orthopnea, and tachycardia.
♦ Rabies. Bilateral Babinski’s reflex—possibly elicited by nonspecific noxious stimuli alone— appears in the excitation phase of rabies. This phase occurs 2 to 10 days after the onset of prodromal signs and symptoms, such as fever, malaise, and irritability (which occur 30 to 40 days after a bite from an infected animal). Rabies is characterized by marked restlessness and extremely painful pharyngeal muscle spasms. Difficulty swallowing causes excessive drooling and hydrophobia in about 50% of affected patients. Seizures and hyperactive DTRs may also occur.
♦ Spinal cord injury. In an acute injury, spinal shock temporarily erases all reflexes. As shock resolves, Babinski’s reflex occurs—unilaterally when the injury affects only one side of the spinal cord (Brown-Séquard syndrome) and bilaterally when the injury affects both sides. Rather than signaling the return of neurologic function, this reflex confirms corticospinal damage. It’s accompanied by hyperactive DTRs, spasticity, and variable or total loss of pain and temperature sensation, proprioception, and motor function. Horner’s syndrome, marked by unilateral ptosis, pupillary constriction, and facial anhidrosis, may occur in a lower cervical cord injury.
♦ Spinal cord tumor. In a spinal cord tumor, bilateral Babinski’s reflex occurs with variable loss of pain and temperature sensation, proprioception, and motor function. Spasticity, hyperactive DTRs, absent abdominal reflexes, and incontinence are also characteristic. Diffuse pain may occur at the level of the tumor.
♦ Spinal paralytic poliomyelitis. Unilateral or bilateral Babinski’s reflex occurs 5 to 7 days after the onset of fever. It’s accompanied by progressive weakness, paresthesia, muscle tenderness, spasticity, irritability and, later, atrophy. Resistance to neck flexion is characteristic, as are Hoyne’s, Kernig’s, and Brudzinski’s signs.
♦ Spinal tuberculosis. Spinal tuberculosis may produce bilateral Babinski’s reflex accompanied by variable loss of pain and temperature sensation, proprioception, and motor function. It also causes spasticity, hyperactive DTRs, bladder incontinence, and absent abdominal reflexes.
♦ Stroke. Babinski’s reflex varies with the site of the stroke. A stroke involving the cerebrum produces unilateral Babinski’s reflex accompanied by hemiplegia or hemiparesis, unilateral hyperactive DTRs, hemianopsia, and aphasia. A stroke involving the brain stem produces bilateral Babinski’s reflex accompanied by bilateral weakness or paralysis, bilateral hyperactive DTRs, cranial nerve dysfunction, incoordination, and unsteady gait. Generalized signs and symptoms of stroke include headache, vomiting, fever, disorientation, nuchal rigidity, seizures, and coma.
♦ Syringomyelia. In syringomyelia, bilateral Babinski’s reflex occurs with muscle atrophy and weakness that may progress to paralysis. It’s accompanied by spasticity, ataxia and, occasionally, deep pain. DTRs may be hypoactive or hyperactive. Cranial nerve dysfunction, such as dysphagia and dysarthria, commonly appears late in the disorder.
SPECIAL CONSIDERATIONS
Babinski’s reflex usually occurs with incoordination, weakness, and spasticity, all of which increase the patient’s risk of injury. To prevent injury, assist the patient with activities and keep his environment free from obstructions.
Diagnostic tests may include a computed tomography scan or magnetic resonance imaging of the brain or spine, angiography or myelography, and possibly a lumbar puncture to clarify or confirm the cause of Babinski’s reflex. Prepare the patient as necessary.
Back pain
Back pain affects an estimated 80% of the population; in fact, it’s the second leading reason—after the common cold—for lost time from work. Although this symptom may herald a spondylogenic disorder, it may also result from a genitourinary, GI, cardiovascular, orthopedic, or neoplastic disorder. Postural imbalance associated with pregnancy may also cause back pain.
The onset, location, and distribution of pain and its response to activity and rest provide important clues about the cause. Pain may be acute or chronic and constant or intermittent. It may remain localized in the back or radiate along the spine or down one or both legs. Pain may be exacerbated by activity—usually, bending, stooping, or lifting—and alleviated by rest, or it may be unaffected by either.
Intrinsic back pain results from muscle spasm, nerve root irritation, fracture, or a combination of these mechanisms. It usually occurs in the lower back, or lumbosacral area. Back pain may also be referred from the abdomen or flank, possibly signaling a life-threatening perforated ulcer, acute pancreatitis, or dissecting abdominal aortic aneurysm.
 If the patient reports acute, severe back pain, quickly take his vital signs; then perform a rapid evaluation to rule out life-threatening causes. Ask him when the pain began. Can he relate it to any causes? For example, did the pain occur after eating? After falling on the ice? Have the patient describe the pain. Is it burning, stabbing, throbbing, or aching? Is it constant or intermittent? Does it radiate to the buttocks or legs? Does he have leg weakness? Does the pain seem to originate in the abdomen and radiate to the back? Has he had a pain like this before? What makes it better or worse? Is it affected by activity or rest? Is it worse in the morning or evening? Does it wake him up? Typically, visceral-referred back pain is unaffected by activity and rest. In contrast, spondylogenic-referred back pain worsens with activity and improves with rest. Pain of neoplastic origin is usually relieved by walking and worsens at night.
If the patient reports acute, severe back pain, quickly take his vital signs; then perform a rapid evaluation to rule out life-threatening causes. Ask him when the pain began. Can he relate it to any causes? For example, did the pain occur after eating? After falling on the ice? Have the patient describe the pain. Is it burning, stabbing, throbbing, or aching? Is it constant or intermittent? Does it radiate to the buttocks or legs? Does he have leg weakness? Does the pain seem to originate in the abdomen and radiate to the back? Has he had a pain like this before? What makes it better or worse? Is it affected by activity or rest? Is it worse in the morning or evening? Does it wake him up? Typically, visceral-referred back pain is unaffected by activity and rest. In contrast, spondylogenic-referred back pain worsens with activity and improves with rest. Pain of neoplastic origin is usually relieved by walking and worsens at night.If the patient describes deep lumbar pain unaffected by activity, palpate for a pulsating epigastric mass. If this sign is present, suspect dissecting abdominal aortic aneurysm. Withhold food and fluid in anticipation of emergency surgery. Prepare for I.V. fluid replacement and oxygen administration.
If the patient describes severe epigastric pain that radiates through the abdomen to the back, assess him for absent bowel sounds and for abdominal rigidity and tenderness. If these occur, suspect a perforated ulcer or acute pancreatitis. Start an I.V. catheter for fluids and drugs, administer oxygen, and insert a nasogastric tube while withholding food.
HISTORY AND PHYSICAL EXAMINATION
If life-threatening causes of back pain are ruled out, continue with a complete history and physical examination. Be aware of the patient’s expressions of pain as you do so. Obtain a medical history, including past injuries and illnesses, and a family history. Ask about diet and alcohol intake. Also, take a drug history, including past and present prescription and over-the-counter drugs.
Next, perform a thorough physical examination. Observe skin color, especially in the patient’s legs, and palpate skin temperature. Palpate femoral, popliteal, posterior tibial, and pedal pulses. Ask about unusual sensations in the legs, such as numbness and tingling. Observe the patient’s posture if pain doesn’t prohibit standing. Does he stand erect or tend to lean toward one side? Observe the level of the shoulders and pelvis and the curvature of the back. Ask the patient to bend forward, backward, and from side to side while you palpate for paravertebral muscle spasms. Note rotation of the spine on the trunk. Palpate the dorsolumbar spine for point tenderness. Then ask the patient to walk—first on his heels, then on his toes; protect him from falling as he does so. Weakness may reflect a muscular disorder or spinal nerve root irritation. Place the patient in a sitting position to evaluate and compare patellar tendon (knee), Achilles tendon, and Babinski’s reflexes. Evaluate the strength of the extensor hallucis longus by asking the patient to hold up his big toe against resistance. Measure leg length and hamstring and quadriceps muscles
bilaterally. Note a difference of more than 3/8″ (1 cm) in muscle size, especially in the calf.
bilaterally. Note a difference of more than 3/8″ (1 cm) in muscle size, especially in the calf.
To reproduce leg and back pain, place the patient in a supine position on the examining table. Grasp his heel and slowly lift his leg. If he feels pain, note its exact location and the angle between the table and his leg when it occurs. Repeat this maneuver with the opposite leg. Pain along the sciatic nerve may indicate disk herniation or sciatica. Also, note the range of motion of the hip and knee.
Palpate the flanks and percuss with the fingertips or perform fist percussion to elicit costovertebral angle tenderness.
MEDICAL CAUSES
♦ Abdominal aortic aneurysm (dissecting). Life-threatening dissection of an abdominal aortic aneurysm may initially cause low back pain or dull abdominal pain, but it usually produces constant upper abdominal pain. A pulsating abdominal mass may be palpated in the epigastrium; after rupture, though, it no longer pulsates. Aneurysm dissection can also cause mottled skin below the waist, absent femoral and pedal pulses, blood pressure that’s lower in the legs than in the arms, mild to moderate tenderness with guarding, and abdominal rigidity. Signs of shock (such as cool, clammy skin) appear if blood loss is significant.
♦ Ankylosing spondylitis. Ankylosing spondylitis is a chronic, progressive disorder that causes sacroiliac pain, which radiates up the spine and is aggravated by lateral pressure on the pelvis. The pain is usually most severe in the morning or after a period of inactivity and isn’t relieved by rest. Abnormal rigidity of the lumbar spine with forward flexion is also characteristic. This disorder can cause local tenderness, fatigue, fever, anorexia, weight loss, and occasionally iritis.
♦ Appendicitis. Appendicitis is a life-threatening disorder in which a vague and dull discomfort in the epigastric or umbilical region migrates to McBurney’s point in the right lower quadrant. In retrocecal appendicitis, pain may also radiate to the back. The shift in pain is preceded by anorexia and nausea and is accompanied by fever, occasional vomiting, abdominal tenderness (especially over McBurney’s point), and rebound tenderness. Some patients also have painful urinary urgency.
♦ Cholecystitis. Cholecystitis produces severe pain in the right upper quadrant of the abdomen that may radiate to the right shoulder, chest, or back. The pain may arise suddenly or may increase gradually over several hours; many patients have a history of similar pain after a highfat meal. Accompanying signs and symptoms include anorexia, fever, nausea, vomiting, rightupper-quadrant tenderness, abdominal rigidity, pallor, and sweating.
♦ Chordoma. A slowly developing malignant tumor, chordoma causes persistent pain in the lower back, sacrum, and coccyx. As the tumor expands, pain may be accompanied by constipation and bowel or bladder incontinence.
♦ Endometriosis. Endometriosis causes deep sacral pain and severe cramping pain in the lower abdomen. The pain worsens just before or during menstruation and may be aggravated by defecation. It’s accompanied by constipation, abdominal tenderness, dysmenorrhea, and dyspareunia.
♦ Intervertebral disk rupture. Intervertebral disk rupture produces gradual or sudden low back pain with or without leg pain (sciatica). It rarely produces leg pain alone. Pain usually begins in the back and radiates to the buttocks and leg. The pain is exacerbated by activity, coughing, and sneezing and is eased by rest. It’s accompanied by paresthesia (most commonly, numbness or tingling in the lower leg and foot), paravertebral muscle spasm, and decreased reflexes on the affected side. This disorder also affects posture and gait. The patient’s spine is slightly flexed and he leans toward the painful side. He walks slowly and rises from a sitting to a standing position with extreme difficulty.
♦ Lumbosacral sprain. Lumbosacral sprain causes localized aching pain and tenderness associated with muscle spasm on lateral motion. The recumbent patient typically flexes his knees and hips to help ease pain. Flexion of the spine and movement intensify the pain, whereas rest helps relieve it.
♦ Metastatic tumors. Metastatic tumors commonly spread to the spine, causing low back pain in at least 25% of patients. Typically, the pain begins abruptly, is accompanied by cramping muscle pain (usually worse at night), and isn’t relieved by rest.
♦ Myeloma. Back pain caused by myeloma—a primary malignant tumor—usually begins abruptly and worsens with exercise. It may be accompanied by arthritic signs and symptoms, such as achiness, joint swelling, and tenderness. Other signs and symptoms include fever, malaise, peripheral paresthesia, and weight loss.
♦ Pancreatitis (acute). Pancreatitis is a lifethreatening disorder that usually produces fulminating, continuous upper abdominal pain that may radiate to both flanks and to the back. To relieve this pain, the patient may bend forward, draw his knees to his chest, or move about restlessly.
Early associated signs and symptoms include abdominal tenderness, nausea, vomiting, fever, pallor, and tachycardia; some patients experience abdominal guarding and rigidity, rebound tenderness, and hypoactive bowel sounds. Jaundice may be a late sign. Occurring as inflammation subsides, Turner’s sign (ecchymosis of the abdomen or flank) or Cullen’s sign (bluish discoloration of skin around the umbilicus and in both flanks) signals hemorrhagic pancreatitis.
♦ Perforated ulcer. In some patients, perforation of a duodenal or gastric ulcer causes sudden, prostrating epigastric pain that may radiate throughout the abdomen and to the back. This life-threatening disorder also causes boardlike abdominal rigidity, tenderness with guarding, generalized rebound tenderness, absence of bowel sounds, and grunting, shallow respirations. Associated signs include fever, tachycardia, and hypotension.
♦ Prostate cancer. Chronic aching back pain may be the only symptom of prostate cancer. This disorder may also cause hematuria and decreased urine stream.
♦ Pyelonephritis (acute). Pyelonephritis produces progressive flank and lower abdominal pain accompanied by back pain or tenderness (especially over the costovertebral angle). Other signs and symptoms include high fever and chills, nausea and vomiting, flank and abdominal tenderness, and urinary frequency and urgency.
♦ Reiter’s syndrome. In some patients, sacroiliac pain is the first sign of Reiter’s syndrome. Pain is accompanied by the classic triad of conjunctivitis, urethritis, and arthritis.
♦ Renal calculi. The colicky pain of renal calculi usually results from irritation of the ureteral lining, which increases the frequency and force of peristaltic contractions. The pain travels from the costovertebral angle to the flank, suprapubic region, and external genitalia. It varies in intensity but may become excruciating if calculi travel down a ureter. Calculi in the renal pelvis and calyces may cause dull and constant flank pain. Renal calculi also cause nausea, vomiting, urinary urgency (if a calculus lodges near the bladder), hematuria, and agitation due to pain. Pain resolves or significantly decreases after calculi move to the bladder. Encourage the patient to recover any expelled calculi for analysis.
♦ Sacroiliac strain. Sacroiliac strain causes sacroiliac pain that may radiate to the buttock, hip, and lateral aspect of the thigh. The pain is aggravated by weight bearing on the affected extremity and by abduction with resistance of the leg. Associated signs and symptoms include tenderness of the symphysis pubis and a limp or a gluteus medius or abductor lurch.
♦ Smallpox (variola major). Worldwide eradication of smallpox was achieved in 1977; the United States and Russia have the only known storage sites of the virus. The virus is considered a potential agent for biological warfare. Initial signs and symptoms include high fever, malaise, prostration, severe headache, backache, and abdominal pain. A maculopapular rash develops on the oral mucosa, pharynx, face, and forearms and then spreads to the trunk and legs. Within 2 days, the rash becomes vesicular and later pustular. The lesions develop at the same time, appear identical, and are more prominent on the face and extremities. The pustules are round, firm, and deeply embedded in the skin. After 8 to 9 days, the pustules form a crust, which later separates from the skin, leaving a pitted scar. Death may result from encephalitis, extensive bleeding, or secondary infection.
♦ Spinal neoplasm (benign). Spinal neoplasm typically causes severe localized back pain and scoliosis.
♦ Spinal stenosis. Resembling a ruptured intervertebral disk, spinal stenosis produces back pain with or without sciatica, which commonly affects both legs. The pain may radiate to the toes and may progress to numbness or weakness unless the patient rests.
♦ Spondylolisthesis. A major structural disorder characterized by forward slippage of one vertebra onto another, spondylolisthesis may produce no symptoms or may cause low back pain with or without nerve root involvement. Associated symptoms of nerve root involvement include paresthesia, buttock pain, and pain radiating down the leg. Palpation of the lumbar spine may reveal a “step-off” of the spinous process. Flexion of the spine may be limited.
♦ Transverse process fracture. This type of fracture causes severe localized back pain with muscle spasm and hematoma.
♦ Vertebral compression fracture. A vertebral compression fracture may be painless
initially. Several weeks later, it causes back pain aggravated by weight bearing and local tenderness. Fracture of a thoracic vertebra may cause referred pain in the lumbar area.
initially. Several weeks later, it causes back pain aggravated by weight bearing and local tenderness. Fracture of a thoracic vertebra may cause referred pain in the lumbar area.
Dear Patient:
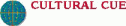
If you have chronic low back pain, the exercises illustrated here may help relieve your discomfort and prevent further lumbar deterioration. When you perform these exercises, keep in mind the following points:
♦ Breathe slowly, inhaling through your nose and exhaling completely through pursed lips.
♦ Begin gradually, performing each exercise only once per day and progressing to 10 repetitions.
♦ Exercise moderately; expect mild discomfort, but stop if you experience severe pain.
Back press
Lie on your back, with your arms on your chest or abdomen and your knees bent. Press the small (lower portion) of your back to the floor while tightening your abdominal muscles and buttocks. Count to 10; then slowly relax.
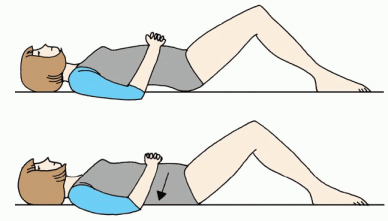 |
Knee grasp
Lie on your back, with your knees bent. Bring one knee to your chest, grasping it firmly with both hands; lower your knee. Repeat with the other knee—then with both knees, as shown here.
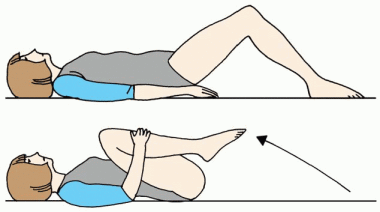 |
Knee bend
Stand with your hands on the back of a chair for support. Keeping your back straight, slowly bend your knees until you’re in a squatting position. Return to your starting position.
 |
Trunk curl
Lie on your back, with your knees bent and feet flat. Cross your arms on your chest. Lift your head and shoulders off of the floor, and hold for a count of 2. Repeat 10 times. Work up to at least 30, taking brief rests as needed.
 |
This patient-teaching aid may be reproduced by office copier for distribution to patients. © 2011, Lippincott Williams & Wilkins.
♦ Vertebral osteomyelitis. Initially, vertebral osteomyelitis causes insidious back pain. As it progresses, the pain may become constant, more pronounced at night, and aggravated by spinal movement. Accompanying signs and symptoms include vertebral and hamstring spasms, tenderness of the spinous processes, fever, and malaise.
♦ Vertebral osteoporosis. Vertebral osteoporosis causes chronic aching back pain that is aggravated by activity and somewhat relieved by rest. Tenderness may also occur.
OTHER CAUSES
♦ Neurologic tests. Lumbar puncture and myelography can produce transient back pain.
SPECIAL CONSIDERATIONS
Monitor the patient closely if the back pain suggests a life-threatening cause. Be alert for increasing pain, altered neurovascular status in the legs, loss of bowel or bladder control, altered vital signs, sweating, and cyanosis.
Until a tentative diagnosis is made, withhold analgesics, which may mask symptoms. Also withhold food and fluids in case surgery is necessary. Make the patient as comfortable as possible by elevating the head of the bed and placing a pillow under his knees. Encourage relaxation techniques such as deep breathing. Prepare the patient for a rectal or pelvic examination. He may also require routine blood tests, urinalysis, computed tomography scan, appropriate biopsies, and X-rays of the chest, abdomen, and spine.
Fit the patient for a corset or lumbosacral support, but instruct him not to wear it in bed. He may also require heat or cold therapy, a backboard, a convoluted foam mattress, or pelvic traction. Explain these pain-relief measures to the patient. Teach the patient about alternatives to analgesic drug therapy, such as biofeedback and transcutaneous electrical nerve stimulation.
Be aware that back pain is notoriously associated with malingering. Refer the patient to other professionals, such as a physical therapist, an occupational therapist, or a psychologist, if indicated.
PEDIATRIC POINTERS
Children may have difficulty describing back pain, so be alert for nonverbal clues, such as wincing or refusing to walk. Closely observe the family dynamics during history taking for clues of child abuse.
Back pain in children may stem from intervertebral disk inflammation (diskitis), neoplasms, idiopathic juvenile osteoporosis, and spondylolisthesis. Disk herniation typically doesn’t cause back pain. Scoliosis, a common disorder in adolescents, rarely causes back pain.
GERIATRIC POINTERS
Suspect metastatic cancer—especially of the prostate, colon, or breast—in older patients with a recent onset of back pain that usually isn’t relieved by rest and worsens at night.
PATIENT COUNSELING
If the patient has chronic back pain, reinforce instructions about bed rest, analgesics, antiinflammatories, and exercise. (See Exercises for chronic low back pain.) Also, suggest that he take daily warm baths to help relieve pain. Help the patient recognize the need to make necessary lifestyle changes, such as losing weight or correcting poor posture. Advise patients with acute back pain secondary to a musculoskeletal problem to continue their daily activities as tolerated, rather than staying on total bed rest.
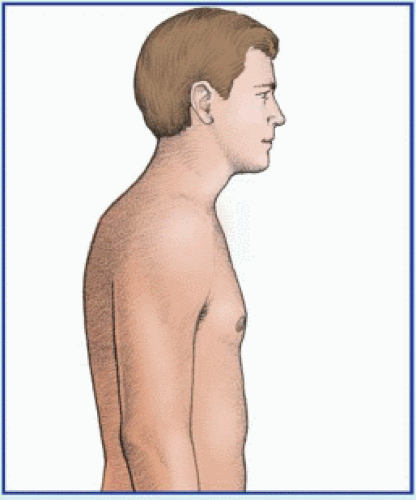
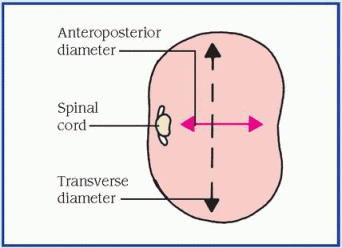
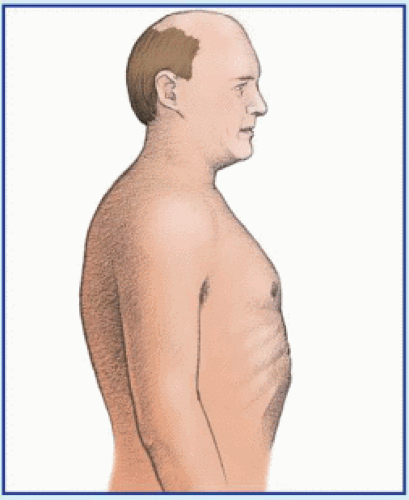
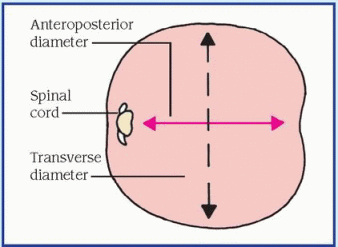
Barrel chest
In barrel chest, the normal elliptical configuration of the chest is replaced by a rounded one in which the anteroposterior diameter enlarges to approximate the transverse diameter. The diaphragm is depressed and the sternum pushed forward with the ribs attached in a horizontal, not angular, fashion. As a result, the chest appears continuously in the inspiratory position. (See Recognizing barrel chest, page 84.)
Typically a late sign of chronic obstructive pulmonary disease (COPD), barrel chest results from augmented lung volumes due to chronic airflow obstruction. The patient may not notice it because it develops gradually.
HISTORY AND PHYSICAL EXAMINATION
Begin by asking about a history of pulmonary disease. Note chronic exposure to environmental
irritants such as asbestos. Also ask about the patient’s smoking habits.
irritants such as asbestos. Also ask about the patient’s smoking habits.
Then explore other signs and symptoms of pulmonary disease. Does the patient have a cough? Is it productive or nonproductive? If it’s productive, have him describe the sputum’s color and consistency. Does the patient experience shortness of breath? Is it related to activity? Although dyspnea is common with COPD, many patients fail to associate it with the disease. Instead, they blame “old age” or “getting out of shape” for causing dyspnea.
Auscultate for abnormal breath sounds, such as crackles and wheezing. Then percuss the chest. Hyperresonant sounds indicate trapped air; dull or flat sounds indicate mucus buildup. Be alert for accessory muscle use, intercostal retractions, and tachypnea, which may signal respiratory distress.
Finally, observe the patient’s general appearance. Look for central cyanosis in the cheeks, nose, and mucosa inside the lips. In addition, look for peripheral cyanosis in the nail beds. Also note clubbing, a late sign of COPD.
MEDICAL CAUSES
♦ Asthma. Typically, barrel chest develops only in chronic asthma. An acute asthma attack causes severe dyspnea, wheezing, and a productive cough. It can also cause prolonged
expiratory time, accessory muscle use, tachycardia, tachypnea, perspiration, and flushing.
expiratory time, accessory muscle use, tachycardia, tachypnea, perspiration, and flushing.
♦ Chronic bronchitis. A late sign in chronic bronchitis, barrel chest is characteristically preceded by a productive cough and exertional dyspnea. This form of COPD may also cause cyanosis, tachypnea, wheezing, prolonged expiratory time, and accessory muscle use.
♦ Emphysema. Barrel chest is a late sign in this form of COPD. Typically, emphysema begins insidiously, with dyspnea the predominant symptom. Eventually, it may also cause chronic cough, anorexia, weight loss, malaise, accessory muscle use, pursed-lip breathing, tachypnea, peripheral cyanosis, and clubbing.
SPECIAL CONSIDERATIONS
To ease breathing, have the patient sit and lean forward, resting his hands on his knees to support the upper torso (tripod position). This position allows maximum diaphragmatic excursion, facilitating chest expansion.
PEDIATRIC POINTERS
In infants, the ratio of anteroposterior to transverse diameter is normally 1:1. As the child grows, this ratio gradually changes to 1:2 by age 5 to 6. Cystic fibrosis and chronic asthma may cause barrel chest in children.
GERIATRIC POINTERS
In elderly patients, senile kyphosis of the thoracic spine may be mistaken for barrel chest. However, patients with senile kyphosis lack signs of pulmonary disease.
PATIENT COUNSELING
Advise the patient to avoid bronchial irritants, especially smoking, which may exacerbate COPD. Tell him to report purulent sputum production, which may indicate upper respiratory tract infection. Instruct him to space his activities to help minimize exertional dyspnea.
Battle’s sign
Battle’s sign—ecchymosis over the mastoid process of the temporal bone—is commonly the only outward sign of a basilar skull fracture. In fact, this type of fracture may go undetected even by X-ray of the skull. If left untreated, a basilar skull fracture can be fatal because of associated injury to the nearby cranial nerves and brain stem as well as to blood vessels and the meninges.
Appearing behind one or both ears, Battle’s sign is easily overlooked or hidden by the patient’s hair. During emergency care of a trauma victim, it may be overshadowed by imminently life-threatening or more apparent injuries.
A force that’s strong enough to fracture the base of the skull causes Battle’s sign by damaging supporting tissues of the mastoid area and causing seepage of blood from the fracture site to the mastoid. Battle’s sign usually develops 24 to 36 hours after the fracture and may persist for several days to weeks.
HISTORY AND PHYSICAL EXAMINATION
Perform a complete neurologic examination, beginning with the history. Ask the patient about recent trauma to the head. Did he sustain a severe blow to the head? Was he involved in a motor vehicle accident? Note the patient’s level of consciousness as he responds. Does he respond quickly or slowly? Are his answers appropriate, or does he appear confused?
Check the patient’s vital signs; be alert for widening pulse pressure and bradycardia, signs of increased intracranial pressure. Assess cranial nerve function in nerves II, III, IV, VI, VII, and VIII. Evaluate pupillary size and response to light as well as motor and verbal responses. Relate these data to the Glasgow Coma Scale. Also, note cerebrospinal fluid (CSF) leakage from the nose or ears. Ask about postnasal drip, which may reflect CSF drainage down the throat. Look for the halo sign—a bloodstain encircled by a yellowish ring—on bed linens or dressings. To confirm that drainage is CSF, test it with a Dextrostix; CSF is positive for glucose, whereas mucus isn’t. Follow up the neurologic examination with a complete physical examination to detect other injuries associated with a basilar skull fracture.
MEDICAL CAUSES
♦ Basilar skull fracture. Battle’s sign may be the only outward sign of a basilar skull fracture, or it may be accompanied by periorbital ecchymosis (raccoon eyes), conjunctival hemorrhage, nystagmus, ocular deviation, epistaxis, anosmia, a bulging tympanic membrane (from CSF or blood accumulation), visible fracture lines on the external auditory canal, tinnitus, difficulty hearing, facial paralysis, or vertigo.
SPECIAL CONSIDERATIONS
Expect a patient with a basilar skull fracture to be on bed rest for several days to weeks. Keep him flat to decrease pressure on dural tears and to minimize CSF leakage. Monitor his neurologic status closely. Avoid nasogastric intubation and nasopharyngeal suction, which may cause cerebral infection. Also, caution the patient against blowing his nose, which may worsen a dural tear.
The patient may need skull X-rays and a computed tomography scan to help confirm a basilar skull fracture and to evaluate the severity of the head injury. Typically, these fractures and any associated dural tears heal spontaneously within several days to weeks. However, if the patient has a large dural tear, a craniotomy may be necessary to repair the tear with a graft patch.
PEDIATRIC POINTERS
Children who are victims of abuse commonly sustain basilar skull fractures from severe blows to the head. As in adults, Battle’s sign may be the only outward sign of fracture and, perhaps, the only clue to child abuse. If you suspect child abuse, follow hospital protocol for reporting the incident.
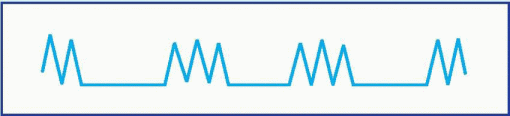
Biot’s respirations
[Ataxic respirations]
A late and ominous sign of neurologic deterioration, Biot’s respirations are characterized by irregular and unpredictable rate, rhythm, and depth. This rare breathing pattern may appear abruptly and may reflect increased pressure on the medulla coinciding with brain stem compression.
 Observe the patient’s breathing pattern for several minutes to avoid confusing Biot’s respirations with other respiratory patterns. (See Identifying Biot’s respirations.) Prepare to intubate the patient and provide mechanical ventilation. Next, take vital signs, noting especially increased systolic pressure.
Observe the patient’s breathing pattern for several minutes to avoid confusing Biot’s respirations with other respiratory patterns. (See Identifying Biot’s respirations.) Prepare to intubate the patient and provide mechanical ventilation. Next, take vital signs, noting especially increased systolic pressure.MEDICAL CAUSES
♦ Brain stem compression. Biot’s respirations are characteristic in brain stem compression—a neurologic emergency. Rapidly enlarging lesions may cause ataxic respirations and, eventually, complete respiratory arrest.
SPECIAL CONSIDERATIONS
Monitor vital signs frequently. Elevate the head of the patient’s bed 30 degrees to help reduce intracranial pressure. Prepare the patient for emergency surgery to relieve pressure on the brain stem. Computed tomography scans or magnetic resonance imaging may confirm the cause of brain stem compression.
Because Biot’s respirations typically reflect a grave prognosis, keep the patient’s family informed and provide emotional support.
PEDIATRIC POINTERS
Biot’s respirations are rarely seen in children.
Bladder distention
Bladder distention—abnormal enlargement of the bladder—results from an inability to excrete
urine, which then accumulates in the bladder. Distention can be caused by a mechanical or anatomic obstruction, a neuromuscular disorder, or the use of certain drugs. Relatively common in all ages and both sexes, it’s most common in older men with prostate disorders that cause urine retention.
urine, which then accumulates in the bladder. Distention can be caused by a mechanical or anatomic obstruction, a neuromuscular disorder, or the use of certain drugs. Relatively common in all ages and both sexes, it’s most common in older men with prostate disorders that cause urine retention.
Distention usually develops gradually, but it occasionally has a sudden onset. Gradual distention usually causes no symptoms until stretching of the bladder produces discomfort. Acute distention produces suprapubic fullness, pressure, and pain. If severe distention isn’t corrected promptly by catheterization or massage, the bladder rises within the abdomen, its walls become thin, and renal function can be impaired.
Bladder distention is aggravated by the intake of caffeine, alcohol, large quantities of fluid, and diuretics. (See Bladder distention: Causes and associated findings, pages 88 and 89.)
 If the patient has severe distention, insert an indwelling urinary catheter to help relieve discomfort and prevent bladder rupture. If more than 700 ml is emptied from the bladder, compressed blood vessels dilate, which may make the patient feel faint. Typically, the indwelling urinary catheter is clamped for 30 to 60 minutes to permit vessel compensation.
If the patient has severe distention, insert an indwelling urinary catheter to help relieve discomfort and prevent bladder rupture. If more than 700 ml is emptied from the bladder, compressed blood vessels dilate, which may make the patient feel faint. Typically, the indwelling urinary catheter is clamped for 30 to 60 minutes to permit vessel compensation.HISTORY AND PHYSICAL EXAMINATION
If distention isn’t severe, begin by reviewing the patient’s voiding patterns. Find out the time and amount of the patient’s last voiding and the amount of fluid consumed since then. Ask if he has difficulty urinating. Does he use Valsalva’s or Credé’s maneuver to initiate urination? Does he urinate with urgency or without warning? Is urination painful or irritating? Ask about the force and continuity of his urine stream and whether he feels that his bladder is empty after voiding.
Explore the patient’s history of urinary tract obstruction or infections; venereal disease; neurologic, intestinal, or pelvic surgery; lower abdominal or urinary tract trauma; and systemic or neurologic disorders. Ask about his drug history, including his use of over-the-counter drugs.
Take the patient’s vital signs, and percuss and palpate the bladder. (Remember that if the bladder is empty, it can’t be palpated through the abdominal wall.) Inspect the urethral meatus, and measure its diameter. Describe the appearance and amount of any discharge. Finally, test for perineal sensation and anal sphincter tone; in male patients, digitally examine the prostate gland.
MEDICAL CAUSES
♦ Benign prostatic hyperplasia (BPH). In BPH, bladder distention develops gradually as the prostate enlarges. Occasionally, its onset is acute. Initially, the patient experiences urinary hesitancy, straining, and frequency; reduced force of and inability to stop the urine stream; nocturia; and postvoiding dribbling. As the disorder progresses, it produces prostate enlargement, sensations of suprapubic fullness and incomplete bladder emptying, perineal pain, constipation, and hematuria.
♦ Bladder calculi. Bladder calculi may produce bladder distention, but pain is usually the only symptom. The pain is usually referred to the tip of the penis, the vulvar area, the lower back, or the heel. It worsens during walking or exercise and abates when the patient lies down. It’s usually most severe when micturition ceases. The pain may be accompanied by urinary frequency and urgency, terminal hematuria, and dysuria.
♦ Bladder cancer. By blocking the urethral orifice, neoplasms can cause bladder distention. Associated signs and symptoms include hematuria (most common sign); urinary frequency and urgency; nocturia; dysuria; pyuria; pain in the bladder, rectum, pelvis, flank, back, or legs; vomiting; diarrhea; and sleeplessness. A mass may be palpable on bimanual examination.
 Bladder cancer is twice as common in Whites as in Blacks. It’s relatively uncommon among Asians, Hispanics, and Native Americans.
Bladder cancer is twice as common in Whites as in Blacks. It’s relatively uncommon among Asians, Hispanics, and Native Americans.♦ Multiple sclerosis. In this neuromuscular disorder, urine retention and bladder distention result from interruption of upper motor neuron control of the bladder. Associated signs and symptoms include optic neuritis, paresthesia, impaired position and vibratory senses, diplopia, nystagmus, dizziness, abnormal reflexes, dysarthria, muscle weakness, emotional lability, Lhermitte’s sign (transient, electric-like shocks that spread down the body when the head is flexed), Babinski’s sign, and ataxia.
♦ Prostate cancer. Prostate cancer eventually causes bladder distention in about 25% of
patients. Usual signs and symptoms include dysuria, urinary frequency and urgency, nocturia, weight loss, fatigue, perineal pain, constipation, and induration of the prostate or a rigid, irregular prostate on digital rectal examination. In some patients, urine retention and bladder distention are the only signs.
patients. Usual signs and symptoms include dysuria, urinary frequency and urgency, nocturia, weight loss, fatigue, perineal pain, constipation, and induration of the prostate or a rigid, irregular prostate on digital rectal examination. In some patients, urine retention and bladder distention are the only signs.
Major associated signs and symptoms | ||||||||||||||||||||||||||
Common causes | Ataxia | Constipation | Dysuria | Fatigue | Fever | Hematuria | Muscle weakness | Myalgia | Nausea | Nocturia | Pain, buttock and sacral | Pain, flank | Pain, lower back | Pain, pelvic | Pain, penile | Pain, perineal | Pain, vulvar | Prostatic enlargement | Prostatic rigidity | Pyuria | Suprapubic fullness | Urethral discharge | Urinary frequency | Urinary stream changes | Urinary urgency | Vomiting |
Benign prostatic hyperplasia | • | • | • | • | • | • | • | • | ||||||||||||||||||
Bladder calculi | • | • | • | • | • | • | ||||||||||||||||||||
Bladder cancer | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||||
Multiple sclerosis | • | • | ||||||||||||||||||||||||
Prostate cancer | • | • | • | • | • | • | • | • | ||||||||||||||||||
Prostatitis (acute) | • | • | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||
Prostatitis (chronic) | • | • | • | • | • | • | • | • | • | • | • | |||||||||||||||
Spinal neoplasms | • | • | • | • | • | • | • | • | • | • | ||||||||||||||||
Urethral calculi | • | • | • | • | • | |||||||||||||||||||||
Urethral strictures | • | • | • | • | • | • | ||||||||||||||||||||
♦ Prostatitis. In acute prostatitis, bladder distention occurs rapidly along with perineal discomfort and a sensation of suprapubic fullness. Other signs and symptoms include perineal pain; tense, boggy, tender, and warm enlarged prostate; decreased libido; impotence; decreased force of the urine stream; dysuria; hematuria; and urinary frequency and urgency. Additional signs and symptoms include fatigue, malaise, myalgia, fever, chills, nausea, and vomiting.
Bladder distention is rare in chronic prostatitis, which may be accompanied by perineal discomfort, a sensation of suprapubic fullness, prostatic tenderness, decreased libido, urinary frequency and urgency, dysuria, pyuria, hematuria, persistent urethral discharge, ejaculatory pain, and dull pain radiating to the lower back, buttocks, penis, or perineum.
♦ Spinal neoplasms. Disrupting upper neuron control of the bladder, spinal neoplasms cause neurogenic bladder and resultant distention. Associated signs and symptoms include a sense of pelvic fullness, continuous overflow dribbling, back pain that often mimics sciatica pain, constipation, tender vertebral processes, sensory deficits, and muscle weakness, flaccidity, and atrophy. Signs and symptoms of urinary tract infection (dysuria, urinary frequency and
urgency, nocturia, tenesmus, hematuria, and weakness) may also occur.
urgency, nocturia, tenesmus, hematuria, and weakness) may also occur.
♦ Urethral calculi. In urethral calculi, urethral obstruction leads to interrupted urine flow and bladder distention. The obstruction causes pain radiating to the penis or vulva and referred to the perineum or rectum. It may also produce a palpable stone and urethral discharge.
♦ Urethral stricture. Urethral stricture results in urine retention and bladder distention with chronic urethral discharge (most common sign), urinary frequency (also common), dysuria, urgency, decreased force and diameter of the urine stream, and pyuria. Urinoma and urosepsis may also develop.
OTHER CAUSES
♦ Catheterization. Using an indwelling urinary catheter can result in urine retention and bladder distention. While the catheter is in place, inadequate drainage due to kinked tubing or an occluded lumen may lead to urine retention. In addition, a misplaced urinary catheter or irritation due to catheter removal may cause edema, thereby blocking urine outflow.
♦ Drugs. Parasympatholytics, anticholinergics, ganglionic blockers, sedatives, anesthetics, and opiates can produce urine retention and bladder distention.
SPECIAL CONSIDERATIONS
Monitor the patient’s vital signs and the extent of bladder distention. Encourage the patient to change positions to alleviate discomfort. Provide an analgesic if necessary.
PEDIATRIC POINTERS
Look for urine retention and bladder distention in any infant who fails to void normal amounts. (In the first 48 hours of life, an infant excretes about 60 ml of urine; during the next week, he excretes about 300 ml of urine daily.) In males, posterior urethral valves, meatal stenosis, phimosis, spinal cord anomalies, bladder diverticula, and other congenital defects may cause urinary obstruction and resultant bladder distention.
PATIENT COUNSELING
If the patient doesn’t require immediate urinary catheterization, provide privacy and suggest that he assume the normal voiding position. Teach him to perform Valsalva’s maneuver, or gently perform Credé’s maneuver. You can also stroke or intermittently apply ice to the inner thigh, or help him relax in a warm tub or sitz bath. Use the power of suggestion to stimulate voiding. For example, run water in the sink, pour warm water over his perineum, place his hands in warm water, or play tapes of aquatic sounds.
Blood pressure decrease
[Hypotension]
Low blood pressure refers to inadequate intravascular pressure to maintain the body’s oxygen requirements. Although commonly linked to shock, this sign may also result from cardiovascular, respiratory, neurologic, or metabolic disorders. Hypoperfusion states especially affect the kidneys, brain, and heart, and may lead to renal failure, change in level of consciousness (LOC), or myocardial ischemia. Low blood pressure may also be caused by certain diagnostic tests—most commonly those using contrast media—and the use of certain drugs. It may stem from stress or a change of position—specifically, rising abruptly from a supine or sitting position to a standing position (orthostatic hypotension).
Normal blood pressure varies considerably; what qualifies as low blood pressure for one person may be perfectly normal for another. Consequently, every blood pressure reading must be compared against the patient’s baseline. Typically, a reading below 90/60 mm Hg, or a drop of 30 mm Hg from the baseline, is considered low blood pressure.
Low blood pressure can reflect an expanded intravascular space (as in severe infections, allergic reactions, or adrenal insufficiency), reduced intravascular volume (as in dehydration and hemorrhage), or decreased cardiac output (as in impaired cardiac muscle contractility). Because the body’s pressure-regulating mechanisms are complex and interrelated, a combination of these factors usually contributes to low blood pressure.
 If the patient’s systolic pressure is less than 80 mm Hg, or 30 mm Hg below his baseline, suspect shock immediately. Quickly evaluate the patient for a decreased LOC. Check his apical pulse for tachycardia and respirations for tachypnea. Also, inspect the patient for cool, clammy skin. Elevate his legs above the level of his heart, or place him in Trendelenburg’s position if the bed can be adjusted. Then start an I.V. line using a large-bore catheter to replace fluids and blood or to administer drugs. Prepare to administer oxygen with mechanical ventilation if necessary. Monitor the patient’s intake and output, and insert an indwelling urinary catheter for the accurate measurement of urine. The patient may also need a central venous access device or a pulmonary artery catheter to facilitate monitoring of fluid status. Prepare for cardiac monitoring to evaluate cardiac rhythm. Be ready to insert a nasogastric tube to prevent aspiration in the comatose patient. Throughout emergency interventions, keep the patient’s spinal column immobile until spinal cord trauma is ruled out.
If the patient’s systolic pressure is less than 80 mm Hg, or 30 mm Hg below his baseline, suspect shock immediately. Quickly evaluate the patient for a decreased LOC. Check his apical pulse for tachycardia and respirations for tachypnea. Also, inspect the patient for cool, clammy skin. Elevate his legs above the level of his heart, or place him in Trendelenburg’s position if the bed can be adjusted. Then start an I.V. line using a large-bore catheter to replace fluids and blood or to administer drugs. Prepare to administer oxygen with mechanical ventilation if necessary. Monitor the patient’s intake and output, and insert an indwelling urinary catheter for the accurate measurement of urine. The patient may also need a central venous access device or a pulmonary artery catheter to facilitate monitoring of fluid status. Prepare for cardiac monitoring to evaluate cardiac rhythm. Be ready to insert a nasogastric tube to prevent aspiration in the comatose patient. Throughout emergency interventions, keep the patient’s spinal column immobile until spinal cord trauma is ruled out.HISTORY AND PHYSICAL EXAMINATION
If the patient is conscious, ask him about associated symptoms. For example, does he feel unusually weak or fatigued? Has he had nausea, vomiting, or dark or bloody stools? Is his vision blurred? Gait unsteady? Does he have palpitations, chest or abdominal pain, or difficulty breathing? Has he had episodes of dizziness or fainting? Do these episodes occur when he stands up suddenly? If so, take the patient’s blood pressure while he’s lying down, sitting, and then standing and compare readings. A drop in systolic or diastolic pressure of 10 mm Hg or more and an increase in heart rate of more than 15 beats/minute between position
changes suggest orthostatic hypotension. (See Ensuring accurate blood pressure measurement, page 92.)
changes suggest orthostatic hypotension. (See Ensuring accurate blood pressure measurement, page 92.)
Next, continue with a physical examination. Inspect the skin for pallor, sweating, and clamminess. Palpate peripheral pulses. Note a paradoxical pulse—an accentuated fall in systolic pressure during inspiration—which suggests pericardial tamponade. Then auscultate for abnormal heart sounds (gallops, murmurs), rate (bradycardia, tachycardia), or rhythm. Auscultate the lungs for abnormal breath sounds (diminished sounds, crackles, wheezing), rate (bradypnea, tachypnea), or rhythm (agonal or Cheyne-Stokes respirations). Look for signs of hemorrhage, including visible bleeding, palpable masses, bruising, and tenderness. Assess the patient for abdominal rigidity and rebound tenderness; auscultate for abnormal bowel sounds. Also, carefully assess the patient for possible sources of infection such as open wounds.
MEDICAL CAUSES
♦ Adrenal insufficiency (acute). Orthostatic hypotension is characteristic in acute adrenal insufficiency and is accompanied by fatigue, weakness, nausea, vomiting, abdominal discomfort, weight loss, fever, and tachycardia. The patient may also have hyperpigmentation of fingers, nails, nipples, scars, and body folds; pale, cool, clammy skin; restlessness; decreased urine output; tachypnea; and coma.
♦ Alcohol toxicity. Low blood pressure occurs infrequently in alcohol toxicity; more common signs and symptoms include a distinct alcohol breath odor, tachycardia, bradypnea, hypothermia, decreased LOC, seizures, staggering gait, nausea, vomiting, diuresis, and slow, stertorous breathing.
♦ Anaphylactic shock. Following exposure to an allergen, such as penicillin or insect venom, a dramatic fall in blood pressure and narrowed pulse pressure signal this severe allergic reaction. Initially, anaphylactic shock causes anxiety, restlessness, a feeling of doom, intense itching (especially of the hands and feet), and a pounding headache. Later, it may also produce weakness, sweating, nasal congestion, coughing, difficulty breathing, nausea, abdominal cramps, involuntary defecation, seizures, flushing, urinary incontinence, tachycardia, and change or loss of voice due to laryngeal edema.
♦ Anthrax, inhalation. Anthrax is an acute infectious disease that’s caused by the grampositive, spore-forming bacterium Bacillus anthracis. Although the disease most commonly occurs in wild and domestic grazing animals, such as cattle, sheep, and goats, the spores can live in the soil for many years. The disease can occur in humans exposed to infected animals, tissue from infected animals, or biological agents. Most natural cases occur in agricultural regions worldwide. Anthrax may occur in cutaneous, inhalation, or GI forms.
Inhalation anthrax is caused by inhalation of aerosolized spores. Initial signs and symptoms are flulike and include fever, chills, weakness, cough, and chest pain. The disease generally occurs in two stages with a period of recovery after the initial signs and symptoms. The second stage develops abruptly with rapid deterioration marked by fever, dyspnea, stridor, and hypotension generally leading to death within 24 hours. Radiologic findings include mediastinitis and symmetrical mediastinal widening.
♦ Cardiac arrhythmias. In an arrhythmia, blood pressure may fluctuate between normal and low readings. Dizziness, chest pain, difficulty breathing, light-headedness, weakness, fatigue, and palpitations may also occur. Auscultation typically reveals an irregular rhythm and a pulse rate greater than 100 beats/minute or less than 60 beats/minute.
♦ Cardiac contusion. In a cardiac contusion, low blood pressure occurs along with tachycardia and, at times, anginal pain and dyspnea.
♦ Cardiac tamponade. An accentuated fall in systolic pressure (more than 10 mm Hg) during inspiration, known as paradoxical pulse, is characteristic in patients with cardiac tamponade. This disorder also causes restlessness, cyanosis, tachycardia, jugular vein distention, muffled heart sounds, dyspnea, and Kussmaul’s sign (increased venous distention with inspiration).
♦ Cardiogenic shock. A fall in systolic pressure to less than 80 mm Hg, or to 30 mm Hg less than the patient’s baseline, because of decreased cardiac contractility is characteristic in patients with this disorder. Accompanying low blood pressure are tachycardia, narrowed pulse pressure, diminished Korotkoff sounds, peripheral cyanosis, and pale, cool, clammy skin. Cardiogenic shock also causes restlessness and anxiety, which may progress to disorientation and confusion. Associated signs and symptoms include angina, dyspnea, jugular vein distention,
oliguria, ventricular gallop, tachypnea, and weak, rapid pulse.
oliguria, ventricular gallop, tachypnea, and weak, rapid pulse.
When taking the patient’s blood pressure, begin by applying the cuff properly, as shown here.
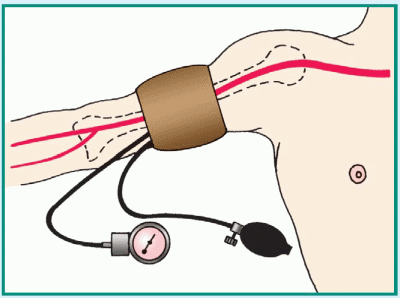 |
Then be alert for these common pitfalls to avoid recording an inaccurate blood pressure measurement.
♦ Wrong-sized cuff. Select the appropriatesized cuff for the patient. This ensures that adequate pressure is applied to compress the brachial artery during cuff inflation. A cuff bladder that’s too narrow will yield a falsehigh reading; one that’s too wide, a false-low reading. The cuff bladder width should be about 40% of the circumference of the midpoint of the limb; bladder length should be twice the width. If the arm circumference is less than 13″ (33 cm), select a regular-sized cuff; if it’s between 13″ and 16″ (33 to 40.5 cm), a large-sized cuff; if it’s more than 16″, a thigh cuff. Pediatric cuffs are also available.
♦ Slow cuff deflation, causing venous congestion in the extremity. Don’t deflate the cuff more slowly than 2 mm Hg/heartbeat because you’ll get a false-high reading.
♦ Cuff wrapped too loosely, reducing its effective width. Tighten the cuff to avoid a false-high reading.
♦ Mercury column not read at eye level. Read the mercury column at eye level. If the column is below eye level, you may record a false-low reading; if it’s above eye level, a false-high reading.
♦ Tilted mercury column. Keep the mercury column vertical to avoid a false-high reading.
♦ Poorly timed measurement. Don’t take the patient’s blood pressure if he appears anxious or has just eaten or ambulated; you’ll get a false-high reading.
♦ Incorrect position of the arm. Keep the patient’s arm level with his heart to avoid a falselow reading.
♦ Cuff overinflation, causing venospasm or pain. Don’t overinflate the cuff because you’ll get a false-high reading.
♦ Failure to notice an auscultatory gap (sound fades out for 10 to 15 mm Hg, then returns). To avoid missing the top Korotkoff sound, estimate systolic pressure by palpation first. Then inflate the cuff rapidly—at a rate of 2 to 3 mm Hg/second—to about 30 mm Hg above the palpable systolic pressure.
♦ Inaudibility of feeble sounds. Before reinflating the cuff, have the patient raise his arm to reduce venous pressure and amplify lowvolume sounds. After inflating the cuff, lower the patient’s arm; then deflate the cuff and listen. Alternatively, with the patient’s arm positioned at heart level, inflate the cuff and have the patient make a fist. Have him rapidly open and close his hand 10 times before you begin to deflate the cuff; then listen. Be sure to document that the blood pressure reading was augmented.
♦ Cholera. Cholera is an acute infection caused by the bacterium Vibrio cholerae that may be mild with uncomplicated diarrhea or severe and life-threatening. Cholera is spread by ingestion of contaminated water or food, especially shellfish. Signs include abrupt watery diarrhea and vomiting. Severe water and electrolyte loss leads to thirst, weakness, muscle cramps, decreased skin turgor, oliguria, tachycardia, and hypotension. Without treatment, death can occur within hours.
♦ Diabetic ketoacidosis. Hypovolemia triggered by osmotic diuresis in hyperglycemia is responsible for the low blood pressure associated with diabetic ketoacidosis, which is usually present in patients with type 1 diabetes mellitus. It also commonly produces polydipsia, polyuria, polyphagia, dehydration, weight loss, abdominal pain, nausea, vomiting, breath with fruity odor, Kussmaul’s respirations, tachycardia, seizures,
confusion, and stupor that may progress to coma.
confusion, and stupor that may progress to coma.
♦ Heart failure. In heart failure, blood pressure may fluctuate between normal and low readings, but a precipitous drop in blood pressure may signal cardiogenic shock. Other signs and symptoms of heart failure include exertional dyspnea, dyspnea of abrupt or gradual onset, paroxysmal nocturnal dyspnea or difficulty breathing in the supine position (orthopnea), fatigue, weight gain, pallor or cyanosis, sweating, and anxiety. Auscultation reveals ventricular gallop, tachycardia, bilateral crackles, and tachypnea. Dependent edema, jugular vein distention, increased capillary refill time, and hepatomegaly may also occur.
♦ Hyperosmolar hyperglycemic nonketotic syndrome (HHNS). HHNS, which is common in persons with type 2 diabetes mellitus, decreases blood pressure—at times dramatically, if the patient loses significant fluid from diuresis due to severe hyperglycemia and hyperosmolarity. It also produces dry mouth, poor skin turgor, tachycardia, confusion progressing to coma and, occasionally, generalized tonic-clonic seizures.
♦ Hypovolemic shock. A fall in systolic pressure to less than 80 mm Hg, or 30 mm Hg less than the patient’s baseline, secondary to acute blood loss or dehydration is characteristic in patients with hypovolemic shock. Accompanying it are diminished Korotkoff sounds, narrowed pulse pressure, and rapid, weak, and irregular pulse. Peripheral vasoconstriction causes cyanosis of the extremities and pale, cool, clammy skin. Other signs and symptoms include oliguria, confusion, disorientation, restlessness, and anxiety.
♦ Hypoxemia. Initially, blood pressure may be normal or slightly elevated, but as hypoxemia becomes more pronounced blood pressure drops. The patient may also display tachycardia, tachypnea, dyspnea, confusion, and stupor that may progress to coma.
♦ Myocardial infarction. In this life-threatening disorder, blood pressure may be low or high. However, a precipitous drop in blood pressure may signal cardiogenic shock. Associated signs and symptoms include chest pain that may radiate to the jaw, shoulder, arm, or epigastrium; dyspnea; anxiety; nausea or vomiting; sweating; and cool, pale, or cyanotic skin. Auscultation may reveal an atrial gallop, a murmur and, occasionally, an irregular pulse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree