FIGURE 8-1 Initial ECG revealing sinus rhythm with a normal axis and intervals and no evidence of preexcitation.
SIGNS/SYMPTOMS
The history and symptoms are quite consistent with AVNRT, which is typically characterized by an abrupt onset and termination. Episodes may last from seconds to hours. Many patients will report that they will often experience the episodes after they lean over to pick something up. The heart rate is usually rapid, ranging from 150 to 250 beats per minute (bpm). It is usually 180 to 200 bpm in adults; in children, the rate may exceed 250 bpm. In the absence of structural heart disease, it is usually well tolerated.
Common symptoms include the following:
• Palpitations
• Dizziness
• Anxiety/nervousness
• Lightheadedness
• Chest discomfort/fullness
• Neck pulsations (often due to near simultaneous contraction of the atria and ventricles)
• Presyncope
Syncope is rare, but may occur in patients with a rapid ventricular rate or prolonged tachycardia due to poor ventricular filling, decreased cardiac output, hypotension, and reduced cerebral perfusion.
The lack of ECG documentation is not unusual as these episodes are often quite brief. In the atypical form of AVNRT the ECG often reveals a long RP interval and can be misinterpreted as sinus tachycardia; however, the P waves (if discernable) are usually inverted in the inferior leads (II, III, and AVF).
EPIDEMIOLOGY
Paroxysmal supraventricular tachycardia (PSVT) has a prevalence of 2.25 per 1000 population and an incidence of 35 per 100,000 person-years. AVNRT is the most common cause of PSVT and is the underlying arrhythmia in 60% of these patients.1–3 Of the patients presenting with AVNRT, 11% to 15% will present with the atypical form.4–7 There is a 3:1 predominance of AVNRT in women.8–10 AVNRT may occur in persons of any age. It is common in young adults, but some patients do not present until their seventh or eighth decade or later. AVNRT is considered less common in newborns and increases in prevalence throughout childhood. However, some reports suggest that AVNRT may be underrecognized in infancy.11
ETIOLOGY AND PATHOPHYSIOLOGY
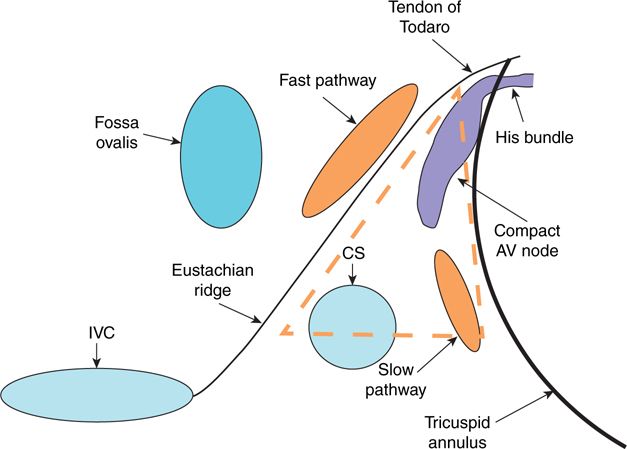
AVNRT (typical and atypical) occurs due to reentry within two (or more) anatomically and functionally distinct pathways located within the region of the AV node; they are known as the fast and the slow pathways and have different electrophysiologic characteristics. The fast pathway is characterized by its more anterior and superior location within the right atrial septum and its relatively shorter conduction time and longer effective refractory period (ERP), whereas the slow pathway is typically located inferiorly and posteriorly and has a relatively longer conduction time and an ERP that typically is short when compared to fast pathway ERP (Figure 8-2). There may be multiple slow pathways in as many as 5% of patients with AVNRT.12 As previously mentioned, these separate pathways are usually anatomically discrete, but dual AV nodal physiology is a common finding during EP studies and is not synonymous with AVNRT. There are two forms of AVNRT that are usually described and include the typical form (ie, slow-fast) and the atypical form (ie, fast-slow or slow-slow), referring to the anterograde-retrograde conduction over the pathways during tachycardia. In the typical form the conduction moves in the anterograde direction through the slow pathway and in the retrograde direction through the fast pathway. In the atypical form, the conduction moves either anterograde in the fast pathway and retrograde in the slow pathway, or anterograde and retrograde through two slow pathways. Either of these scenarios can result in a long RP interval during tachycardia.6,7,13–18 Typically, retrograde CS activation is concentric (Figures 8-3A and B and 8-4) as the inputs of the fast and slow pathways usually reside at the anterior/superior right atrial septum and the inferior/posterior right atrial septum, respectively. However, eccentric CS activation is seen in approximately 5% of all AVNRT and 32% to 80% of atypical AVNRT due to leftward inferior nodal extensions which are densely populated with transitional cells.7,15,18 In most patients with AVNRT, the tachycardia is initiated when a premature complex (atrial or ventricular) is blocked in the one pathway (usually the fast pathway with a longer refractory period) and conducts in the other pathway (usually the slow pathway with a shorter refractory period). While the impulse conducts in one pathway, the other pathway recovers so that the impulse can conduct in the opposite direction thus completing the loop of reentry.
FIGURE 8-2 Schematic representing an RAO projection of the right atrial septum. The fast and slow pathways are depicted in red and yellow, respectively. The dotted red line represents the borders of the triangle of Koch.
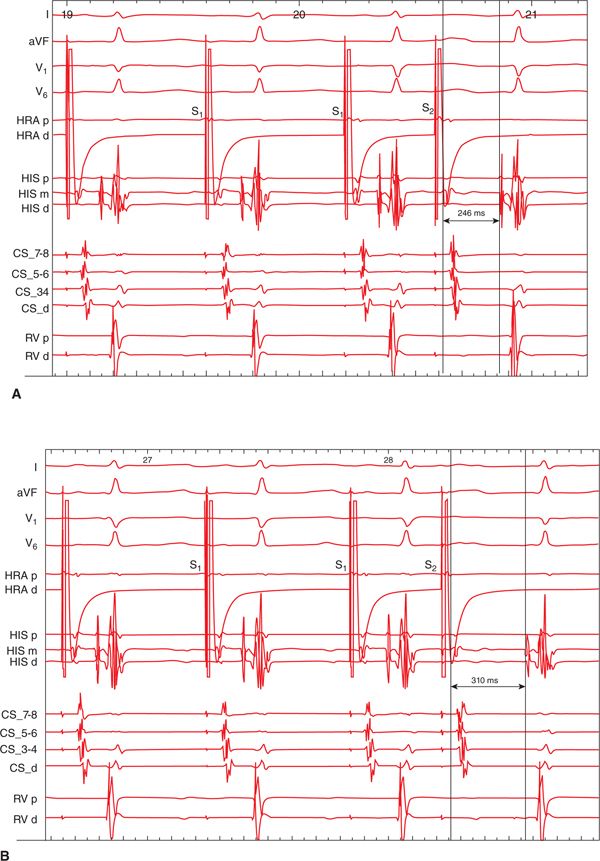
FIGURE 8-3 Programmed electrical stimulation is performed from the high right atrial catheter. Simultaneous recordings are taken from the proximal and distal high right atrium (HRA p, HRA d), the proximal, mid, and distal His bundle (HIS p, HIS m, HIS d), the proximal to distal coronary sinus (CS_7,8 to CS_d), and the proximal and distal right ventricular apex (RVA p, RVA d). (A): Decremental conduction has occurred down the fast pathway, and the AH interval measures 246 ms. (B) After a 10-ms decrement in the S2, there is a 64 ms “jump” in the AH interval consistent with dual AV nodal physiology.
FIGURE 8-4 Typical AVNRT in this patient as evidenced by a long AH interval and short VA interval during tachycardia.
DIAGNOSIS
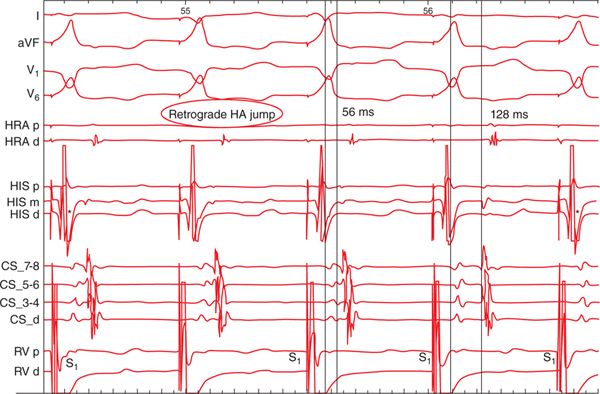
The definitive diagnosis of AVNRT (typical or atypical) can only be made with electrophysiologic testing. The hallmark of AVNRT is the presence of dual AV node physiology which is defined as a >50 ms “jump” in the atrial-His interval (AH) between a 10 ms S1S2 decrement during atrial-programmed stimulation. This is evident in this patient (see Figures 8-3A and B and 8-4). An HA jump during ventricular pacing or programmed stimulation is frequently seen in patients with atypical AVNRT and was present in this patient (Figure 8-5).
FIGURE 8-5 During a ventricular pacing drive in this patient there is a 72-ms HA “jump” indicating a switch from conduction up the retrograde fast pathway to the retrograde slow pathway. Note that the earliest atrial activation switches from the proximal His (HIS p) to the proximal CS (CS_7,8). The asterisks on the first and last beat indicate the retrograde His deflection.
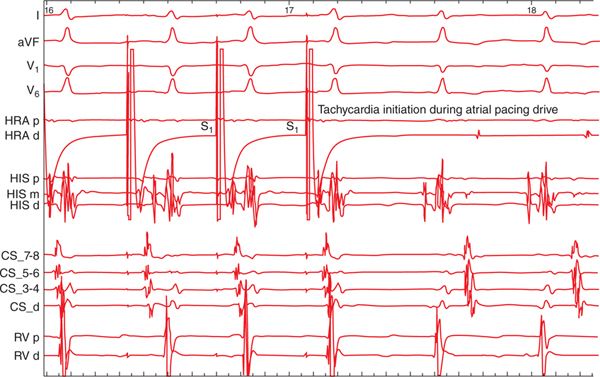
Approximately 85% of patients presenting with atypical AVNRT will also have inducible typical AVNRT.7 AVNRT can be initiated by ectopic atrial or ventricular beats. The typical form is usually initiated by atrial ectopic beats that block in the fast pathway and travel anterograde via the slow pathway. The resulting arrhythmia results in near simultaneous activation of the atria and ventricles (see Figure 8-4). The atypical form can be induced with atrial or ventricular extrastimuli or may occur during an atrial or ventricular pacing drive (Figure 8-6). Some of the distinguishing features of the various forms of AVNRT are as follows7,17:
FIGURE 8-6 Initiation of atypical AVNRT during an atrial pacing drive. Notice the long AH interval on the HIS catheter and the longer VA time when compared to the typical form in Figure 8-4.
 Slow-fast → VA <60 ms and AH > HA during tachycardia, earliest retrograde atrial activation at the His bundle
Slow-fast → VA <60 ms and AH > HA during tachycardia, earliest retrograde atrial activation at the His bundle
• Atypical
 Fast-slow → often no jump seen, VA >60 ms and HA > AH during tachycardia, earliest retrograde atrial activation near CS os
Fast-slow → often no jump seen, VA >60 ms and HA > AH during tachycardia, earliest retrograde atrial activation near CS os
 Slow-slow → AH jump often seen, VA >60 and AH > HA during tachycardia, earliest retrograde atrial activation near CS os
Slow-slow → AH jump often seen, VA >60 and AH > HA during tachycardia, earliest retrograde atrial activation near CS os
There is frequently quite a bit of cycle length variability during atypical AVNRT, which may be due to multiple slow pathways or presence of an upper or lower common pathway6,12,15,16 and is seen in this patient (Figures 8-7 and 8-8).
FIGURE 8-7 Beat-to-beat variations in the VA time during atypical AVNRT in this patient. Note the long VA time (>100 ms).
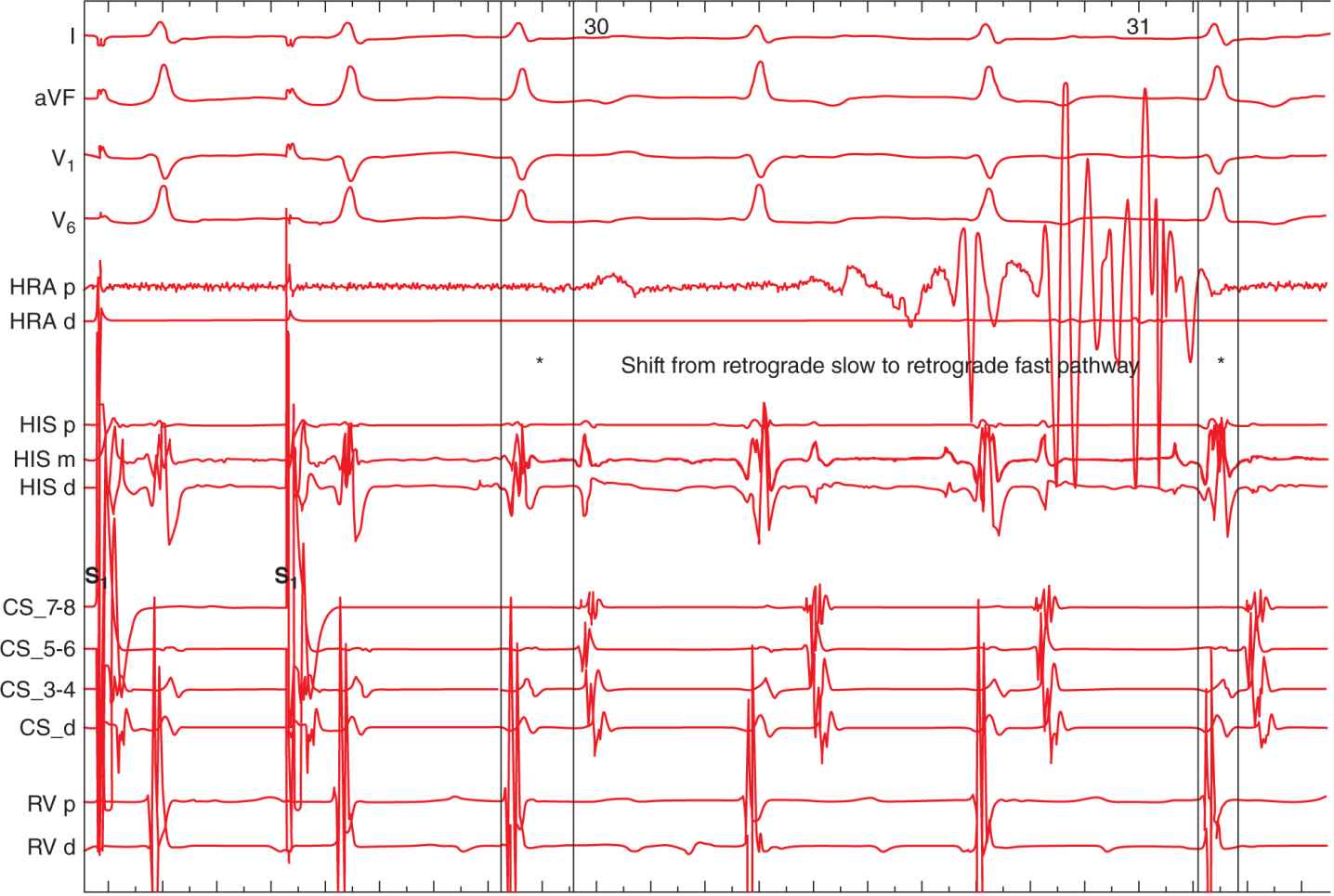
FIGURE 8-8 Example of a switch from the retrograde slow pathway to the retrograde fast pathway during tachycardia. Note the difference in VA times between the beats annotated with asterisks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree