Atypical Lymphoid Hyperplasia
Definition
Hyperplasia with atypical histologic or cytologic features of lymph nodes (or of other lymphoid organs), suggestive but not diagnostic of lymphoma.
Pathogenesis
Atypical lymphoid hyperplasia (ALH) is neither a clinical nor a pathologic entity, but rather a diagnostic category comprising borderline cases in which a definite determination of benign or malignant lesion cannot be made by microscopic examination (1). Some of these cases may represent early lymphomas, and others, abnormal lymph node reactions to various antigenic stimulants.
In persons with primary immunodeficiency diseases, such as ataxia telangiectasia or Wiskott-Aldrich syndrome, the incidence of lymphomas is increased (2), and these patients also show atypical lymph node reactions that cannot be classified. In a series of 35 lymphoreticular disorders that developed in patients with primary immunodeficiency, three (8.5%) were unclassifiable and considered to represent reactive phenomena in immunologically abnormal hosts (3).
In several retrospective studies of lymph node biopsies, patient follow-up was used to assess the subsequent course of nondiagnostic lesions and lesions diagnosed as atypical hyperplasia. In one review of 379 biopsies of peripheral lymph nodes, 158 were nondiagnostic and 12 were diagnosed as atypical hyperplasia. Lymphomas developed in seven of these patients (4). Sinclair et al. (1) reviewed 135 biopsies of enlarged superficial lymph nodes. Fifty (27%) of these were nondiagnostic, and lymphomas occurred in nine. In the series of Saltzstein (5), 105 of 177 patients undergoing lymph node biopsy had no specific pathologic diagnosis; however, 56 (53%) in the next 6 months showed a disease related to the initial indication for biopsy. In a survey of 600 cases referred for a second histologic opinion after an initial biopsy of Hodgkin disease, Symmers (6) found the diagnosis to be incorrect in 283 cases (47%). In 14 cases, he considered the lesion to be unclassifiable; seven of these patients died with lymphomas and seven recovered completely. Finally, when Schroer and Franssila (7) reviewed 70 cases in which a diagnosis of atypical hyperplasia of lymph nodes had been made, they found that a malignant lymphoproliferative disease had developed in 37% of the patients during the following 2 to 13 years. The atypical hyperplasia represented 3.1% of all lymph node biopsies performed during the same period (7).
Some clinicopathologic entities, such as progressive transformation of germinal centers (see Chapter 34), iatrogenic lymphadenopathies (see Chapters 45 and 46), Kikuchi lymphadenopathy (see Chapter 37), rheumatoid lymphadenopathy (see Chapter 40), human immunodeficiency virus (HIV) lymphadenitis (see Chapter 15), angioimmunoblastic lymphadenopathy/lymphoma (see Chapter 75), and others, exhibit features of ALH and possibly were included in this category before they were described as separate entities.
Lymphoproliferative disorders are hyperplastic reactions of lymphoid tissues that develop in recipients of organ transplants (8,9) (see Chapter 81). They may also develop in persons with primary or acquired immunodeficiency (10) (see Chapter 82). Lymphoproliferative disorders may encompass a whole spectrum of lymphoid proliferations, from benign reactive lymphoid hyperplasia (RLH) to non-Hodgkin lymphoma (NHL) of high-grade large-cell type. Whereas a diagnosis at either of the two extremes of this spectrum is not particularly difficult, in a significant number of cases, a histologic determination of benign or malignant cannot readily be made, and such lesions are therefore referred to as lymphoproliferative lesions. The term is noncommittal and reflects the difficulty of reaching a firm histologic diagnosis. The microscopic appearance is essentially that of ALH, showing various types of histologic or cytologic atypia. The observations of spontaneous regression of some lesions diagnosed as lymphomas after discontinuance of immunosuppressive treatment raise further questions about the accuracy of histologic diagnosis in some cases of atypical lymphadenopathies.
Artifactual changes in cytology and histology are commonly produced by faulty techniques in the processing of lymph nodes. Uneven fixation, incomplete dehydration, and poor staining can cause tissue alterations that are often misinterpreted as atypical or even malignant changes. Although it has been frequently stated (11,12,13), it cannot be overemphasized that the correct reading and interpretation of lymph node sections requires nearly perfect processing techniques. It is reasonable to assume that the diagnosis of ALH will be made less frequently in the future, as the processing of lymph nodes improves and the interpretation of changes is facilitated by a better characterization of old and new entities. Nevertheless, if a clear conclusion cannot be reached, and if the diagnosis of ALH is a matter of concern, the clinician should not hesitate to suggest a repeated lymph node biopsy and include appropriate immunohistochemical and molecular examinations.
Clinical Syndrome
Systemic symptoms such as fever, night sweats, anorexia, and fatigue appear to be more common in patients in whom lymphomas ultimately develop than in those in whom they do not (1). It also seems that lymph node enlargement limited to one area correlates with a more favorable prognosis than does generalized enlargement. Abnormal peripheral blood counts and morphology are generally unfavorable prognostic features. Although the clinical information is contributory and should be considered in every case, most authors agree that the final pathologic diagnosis must be based on histologic findings (7,11).
Histopathology
Atypical lymphoid hyperplasia has no characteristic histologic pattern. In some cases, the architecture is nodular; in others,
it is diffuse (7). Both patterns are similar to those described in RLH (see Chapter 32).
it is diffuse (7). Both patterns are similar to those described in RLH (see Chapter 32).
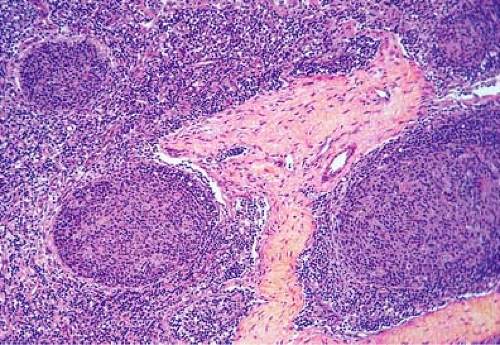
In the nodular type of ALH, the number of lymph node follicles is increased, and their size and shape vary greatly. Elongated, angulated, and dumbbell-shaped nodules, frequently coalescing, are common (14). The germinal centers are large and include various types of cells and frequent mitoses. In children, RLH may be particularly exuberant, resulting in enlarged lymph nodes with numerous follicles and hyperreactive germinal centers that may not exhibit the usual starry-sky pattern with numerous tingible-body macrophages (Fig. 33.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree