FIGURE 9-1 A 12-lead electrocardiogram showing sinus rhythm with evidence of ventricular preexcitation. The delta wave is negative in lead V1 (arrow) and the transition (asterisk) in the precordial leads occurs between leads V3 and V4, compatible with a right free wall accessory pathway.
FIGURE 9-2 Induction of orthodromic atrioventricular reciprocating tachycardia (ORT) with programmed atrial stimulation. After a drive train at 400 ms (S1), a single atrial extrastimulus (S2) is introduced at 210 ms. The extrastimulus blocks in the accessory pathway and conducts over the specialized conduction system, yielding supraventricular tachycardia. The mechanism of a tachycardia whose induction depends upon conduction block in the accessory pathway is very likely to be ORT. Abl = ablation; CS = coronary sinus; H His; RV = right ventricle.
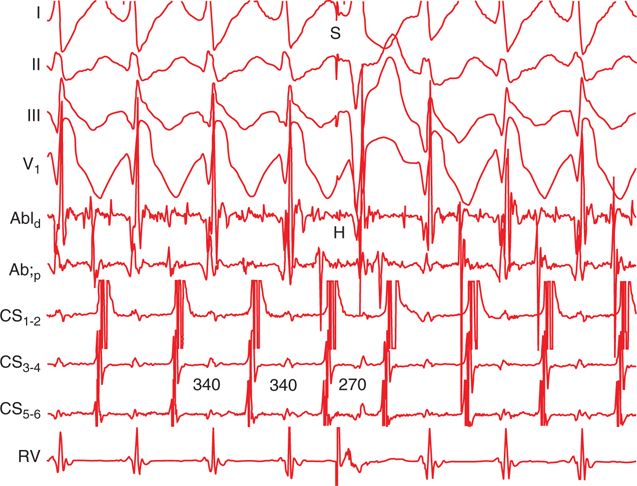
FIGURE 9-3 Response to a His-synchronous premature ventricular complex (“S”) during supraventricular tachycardia. The premature ventricular complex (PVC) results in advancement of the subsequent atrial electrogram (from 340 to 270 ms), which confirms the presence of an accessory pathway.
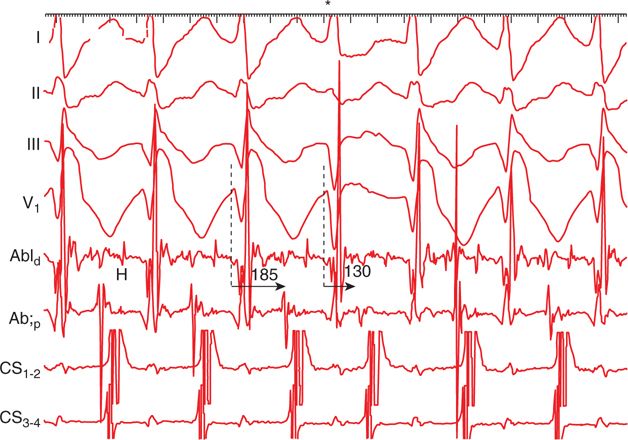
FIGURE 9-4 The ventriculoatrial (VA) time during supraventricular tachycardia with a right bundle branch block pattern is 185 ms, as compared with 130 ms during the narrow QRS complex (asterisk). This observation proves that the mechanism of the tachycardia is orthodromic reciprocating tachycardia (ORT) utilizing a right free wall accessory pathway. (Although the QRS morphology during tachycardia was that of a right bundle branch block pattern, there were several instances in which a narrow QRS complex appeared spontaneously. The narrow QRS complex was always followed by a shorter VA time.)
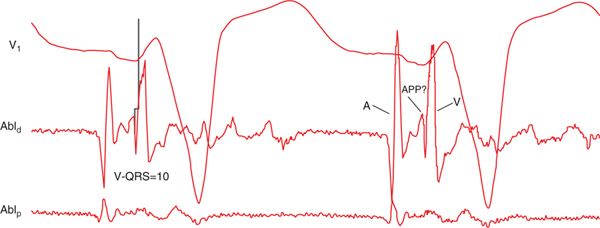
FIGURE 9-5 Prior to radiofrequency ablation, ORT was induced to ensure that a His potential was not present at target site, which had afforded the earliest ventricular activation during sinus rhythm. Note the possible accessory pathway potential (APP) between the ventricular and atrial electrograms.
FIGURE 9-6 Bipolar electrogram during sinus rhythm, recorded by the ablation (Abl) catheter at the site where radiofrequency energy eliminated conduction over the accessory pathway. The activation time (V-QRS) is relatively modest, but there may also be an accessory pathway potential (APP) present.
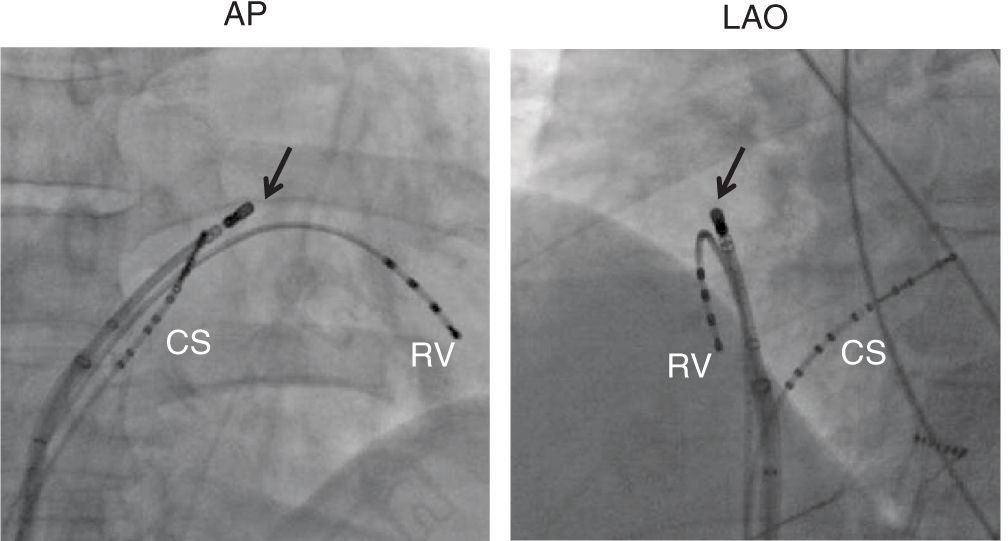
FIGURE 9-7 Fluoroscopic view showing the position of the ablation catheter (arrow) at the site on the tricuspid annulus where radiofrequency ablation eliminated preexcitation. AP = posterior; LAO = left anterior oblique.
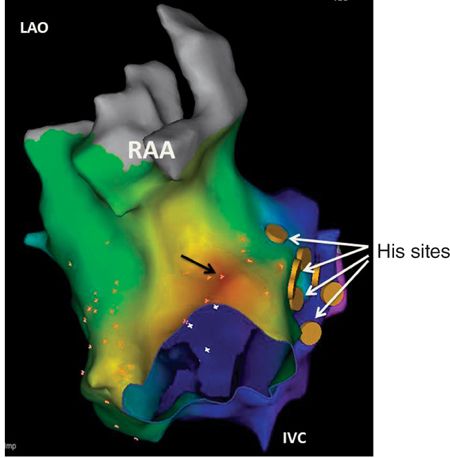
FIGURE 9-8 Activation map of the right atrium (RA) showing that the earliest ventricular activation (arrow) was found at the anterior tricuspid annulus (12 o’clock). A His potential could be recorded relatively diffusely over the septal region. IVC inferior vena cava; RAA = right atrial appendage.
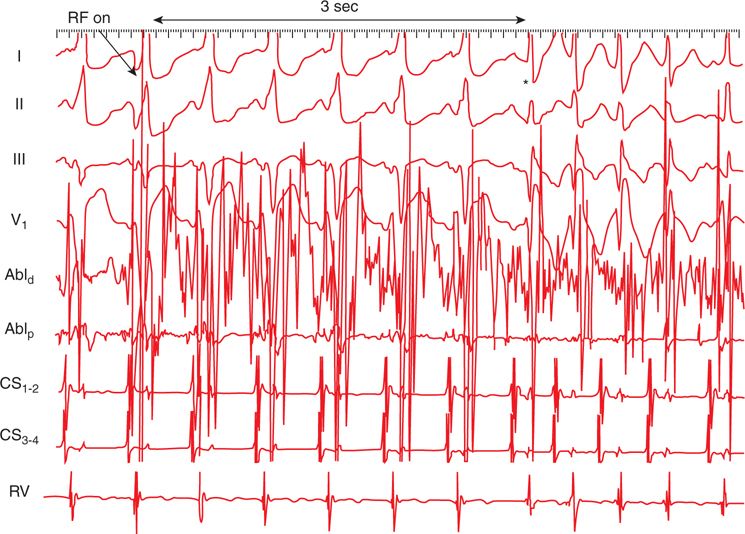
FIGURE 9-9 Initiation of radiofrequency (RF) energy at the anterior tricuspid annulus readily eliminates preexcitation (asterisk). There was no longer evidence of retrograde activation over the pathway or tachycardia.
EPIDEMIOLOGY
AVRT is the most common sustained arrhythmia in patients with WPW syndrome. It is the second most common arrhythmia mechanism in patients presenting for catheter ablation of paroxysmal SVT. In patients undergoing catheter ablation of AVRT/WPW syndrome, right free wall APs account for about 15% of cases. Left free wall and septal accessory pathways are found in about 60% and 25% of patients, respectively. The prevalence of the WPW pattern, that is, evidence of ventricular preexcitation without arrhythmic symptoms, is estimated to be about 2 to 4 per 1000 individuals.1
ETIOLOGY AND PATHOPHYSIOLOGY
Ventricular preexcitation is mediated by anomalous muscular tracts that connect the atrium and ventricle along the mitral or tricuspid annulus. Patients with WPW syndrome are usually otherwise healthy, and no significant abnormalities are found on cardiovascular testing. Occasionally, AVRT may occur in the context of overt heart disease, such as Ebstein anomaly or hypertrophic cardiomyopathy.
Orthodromic AVRT (or ORT) is due to a macroreentrant circuit that involves anterograde activation of the specialized conduction system and retrograde activation over the AP. During ORT, typically a narrow complex tachycardia is inscribed on the 12-lead ECG, with retrograde P waves obscured by the ST segment. In cases of a slowly conducting AP, retrograde conduction may be delayed such that the P wave is found after the T wave, resulting in a long RP tachycardia. Classically, such pathways insert near the posteroseptal area, resulting in negative P waves in the inferior leads. These slowly conducting pathways may result in frequent or nearly incessant bouts of tachycardia, ie, permanent junctional reciprocating tachycardia (PJRT). Frequent tachycardia may be associated with left ventricular dysfunction, which resolves after elimination of the AP.
Much less commonly, one may encounter antidromic AVRT or ART during which the circus movement involves anterograde conduction along the AP and retrograde conduction over the normal conduction system or another AP. The ECG in this case shows a wide QRS-complex tachycardia, the morphology of which does not resemble a typical bundle branch block pattern. The QRS complex during ART is maximally preexcited and may be mistaken for ventricular tachycardia.
One may encounter less common forms of AVRT mediated by APs that do not insert along the AV ring. These include atriofascicular, nodofascicular, and nodoventricular pathways. Conduction along these pathways is decremental and may not be apparent on the resting ECG. Atriofascicular pathways connect the atrium to the right bundle branch and are incapable of retrograde conduction. Nodofascicular or nodoventricular pathways connect the AV node and proximal right bundle or the right ventricular myocardium, respectively. Fasciculoventricular APs connect the distal right bundle branch to the ventricular myocardium. As such, the ECG shows only subtle preexcitation in patients with a fasciculoventricular pathway. These pathways are thought not to participate in AVRT but may act as bystanders during supraventricular tachycardia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree