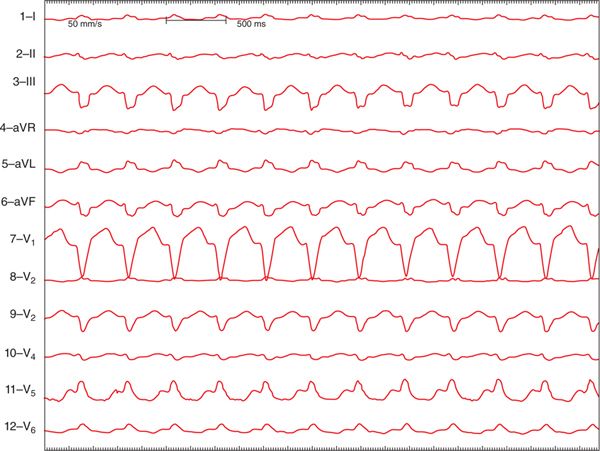
FIGURE 12-1 Twelve-lead ECG demonstrating a long RP supraventricular tachycardia at a rate of 130 bpm. Note the deeply inverted P waves in the inferior leads (II, III, aVF), which clearly distinguish this from sinus tachycardia.
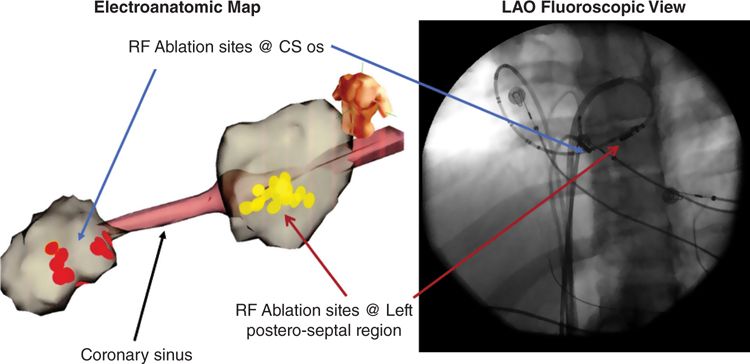
He was referred to the electrophysiology service for evaluation of possible catheter ablation of his arrhythmia. An electrophysiology study was performed which demonstrated an incessant atrioventricular (AV) reentrant tachycardia utilizing a decremental posteroseptal accessory pathway (AP) with a long conduction time. Mapping during tachycardia revealed a broad atrial insertion of the pathway spanning across the posteroseptal space from the mouth of the coronary sinus ostium to the left posteroseptal region of the mitral annulus. Ablation at the coronary sinus ostium and posteroseptal mitral annulus via a transeptal approach terminated the tachycardia and eliminated pathway conduction (Figure 12-2). The patient was seen at follow-up 2 months after the ablation procedure. His symptoms had abated, no further tachycardia was noted on Holter monitoring, and there was normalization of the ejection fraction by echocardiography.
FIGURE 12-2 Shown in this figure are the electroanatomic map and fluoroscopic view of the ablation procedure. The blue and red arrows point to the ablation sites at the coronary sinus ostium (CS os) and left posteroseptal region, respectively. The pathway had a broad atrial insertion requiring ablation on both sides of the posteroseptal space for elimination.
EPIDEMIOLOGY
This patient had a classic case of permanent junctional reciprocating tachycardia (PJRT). PJRT is a long RP tachycardia that is associated with deeply negative P waves in the inferior leads and is caused by an “atypical” AP.
A “typical” AP is one that has a rapid and fixed conduction time and is located along the AV groove anywhere except at the anteromedial mitral annulus where the aortic valve sits.1,2 Both the atrial and ventricular insertions of a typical AP are close to the mitral or tricuspid valve annulus.
A simple definition of an “atypical” accessory pathway is any AP that has either unusual conduction characteristics (long conduction time or decremental conduction) or an unexpected location.
Pathways with unusual locations such as those coursing through the fibrous region of the aortomitral continuity, traveling around the aortic valve through the left anteroseptal region or connecting directly between the right or left atrial appendage and the ventricles, are very rare and have been reported only in small series or isolated case reports.3–6
During electrophysiologic testing in patients with an AP, the probability of finding decremental pathway conduction is not rare and in one series was reported to be on the order of 10%.7 In the majority of cases from this series, the pathways had relatively short conduction times with decremental conduction in the retrograde direction. The most common location for a decremental pathway was in the posteroseptal region (47%).7
Two specific variants of atypical APs occur frequently enough and have consistent enough characteristics to form distinct clinical subgroups. These are pathways associated with PJRT and Mahaim fibers. Both of these pathways types are fairly rare, and each type accounts for less than 2.5% of pathways in large ablation series of adult patients.7–9
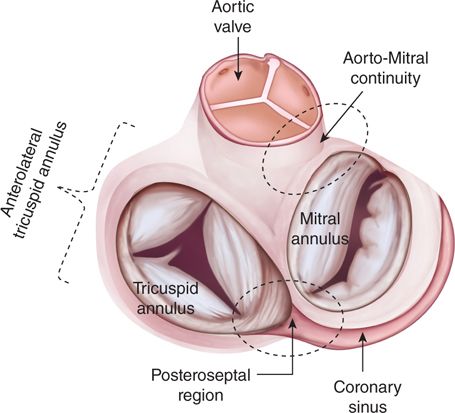
The locations of the most common sites for atypical APs are shown in Figure 12-3.
FIGURE 12-3 The most common locations for atypical accessory pathways are shown in the areas outlined with a dashed line. The most common variant of Mahaim fibers, atriofascicular pathways, are located along the anterolateral tricuspid annulus. The posteroseptal region is the usual location for pathways responsible for PJRT and is the most common location for any pathway with decremental conduction properties. Pathways located in the aortomitral continuity are atypical by virtue of their location; very rarely pathways can traverse this area, which is a region of dense fibrous tissue that separates the left atrium and ventricle.
ETIOLOGY AND PATHOPHYSIOLOGY
APs of the PJRT type have very long conduction times with decremental conduction properties. These pathways essentially only conduct in the retrograde direction and are therefore concealed on the baseline ECG. They are usually located in the posteroseptal region close to the coronary sinus ostium (75% of patients), but pathways with these conduction characteristics can also be found in other locations.10
The characteristic tachycardia associated with this type of pathway is a long RP tachycardia with deeply inverted P waves in the inferior leads. The P wave timing is due to the long VA conduction time of the pathway and the morphology of the P wave is the result of earliest activation of the atrium being near the coronary sinus ostium. These tachycardias can be paroxysmal in nature, but in a high percentage of patients they can be nearly incessant. In one large ablation series of 49 patients with PJRT type pathways, the tachycardia was incessant in 47% and led to a tachycardia-induced cardiomyopathy in 16% of cases.10
Mahaim fibers, on the other hand, are APs with long conduction times and decremental conduction properties that conduct in the antegrade direction only. These pathways are typically very long in their course, usually originating in the anterolateral right atrium and inserting in the distal right ventricle near the right bundle branch.11 They behave like a duplicate AV node and His-Purkinje system and are referred to as atriofascicular pathways. The tachycardias associated with these pathways are wide complex preexcited tachycardias with a left bundle branch block configuration (Figure 12-4).
FIGURE 12-4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree