FIGURE 10-1 Twelve-lead ECG during tachycardia (A) with LBBB QRS morphology similar to that in sinus rhythm (B).
In the ED the patient recalled having episodes of palpitations for the past 3 years. Initially she described intermittent “blips” in her chest without associated chest pain or dyspnea. Later, episodes of palpitations became more frequent and more protracted, prompting two prior visits to the ED. Each time tachycardia, thought to be supraventricular tachycardia, resolved with adenosine. The patient received diltiazem, with limited improvement in the frequency and duration of the episodes of palpitations. Three years prior to the current presentation she was diagnosed with LBBB. At that time the workup included an echocardiogram that revealed left atrial enlargement and normal left ventricular systolic function, and an exercise myocardial perfusion imaging stress test without evidence of ischemia or infarction.
Given the recurrent episodes of symptomatic supraventricular tachycardia, the patient underwent an electrophysiology (EP) study. With ventricular pacing, the atrial activation was eccentric—earliest at the distal dipole of the coronary sinus catheter situated in a lateral position (CS 1-2; Figure 10-2) suggesting retrograde conduction via a lateral accessory pathway (AP). With atrial pacing, conduction was decremental, via the AV node. The retrograde effective refractory period of the AP was 330 ms at a 600 ms driving train. At baseline, single echos were seen (Figure 10-3). Supraventricular tachycardia with a cycle length of 400 ms (heart rate 150 bpm) was induced with atrial extrastimuli (Figure 10-4). The surface ECG was similar to the ECG on presentation in the ED. The earliest atrial activation was again at the CS 1-2 electrode. Ventricular entrainment revealed a VAV response. His-synchronous PVCs advanced the subsequent A as well as the tachycardia (Figure 10-5). These maneuvers were consistent with orthodromic atrioventricular reentrant tachycardia (AVRT), using a concealed left lateral AP. A transseptal puncture was performed, and radiofrequency applications were delivered to the area of the earliest activation at the left lateral region during ventricular pacing. Pathway conduction was abolished at the successful site after 3 seconds of RF application (Figure 10-6). Postablation there was midline and decremental AV conduction with no evidence for dual AV nodal physiology. There was no retrograde VA conduction. The patient tolerated the procedure well. At follow-up there has been no recurrence of arrhythmia symptoms, and the ECG remained unchanged.
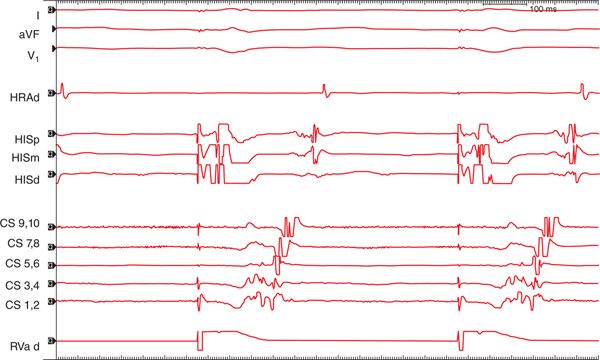
FIGURE 10-2 With ventricular pacing the atrial activation was eccentric—earliest at the distal dipole of the coronary sinus catheter (CS 1-2) suggesting retrograde conduction via a left lateral accessory pathway. Tracings are shown from surface leads I, aVF, and V1 as well as HRA, His proximal (HISp), mid (HISm), and distal (HISd), coronary sinus (CS) proximal (9,10) to distal (1,2), and right ventricular apex (RVa).
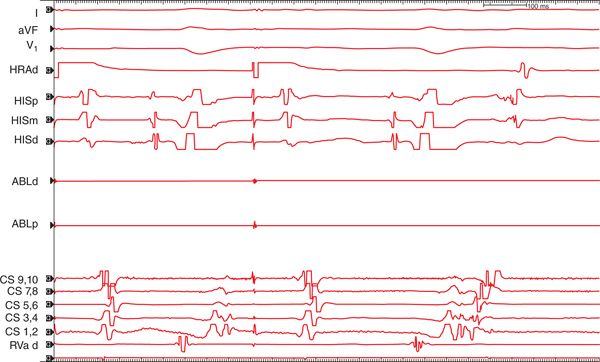
FIGURE 10-3 Single atrial echo beats were seen with atrial extrastimuli. Tracings are shown from surface leads I, aVF, and V1 as well as HRA, His proximal (HISp), mid (HISm), and distal (HISd), ablation catheter distal (ABLd) and proximal (ABLp), coronary sinus (CS) proximal (9,10) to distal (1,2), and right ventricular apex (RVa).
FIGURE 10-4 Supraventricular tachycardia with cycle length of 400 ms (heart rate 150 bpm) was induced with an atrial extrastimulus. Tracings are shown from surface leads I, aVF, and V1 as well as HRA, His proximal (HISp), mid (HISm), and distal (HISd), coronary sinus (CS) proximal (9,10) to distal (1,2), and right ventricular apex (RVa).
FIGURE 10-5 His-synchronous PVCs advanced the subsequent A as well as the tachycardia. Tracings are shown from surface leads I, aVF, and V1 as well as HRA, His proximal (HISp), mid (HISm), and distal (HISd), coronary sinus (CS) proximal (9,10) to distal (1,2), and right ventricular apex (RVa).
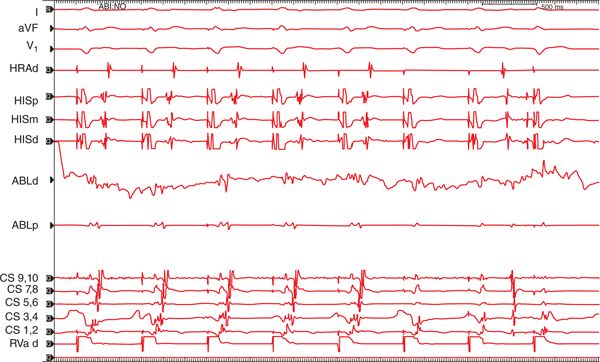
FIGURE 10-6 Pathway conduction was abolished at the successful site after 3 seconds of radiofrequency ablation. Tracings are shown from surface leads I, aVF, and V1 as well as HRA, His proximal (HISp), mid (HISm), and distal (HISd), ablation catheter distal (ABLd) and proximal (ABLp), coronary sinus (CS) proximal (9,10) to distal (1,2), and right ventricular apex (RVa).
EPIDEMIOLOGY, ETIOLOGY, AND PATHOGENESIS
AVRT is the second most common cause of paroxysmal supraventricular tachycardia, but the etiology of AP formation remains largely unknown.1,2 It is not clear whether the development of atrioventricular connections is genetically determined,3 due to some environmental exposure, or due to other factors.1
The APs are located in the left free wall in approximately 60% of patients undergoing RF ablation, in or adjacent to the interventricular septum in 20% to 30% of patients, and in the right free wall in about 10% of patients.4,5
There are gender differences in the clinical characteristics of the APs. Women seem have more concealed accessory pathways (59%) than men (50%).5 Orthodromic AVRT is more frequent than antidromic AVRT in both men and women.5 The left free wall locations are similarly encountered in men and in women.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree