Chapter 6 Attention deficit hyperactivity disorder (ADHD)
With contribution from Dr Lily Tomas
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) — characterised by attention-deficit, impulsivity and hyperactivity — is one of the most common neurobehavioral disorders affecting children and adolescents today.1, 2, 3 The incidence of ADHD is rising with the annual prevalence in Australia in 2001 being estimated at 11% (diagnosed by DSM-IV criteria), equating to a 7.5% prevalence in people aged 6–17 years.4
There has been a concomitant rise in the use of stimulant medications, namely phenylmethidate and dexamphetamine, despite a lack of studies regarding long-term social and psychological effects, and cardiovascular and neurophysiological clinical effects. Although stimulants are very helpful in 60–70% of patients, many families seek alternatives because of adverse reactions, lack of compliance and the fact that stimulants cannot be given late in the day, limiting the benefits largely to school hours.5
The use of complementary and alternative medicines (CAM) for ADHD has increased, both by parents and health care providers.6 Parents are especially drawn to CAM interventions in order to avoid or decrease the use of psychotropic medications.7, 8 Because of the wide-ranging disruptive impact on the lives of both patients and their families, an integrative approach to management simply reflects the multifactorial aetiology and nature of this disorder.
A recent Australian survey demonstrated that the most common CAM therapies used include dietary modification, nutritional supplementation, aromatherapy and chiropractic. It has been advised that doctors should always inquire about the use of CAM and use available resources to help guide families in their therapeutic choices.9
The exact aetiology of ADHD is unknown and, indeed, may differ from individual to individual. Genetics and genetic polymorphisms certainly play a role, however, major aetiological contributors may also include adverse responses to food additives, intolerances of foods, differing biochemical pathways and nutritional deficiencies, sensitivities to environmental chemicals and exposure to neurodevelopmental toxins such as heavy metals and tobacco smoke.10–15
ADHD is a complicated condition that requires multidimensional treatment strategies.16 It is imperative to understand that the aetiology and hence the management of ADHD may be different for each individual. One must attempt to elucidate all possible contributory factors and eliminate or treat each respectively.
The PFC, especially the right hemisphere, is crucial to the regulation of behaviour and attention. It is extremely sensitive to its neurochemical environment, with either too much or too little catecholamine release weakening the individual’s cognitive control of both behaviour and attention.17
Individuals with ADHD are known to have depleted levels of dopamine and noradrenaline most likely as a result of dysfunctional transporter systems.18 The role of other neurotransmitters such as histamine, acetylcholine, glutamine and serotonin in modulating catecholamine pathophysiology in ADHD is yet to be elucidated.19
Lifestyle
Most of the lifestyle factors associated with ADHD are covered under the appropriate headings below.
Mind–body medicine
Neurobiofeedback
Electroencephalogram (EEG) biofeedback is a promising alternative treatment for patients with ADHD.20 It is a form of behavioural training aimed at developing skills for the self-regulation of brain activity.21 Most individuals with ADHD, as compared to matched peers, show abnormal functioning of their anterior cingulate cortex with excess slow-wave (theta) activity and reduced fast-wave (beta) activity during tasks of selection attention.22, 23
In particular, it is well documented that hyperactive behaviour in many children with ADHD is due to abnormally enhanced 4-8Hz Theta activity in both frontal and central cortical areas of the brain.24 In the last decade there has been a multitude of clinical trials and literature reviews that demonstrate the positive effects of biofeedback on these children with clinical improvement being primarily directly related to declining theta/beta ratios and/or amplitudes over the frontal/central cortex.25–42 These have largely been good quality studies that have tended to overcome the methodological shortcomings of earlier studies.21
Research findings published to date indicate a positive clinical response (reduced hyperactivity and impulsivity, improved attention, IQ, processing speed and music performance) in approximately 75% of patients treated in controlled group studies. The Association for Applied Psychophysiology and Biofeedback and the International Society for Neuronal Regulation deem EEG biofeedback to be ‘probably efficacious’ for the treatment of ADHD, particularly for those patients who do not respond to medications.30, 36, 38
During biofeedback, individuals are taught to increase their beta activity and suppress their theta activity over a period of usually 30 or more sessions.29, 30, 32, 33 This enables the child to become an active agent of their own coping strategies and thus increase their internal locus of control.43 EEG biofeedback therapy works by rewarding scalp EEG frequencies that are associated with relaxed attention and suppressing those frequencies associated with under or over-arousal.20 It provides immediate feedback to the individual about his/her brain-wave activity in the form of a video/computer game, the action of which is influenced by the individual meeting predetermined threshold of brain activity.22 Obviously, the child must be at an age where they are able to play such games — most studies include children aged 6 years and above.28, 29, 30, 33
There are many different forms of biofeedback available. The regulation of cortical excitation thresholds are also considered to be impaired in children with ADHD and the training of slow cortical potentials addresses the regulation of cortical excitability. It has been suggested that the regulation of fronto–central negative slow cortical potentials affects the cholinergic-dopaminergic balance, allowing children to adapt to task requirements with more flexibility.21, 25, 30
Recently published studies using quantitative EEG (QEEG) techniques indicate that power spectral analysis and event-related cortical potentials may be useful in differentiating ADHD from other disorders, such that QEEGs may be used clinically in the assessment, diagnosis and treatment of ADHD.25, 35 In particular, a deficit in low frequency wave (approximately 1 Hz) activity associated with levels of hyperactivity and impulsivity has been demonstrated in both children and adolescents with ADHD. This marker is evident across a range of tasks and may, indeed, be specific to ADHD.25
Several recent neuro-feedback trials have demonstrated comparable results with Methylphenidate (Ritalin) in terms of increased attention span and reduced problem behaviour (impulsivity and hyperactivity) in children with ADHD without the side-effects often associated with medication.20, 22, 31, 37, 39, 44
It is also important to note that in those studies of children using both biofeedback and methylphenidate, only those children who had received biofeedback sustained these gains when reassessed without Ritalin. Furthermore, Quantitative Electroencephalographic Scanning Process (QESP) studies show a significant reduction in persistent cortical slowing only in those patients who underwent EEG biofeedback.39, 45 This is confirmed by parent and teacher evaluations who report significant behavioural and cognitive improvements for at least 6 months after the cessation of treatment.29
Psychosocial and/or cognitive behaviour therapy (CBT)
Although pharmacological treatments have traditionally been considered the first-line therapy for ADHD, many individuals continue to experience major functional impairment or choose not to use such medications. Behavioural school interventions and parent training have been supported by empirical evidence.1, 46 It is important to note, however, that the children respond to such behavioural interventions only when they are appropriately implemented both at home and in the classroom setting.47
Psychosocial therapies, especially behavioural modification techniques, should be considered for children with ADHD and oppositional behaviours whilst cognitive behaviour therapy (CBT) may be useful for adolescents and adults.48, 49 When behavioural therapies have been combined with medication, improvements in function have been demonstrated and the amount of stimulant reduced.50
A recent Cochrane review has confirmed that both behavioural and CBT interventions are highly effective, however, access to these treatments is limited due to length of consultations and expense, with significant behavioural improvements taking up to 2 hours of therapist time.51
It has been hypothesised that family therapy without medication may help to develop family structure and may help to manage children’s behaviour. A 2005 Cochrane review has deemed that further research is necessary to determine whether family therapy is an effective intervention for children with ADHD.52
Available data supports the use of group and individual structured, skills-based psychosocial interventions for adults with ADHD.53, 54
Meditation and relaxation training
Mindfulness meditation may also improve behavioural and neurocognitive impairments in adolescents and adults with ADHD. One recent study has demonstrated improved attention and cognition with reduced anxiety and depression after an 8 week mindfulness training program.55
A range of studies have suggested that relaxation training can help children with ADHD to learn to relax, thereby decreasing their autonomic activity.7, 56 Reductions in problem behaviour, increased attention span and greater internal locus of control are other potential benefits of relaxation therapy. It should be noted, however, that these skills need to be practised regularly for continued effect.57–60
In the mainstream literature there have been no published studies on the potential application of meditation for ADHD, however, the Royal Hospital for Women, Sydney, has devised a pilot clinic aimed at developing meditative strategies, using Sahaja Yoga Meditation, to help these children (www.sesiahs.health.nsw.gov.au/rhw/). The clinic exclusively accepted children with a formal diagnosis of ADHD and whose usual supervising health professional had permitted their involvement. Both the child and at least 1 parent were required to attend classes and practice daily meditation. The results were very promising. Of the 16 children who completed the program, 6 were able to decrease and 3 were able to stop their medication whilst maintaining completely normal behavioural traits. All parents reported feeling generally better, less stressed and more relaxed and most felt the program had benefited their children.
About half the parents said their child was less restless with improved sleep and that they were experiencing a better relationship with them. Whilst this is not a randomised controlled study, it is at the moment the best available evidence for meditation’s potential role in ADHD and clearly suggests that Sahaja Yoga meditation may be particularly beneficial for this condition. More rigorously designed studies are planned in order to achieve a more conclusive understanding of this radically different approach.3
Sound therapy
Recent studies have demonstrated that children with ADHD, upon performing visual discrimination tasks, were less attentive than controls when exposed to distracting novel sounds. Event-related brain potentials correspondingly displayed significant differences over the fronto-central left hemisphere and the left parietal scalp region, revealing low control of involuntary attention that may further underlie their abnormal distractibility.61
Systems such as the ‘Tomatis Method’, ‘Integrated Listening System’ (ILS) and Dr Guy Berard’s (ENT physician) Auditory Integration Training (www.integratedlistening.com) have been designed around the brain’s ability to form new neural connections throughout life, changing the way the brain processes auditory information. ILS stimulates both cerebellar activity, in order to strengthen these neural connections, and the vestibular system, in order to improve balance, posture and hand/eye coordination. Such therapies are used by many patients who experience auditory processing difficulties and hypersensitivity to specific auditory frequencies. There are currently no well-designed studies in the literature regarding such therapies, however, anecdotal reports are very promising.
The Moderate Brain Arousal model suggests that dopamine levels modulate how much noise is required for optimal cognitive performance. Studies have shown that individuals with low dopamine levels (ADHD) need more background noise than controls for optimal cognitive performance. This positive effect of noise may be explained by the phenomenon of Stochastic Resonance (SR), whereby external noise is relayed as internal noise into the neural network subsequently affecting neurotransmitter levels.62 This method aims to teach children with ADHD to focus and intently listen to specific sounds, subsequently helping with behaviour modification, cognitive development and concentration.
Normally, high dopamine down-regulates stimuli-evoked phasic dopamine responses through autoreceptors, however, abnormally low extracellular dopamine in ADHD up-regulates these receptors so that stimuli-evoked phasic dopamine is boosted. It is postulated that these boosted phasic responses create hypersensitivity to environmental stimuli in ADHD. Empirical data supports the concept that more noise is required for SR to occur in dopamine-deprived neural systems in ADHD.17
There is also some evidence to show that music therapy may contribute to a reduction in a range of ADHD symptoms in the classroom.43, 63
Sleep and behaviour
It is important to note that, even in children that do not suffer with ADHD, sleep problems during school transitions are common, and are associated with poor outcomes. Future RCTs could determine if sleep interventions can reduce the prevalence and impact of such detrimental sleep problems.64
Sleep restoration/melatonin
There is a clear correlation between ADHD and sleep difficulties with substantial evidence that ADHD psychopathology and sleep/wake regulation share common neurobiological mechanisms. Furthermore, there may even be an overlap between ADHD and sleep disorders such as obstructive sleep apnoea and restless leg syndrome (RLS).65 Anecdotal evidence strongly suggests that magnesium assists in the treatment of RLS.
Approximately 25% of children suffering with ADHD also experience some form of sleep disorder. Unfortunately, in contrast with adults, these often go undetected. Diagnosis of these patients is critical.66 Therefore, all children with ADHD should be fully assessed for sleep disturbances because adequate treatment is often associated with improvement of symptoms and a decreased requirement for stimulant medications.65, 66
The circadian rhythm of melatonin secretion from the pineal gland is reflective of mechanisms that are in control of the sleep/wake cycle. In those individuals with primary insomnia, nocturnal plasma melatonin levels tend to be lower than in healthy controls. Melatonin has been used successfully to treat insomnia in children with ADHD.67 Several randomised double-blind placebo-controlled trials using 3–6mg melatonin for 1 month demonstrated enhanced total time asleep in children with ADHD and chronic sleep onset insomnia. Melatonin is shown to be a safe and effective treatment for sleep disorders, however this had no observable effect on other ADHD symptoms.68, 69
Environment
Outdoor play
Research on children with ADHD demonstrates significant improvement in symptoms such as inattention and impulsivity after exposure to natural views or settings. Four hundred and fifty-two parents or guardians from across the US with ADHD or Attention Deficit Disorder (ADD) children aged 5–18 years enrolled in a study to assess the benefits of playing outdoors in a natural setting.70 Compared with baseline results, outdoor activities conducted in natural environments significantly improved ADHD symptoms (difficulty in remaining focused, completing tasks, listening and following directions, and in resisting distractions) compared to activities conducted indoors or those in built outdoor settings, such as parking lots.
Heavy metals and chemicals
Lead
Lead is a common environmental contaminant such that in the year 2000, nearly 1 million preschool-aged children in the US alone were shown to have elevated blood levels (>10ug/dL).71
In 1991, the US Centres for Disease Control and Prevention (CDC) established 10ug/dL as the lowest concern for children’s blood lead levels. However, in recent years, there has been a wealth of evidence-based clinical trials demonstrating that levels below 10ug/dL may impair neurological development. In fact, there is now sufficient and compelling scientific evidence to call for the CDC to lower the blood lead action level in children to a level as low as 2ug/dL.72, 73, 74
Indeed, no level of lead exposure appears to be safe with multiple studies now demonstrating reduced IQ and academic deficits in otherwise ‘healthy’ children. There appears to be an inverse relationship between lead levels and IQ levels, particularly at levels <10ug/dL.75, 76, 77 At lower levels of toxicity, a child may have no specific individual symptoms but may certainly be affected sub-clinically.78 For this reason, health care practitioners should obtain a thorough environmental history on all children they examine.74
Having adjusted for covariates, children with 5–10ug/dL have been shown to have 5 points lower IQ scores compared to children with blood lead levels of 1–2ug/dL. Verbal IQ appears to be more negatively associated than performance IQ, as does reading and maths composite scores. Working memory and attention were also shown to be lowered with increasing lead levels.79, 80
In particular, there have been several studies associating ADHD with elevated lead levels. Individuals with ADHD are more likely to have been exposed to lead during childhood, such that ADHD may now be deemed an additional deleterious outcome of lead exposure, even when levels are <10ug/dL.81 Its effects may be mediated by less effective cognitive control, consistent with a route of influence via striatal-frontal neural circuits.82
Chelation therapy is advised for children with blood level concentrations of >44ug/dL, however, there are no evidence-based clinical trials for other gentler chelation treatment options for children with levels less than this. Because lead absorption is partially related to nutritional status, micronutrient supplements may be a possible solution for combating low-level chronic lead exposure.71, 80 Zinc, in particular, is 1 supplement that has shown some results in effectively reducing oppositional, hyperactive, cognitive problems and other ADHD symptoms in most individuals.80, 83
Mercury
Numerous studies report positive correlations between the number of dental amalgams and urinary mercury concentrations in non-occupationally exposed individuals.84, 85, 86 Experimental evidence consistently demonstrates that mercury is released from dental amalgams and is absorbed by the human body.87 However, there is much controversy regarding the effects of mercury (from dental amalgams and vaccinations) on neurodevelopment, renal and immune function.
One of the latest randomised controlled studies has confirmed that treatment of children with amalgam restorations leads to increased, albeit low level, exposure to mercury. Amalgam exposure resulted in small, transient immune deficits 5–7 days post treatment, however, it did not cause overt immune defects. The authors concluded that these changes ‘most likely did not need to be of concern to practitioners considering the use of this restorative dental material’.88 It is important to note, however, the history of what initially constituted toxic lead levels and how this has changed in recent years with accumulated evidence-based studies.
In a similar manner, mean urinary mercury concentrations have been found to be greater in children with amalgams rather than composite dental restorations.89, 90 Children treated with mercury amalgams did not ‘on average’ have statistically significant differences with respect to neuropsychological function. ‘Although it is possible that very small IQ effects cannot be ruled out’, thus far evidence-based trials largely demonstrate that dental amalgam is not associated with an increase in children’s risk of experiencing neuropsychological dysfunction.75, 90, 91, 92,
These results support the concept that some healthy children may, indeed, be out of the bell-curve, being more predisposed to toxic effects of mercury at lower levels than others. This is further highlighted by a recent trial specifically concerning children suffering with ADHD. In this study of Chinese children, a significant difference in blood mercury levels was noted between children with ADHD compared with controls, after adjustments for age, gender and parental occupations. The geometric mean blood mercury level was also significantly higher in children with inattentive and combined subtypes of ADHD. In fact, children with a blood mercury level >29nmol/L were found to have 9.69 times higher risk of having ADHD after adjustment for confounding variables. The researchers concluded that high blood mercury levels were associated with ADHD.93
Manganese/aluminium
Manganese (Mn) is an essential trace element, however, it has also been shown to be toxic at high doses. Animal studies have recently shown that intra-nasally administered Mn actually circumvents the Blood-Brain-Barrier and passes directly into the brain via olfactory pathways. Long-term exposure to inhaled Mn from shower water as a significant risk for central nervous system (CNS) neurotoxicity is currently being investigated. Similarly, existing Mn drinking water standards may also need to be revised.94
A recent study of Canadian children found that those who were exposed to drinking water that was naturally high in Mn had greater scores of hyperactivity and oppositional behaviour (Revised Connor’s Rating Scale) than controls. All children with T scores >65 had hair Mn higher than 3.0ug/g.95
It is postulated that both aluminium and Mn toxicity may potentiate oxidative and inflammatory stress, subsequently leading to impaired neurological function.96
Industrial chemicals
Available data up to 2007 show that at least 202 widely-used industrial chemicals, (including lead, methylmercury, polychlorinated biphenyls, arsenic and toluene) can damage the human brain, the researchers concluding that chemical pollution may have harmed the brains of millions of children worldwide.97, 98 The specific role these chemicals may play in the development of ADHD is not certain, but a detailed environmental history should be taken in all of those with neurodevelopmental disorders.99
Tobacco smoke, air pollution, pesticides
Environmental tobacco smoke, air pollution and pesticides have also been shown to have adverse effects on fetal growth and child neurodevelopment.100, 101, 102
Tobacco smoke
A recent systematic review has demonstrated that both prenatal and possibly postnatal tobacco smoke exposure are significantly associated with increased rates of behaviour problems and ADHD.11, 12, 14, 15 If causally linked, it is estimated that prenatal tobacco exposure may account for at least 270 000 excess cases of ADHD in American children today.13
Like stimulant medication, nicotine has been shown to lower the availability of the dopamine transporter, a significant factor in dopamine metabolism.18
Physical activity
Exercise
Exercise is considered an important part of the management of the child with ADHD as it not only increases coordination skills (that many children with ADHD lack) but it provides opportunities for social interaction.7 A recent study determining the effects of exercise on children with ADHD suggests that vigorous exercise may provide a dopaminergic adjuvant in the management of behavioural features of ADHD.103
It has also been demonstrated that adolescents with ADHD have frontal lobe deficits, particularly on the right sides of their brain. Animal studies were subsequently designed which showed that ‘rough-and-tumble’ play therapy was able to reduce hyperactivity and excessive playfulness, concluding that this may be a useful new treatment for ADHD.104
Another pilot study on Therapeutic Eurythmy — a holistic movement developed by Rudolph Steiner — has also reported shifts in the concentration and motor skills of children with ADHD.105
Yoga
Randomised controlled trials (RCTs) on the effectiveness of body-oriented therapies such as yoga for children with ADHD are lacking. The effects of yoga were recently compared to the effects of conventional motor exercises in children with ADHD. It was found that yoga was an effective complementary or concomitant treatment for children with ADHD. It should be noted that the training was especially effective for children also taking medications.106 Another study of boys with ADHD practicing yoga confirmed this finding, where yoga was particularly effective in the evening when the effects of medication were absent.107
Dietary modifications
Food elimination regimes
There has been much discussion over the last 30 years regarding the possible links between diet and behaviour of the individual with ADHD. In 1975, Benjamin Feingold, an allergist, hypothesised that an intake of salicylates in artificial flavours, colours and preservatives and/or natural salicylates may induce hyperactive behaviour and learning disabilities in children. Although Feingold demonstrated that 50% of children with ADHD improved after eliminating these substances from their diet, this has not been successfully repeated until recent years.43
The use of food elimination diets in the management of individuals with ADHD is now well documented.108–112 In fact, a strictly supervised elimination diet is considered to be a valuable instrument in determining whether dietary factors are contributing to ADHD symptoms. In a recent RCT, the number of criteria on the ADHD rating scale showed a scale reduction of 69.4%. Furthermore, comorbid symptoms of oppositional defiant disorder (ODD) also showed a significantly greater decrease in the intervention than the control group.113
There is an accumulating body of evidence that many children with behavioural problems, including ADHD, are sensitive to 1 or more food components that can negatively impact upon their behaviour.114 In 1 study, 19 of 26 children with ADHD improved dramatically after eliminating artificial colours, corn, wheat, milk, soy and oranges from their diet. It is interesting that most of the children who responded to such dietary changes had atopic histories implying that atopic children are more likely to benefit from a restricted diet.112 Other risk factors associated with a beneficial dietary response were a family history of migraine and young age.109 Another study also demonstrated a significant improvement in behaviour in 62% of 40 children with ADHD after a 2-week diet based solely on rice, turkey, pear and lettuce.115 This diet is clearly too restrictive for any child but it does demonstrate that nutrition can influence behaviour.
For children showing behaviour problems such as hyperactivity, the use of dietary manipulation tends to be a more acceptable approach to treatment than the use of drugs.116 If parents strongly suspect a specific dietary item, a trial of elimination is warranted.117 However, there are various regimes; usually this would consist of avoiding the item for 3 weeks then reintroducing it in a step-wise fashion — a little the first day, then challenging the body with a higher dose during the second day if no obvious reaction has already occurred. Depending upon the age of the child, multiple foods may be eliminated simultaneously and reintroduced separately in a similar manner under strict supervision. In conducting such dietary modifications, it is mandatory that all practitioners be aware of the dangers potentially associated with unsupervised restriction diets with children.116, 118
In general, dietary modification plays a major role in the management of ADHD and should be routinely considered as part of the treatment protocol.114 Many children with ADHD have associated digestion problems — including diarrhoea, constipation, abdominal bloating, excess burping and/or flatulence, reflux/indigestion or abdominal pain/discomfort. These are generally symptoms of deficient beneficial gut flora (probiotics) and/or food intolerances which may serve as triggers for abnormal behaviour.
A plethora of studies have now shown that food additives have also been shown to increase hyperactivity symptoms in children.119, 120 This includes a recent systematic review, which concluded that an additive-free elimination diet was considered Level II evidence with respect to its current level of evidence.121
Although the use of single food additives at their regulated concentrations are believed to be relatively safe in terms of their neuronal development, their combined effects remain unclear. Four common food additives, brilliant blue, L-glutamic acid, Quinolone yellow and aspartame were observed in combination. Neurotoxicity (measured as inhibition of neurite outgrowth) was found at concentrations of additives theoretically achievable in plasma by the ingestion of a typical snack and drink.122
Symptoms that are due to, or exacerbated by, specific food additives usually involve non-IgE mediated mechanisms that are usually less severe than those induced by food allergy.123 A recent RCT demonstrated that artificial colours and/or a sodium benzoate preservative in the diet results in increased activity in children aged 3 or 8–9 years old.124 This confirmed an earlier study where the adverse behaviour of 3-year olds from the same additives was detectable by parents but not by a simple clinical assessment.125
Despite a plethora of anecdotal reports that sugar increases hyperactivity and disruptive behaviour in the child with ADHD, there are as yet no consistent clinical trials to support this allegation.126
Like most neuropsychiatric disorders, there is evidence that ADHD is associated with increased oxidative stress and therefore increased lipid peroxidation. For this reason, it is postulated that individuals with ADHD may benefit from a whole-food, plant-based diet that is high in antioxidants and devoid of refined carbohydrate products.127
Several recent studies have also reported a possible association of coeliac disease with ADHD. In fact, ADHD-like symptomatology is markedly over represented amongst individuals with untreated coeliac disease. A gluten-free diet can result in a significant improvement of such symptoms within a short time period, such that coeliac disease (as well as gluten intolerance) should be included in the list of diseases associated with ADHD-like symptomatology.128, 129 Furthermore, a high frequency (57%) of antigliadin antibodies has been demonstrated in adult patients with neurological dysfunctions of unknown cause. In a study of children with various neurological disorders, including ADHD, 13% (compared with 9% of controls) showed positive for IgG antigliadin antibodies but negative for IgA and endomysial antibodies.130
Nutritional supplementation
Nutritional supplementation is widely used to help ameliorate the symptoms of ADHD. Many nutrients, (vitamins, minerals, essential amino acids, essential fatty acids) have direct effects on the structure and function of the human brain.131 Indeed, the role of nutrition in the prevention and management of ADHD is vital, cost-effective and extremely safe.132
Magnesium/vitamin B6
Magnesium deficiency has long been known to cause hyperexcitability with seizures in animal studies, effects that have been successfully reversed by treatment with magnesium. Significantly decreased plasma and red blood cell magnesium with concomitant decreases in Mg(2+) ATPase activity have been identified in children with ADHD.133–136 Magnesium is required for more than 350 different biochemical metabolism pathways in the human body, including oxidation/reduction and ionic regulation.131
Vitamin B6 is essential to the synthesis of many neurotransmitters, particularly dopamine, noradrenaline GABA, etc (see Figure 6.1).131
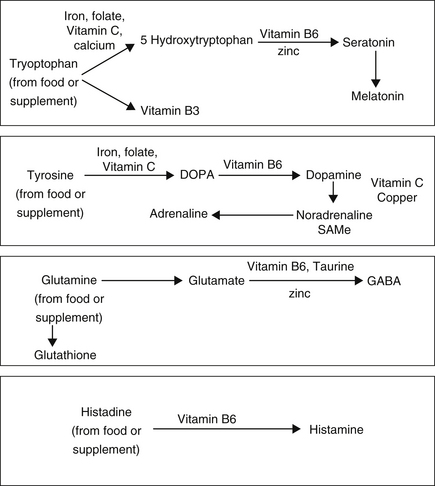
Figure 6.1 Central Nervous system biochemical pathways and cofactors required for neurotransmitter and hormone production132
Several European trials have demonstrated an improvement in the symptoms of ADHD with a combination of magnesium and vitamin B6. Children prescribed a magnesium/B6 regimen (6mg/kg/day Mg, 0.6mg/kg/day B6) for at least 8 weeks displayed a significant reduction in their symptoms of hyperactivity and aggressiveness whilst their attention at school was improved. When the supplementation was ceased, clinical symptoms of the disease reappeared within a few weeks, as did their original lower red blood cell Mg concentrations.137
After 1 month of supplementation of magnesium and B6, magnesium homeostasis was again normalised and there were noticeable improvements in behaviour and attention whilst levels of anxiety and aggression were reduced. Thus, it has been postulated that the determination of plasma and red blood cell Mg can be used to detect deficits and monitor the efficiency of treatment.135, 136
An earlier study found that even though 32 out of 50 children with ADHD demonstrated low red blood cell Mg levels, all patients showed an improvement in symptoms (hyperexcitability, physical aggressiveness, instability, attention, hypertony, spasm, myoclony) after 1–6 months of treatment with magnesium.133 Similarly, children with ADHD receiving 200mg/day magnesium showed a significant decrease in hyperactivity compared to a non-supplemented control group.138
Iron
Iron is necessary to ensure oxygenation, produce energy in the cerebral parenchyma (via cytochrome oxidase) and for the synthesis of both neurotransmitters and myelin. Iron concentrations in the umbilical artery are critical for the development of the fetus and are specific to the IQ/cognition of the child, playing a major role in both brain structure and function.131, 132
Furthermore, the lower the serum ferritin levels, the more severe the general ADHD (hyperactivity) symptoms.139 Available data is conflicting as to the relationship of low serum ferritin specifically to cognitive deficits.140, 141
As stated previously, there is a documented significant comorbidity between ADHD and RLS. Iron is a cofactor in dopamine production and patients with restless legs have lower levels of dopamine in their substantia nigra.142 Thus iron deficiency may, indeed, be one of the underlying common pathophysiological mechanisms in individuals with both ADHD and RLS. Thus, it is suggested that physicians assess children with ADHD for RLS, a family history of RLS and iron deficiency.139
A recent trial of iron supplementation (ferrous sulfate 170mg/day) resulted in an improvement of ADHD symptoms in those children with low serum ferritin levels. Iron therapy was well tolerated with effectiveness comparable to stimulant medication.143 However, an earlier Cochrane study has demonstrated that there is no clear evidence that iron treatment in children less than 3 years of age with iron deficiency anaemia will improve psychomotor development after 5–11 days of treatment.144 There is a need for future investigations with larger controlled trials.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


