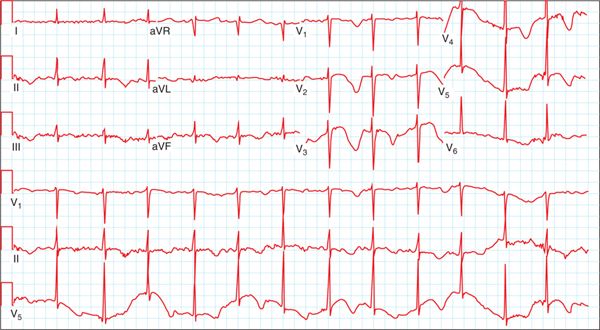
FIGURE 63-1 Initial rhythm seen on rhythm strip following witnessed arrest.
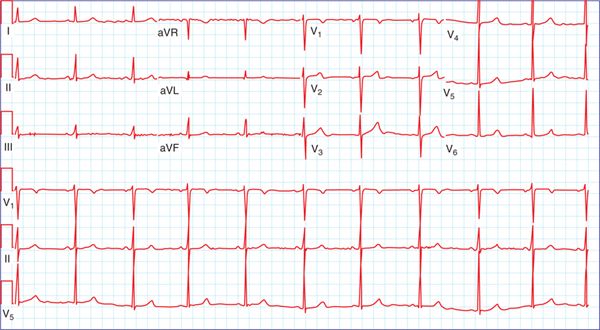
FIGURE 63-2 Initial 12-lead ECG following defibrillation.
FIGURE 63-3 Twelve-lead ECG several days following cessation of levofloxacin.
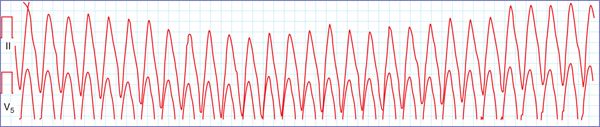
A 60-year-old man with a known medical history of coronary artery disease, previous stent to the left anterior descending coronary artery with a chronically occluded right coronary artery, hypertension, hyperlipidemia, diabetes, and an ischemic cardiomyopathy with an ejection fraction (EF) of 40% presents after an out-of-hospital cardiac arrest. He was playing golf with a friend when he was noted to suddenly collapse. CPR was initiated and EMS was contacted. An automatic external defibrillator (AED) was available and was used to defibrillate the patient. Interrogation of the AED revealed the patient to be in ventricular tachycardia (Figure 63-4). Upon arrival to the emergency department, routine laboratory work revealed a low potassium level of 3.2 mmol/L. The patient was started on potassium replacement, and a single chamber implantable cardiac defibrillator (ICD) was placed. At follow-up, his potassium level had remained in the normal range; however, interrogation of his ICD revealed several episodes of ventricular tachycardia that were pace-terminated.
FIGURE 63-4 Rhythm strip of initial rhythm prompting defibrillation from AED.
ETIOLOGY
There are several mechanisms by which sudden cardiac death (ventricular tachycardia/ventricular fibrillation [VT/VF]) can be can be caused by potentially reversible causes. The most common of these include electrolyte imbalances, drugs, and ischemia.1
Electrolyte Abnormalities
Hypokalemia
Hypokalemia is a common electrolyte abnormality that is encountered during clinical practice. It can be observed in as many as 20% of hospitalized patients.2 This prevalence is notable among cardiac patients, as the most common cause of hypokalemia is the use of diuretics, mainstay therapy for hypertension and heart failure.2 See Table 63-1 for major causes of hypokalemia.
TABLE 63-1 Major Causes of Hypokalemia
Causes of Hypokalemia
Renal losses |
• Diuretic use |
• Renal tubular acidosis |
• Hypomagnesemia |
• Mineralocorticoid excess |
Gastrointestinal loses |
• Diarrhea |
• Emesis |
• Laxatives |
• Drainage (naso-gastric tube, G-tube, etc.) |
Intracellular shift |
• Alkalosis |
• Excess insulin |
• Hypothermia |
• Use of beta-agonists |
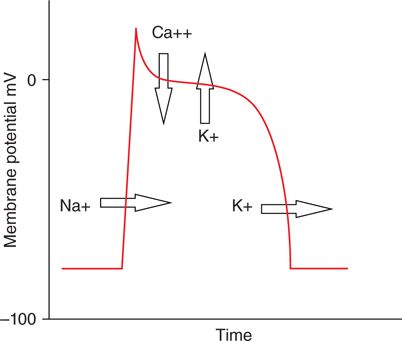
Potassium is necessary in the maintenance of the cardiac myocyte resting transmembrane potential as well as repolarization of the cardiac action potential3,4 (Figure 63-5). As such, alterations in the serum potassium concentration can have important cellular electrophysiolgic effects. Specifically, low serum potassium concentrations decrease the outward delayed rectifier current (IKr), prolonging repolarization.3 This may occur through internalization and degradation of the HERG channels that are responsible for IKr, which has been demonstrated to occur at low serum potassium concentrations.5 The electrocardiographic results of hypokalemia can be prolongation of the QT interval predisposing to malignant ventricular arrhythmias and torsades de pointes.3,5
FIGURE 63-5 Cardiac action potential with ion movements during the various phases. Sodium and calcium ions entering the cell; potassium ions moving out of the cell during repolarization.
Hyperkalemia
While not as common as hypokalemia, hyperkalemia can occur in up to 8% of hospitalized patients. Hyperkalemia is most commonly observed in patients with renal insufficiency and as a consequence of medications.6 Please see Table 63-2 for causes of hyperkalemia.
TABLE 63-2 Major Causes of Hyperkalemia
Causes of Hypokalemia
Reduced excretion |
• Acute and chronic kidney disease |
• Aldoseterone deficiency |
• Volume depletion |
Extracellular shift |
• Acidosis |
• Hyperglycemia |
• Beta blockers |
• Exercise |
Drugs |
• Digoxin |
• SuccinyIcholine |
• Calcineurin inhibitors |
• Minoxidil |
The cardiac myocyte resting membrane potential is maintained at approximately –90 mV.3 As extracellular potassium levels increase, as in the setting of hyperkalemia, the resting membrane potential decreases. This change in resting membrane potential affects the number of voltage gated sodium channels available for activation during phase 0 of the action potential. As the number of sodium channels available decreases, the magnitude of the inward sodium current decreases, resulting in slowing of impulse propagation and prolongation of membrane depolarization. As potassium levels continue to rise, membrane depolarization continues to lengthen with widening of the QRS and eventual merging with the T wave, producing a sine wave pattern. Once this is observed, without normalization of the potassium level, ventricular fibrillation and asystole are almost certain.7
Hypomagnesemia
Hypomagnesemia is another frequently occurring electrolyte abnormality, occurring in up to 12% of hospitalized patients.8 Similar to potassium, the use of diuretics, both loop and thiazide-type, can result in renal magnesium wasting.9 Other medications, such as the frequently prescribed proton pump inhibitors, can also cause hypomagnesaemia through decreased absorption.10
The effects of magnesium on the cardiac action potential most likely occurs through its interactions with the ion channels of other cations. Magnesium within the cardiac cell functions to block cellular potassium channels thus limiting efflux of intracellular potassium. This action is crucial in promoting the potassium flow that comprises the inward rectification current.11 Magnesium also influences calcium movement through L-type Ca++ channels, which work with the rectification current to maintain the phase 2 plateau of the cardiac action potential.3,11 Increase in either of these currents, resulting from magnesium depletion, decreases the cardiac action potential and thus increases susceptibility to arrhythmias.12
Hypocalcemia
Hypocalcemia is most frequently encountered in patients with chronic renal insufficiency.6 During phase 2 of the cardiac action potential, influx of calcium though L-type Ca++
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree