Atopic Dermatitis
KEY CONCEPTS
![]() Atopic dermatitis is a chronic skin disorder involving inflammation associated with intense pruritus, a hallmark symptom. Management of atopic dermatitis must always include appropriate management of the associated pruritus.
Atopic dermatitis is a chronic skin disorder involving inflammation associated with intense pruritus, a hallmark symptom. Management of atopic dermatitis must always include appropriate management of the associated pruritus.
![]() Atopic dermatitis is associated with other atopic diseases such as asthma and allergic rhinitis in the same patient or family. The three conditions are known as the atopic triad.
Atopic dermatitis is associated with other atopic diseases such as asthma and allergic rhinitis in the same patient or family. The three conditions are known as the atopic triad.
![]() The prevalence of atopic dermatitis appears to have increased two- to threefold in many developed and developing countries during the last three decades. Recent data indicate age and country or regional differences, with some countries showing no change or even a decrease. Rural areas appear to have lower prevalence rates.
The prevalence of atopic dermatitis appears to have increased two- to threefold in many developed and developing countries during the last three decades. Recent data indicate age and country or regional differences, with some countries showing no change or even a decrease. Rural areas appear to have lower prevalence rates.
![]() There are genetic and environmental factors in the pathogenesis and pathophysiologic manifestations of atopic dermatitis. The inheritance pattern is not straightforward. More than one gene may be involved in the disease, with the filaggrin gene (FLG) being a key player.
There are genetic and environmental factors in the pathogenesis and pathophysiologic manifestations of atopic dermatitis. The inheritance pattern is not straightforward. More than one gene may be involved in the disease, with the filaggrin gene (FLG) being a key player.
![]() Atopic dermatitis often presents in infants and young children. The clinical presentation differs somewhat depending on the age of the patient.
Atopic dermatitis often presents in infants and young children. The clinical presentation differs somewhat depending on the age of the patient.
![]() Secondary bacterial skin infections are common in patients with atopic dermatitis and must be promptly treated.
Secondary bacterial skin infections are common in patients with atopic dermatitis and must be promptly treated.
![]() Management of atopic dermatitis must always include appropriate nonpharmacologic management of any controllable environmental factors, such as avoidance of identified triggers. These may include aeroallergens (e.g., mold, grass, pollen), foods (e.g., peanuts, eggs, tomatoes), chemicals (e.g., detergents, soaps), clothing material (e.g., wool, polyester), temperature (e.g., excessive heat), and humidity (e.g., low humidity).
Management of atopic dermatitis must always include appropriate nonpharmacologic management of any controllable environmental factors, such as avoidance of identified triggers. These may include aeroallergens (e.g., mold, grass, pollen), foods (e.g., peanuts, eggs, tomatoes), chemicals (e.g., detergents, soaps), clothing material (e.g., wool, polyester), temperature (e.g., excessive heat), and humidity (e.g., low humidity).
![]() Nonpharmacologic management of atopic dermatitis entails managing the symptoms associated with pruritus and encouraging appropriate skin care habits such as proper bathing techniques and the copious use of moisturizers, which is a standard of care.
Nonpharmacologic management of atopic dermatitis entails managing the symptoms associated with pruritus and encouraging appropriate skin care habits such as proper bathing techniques and the copious use of moisturizers, which is a standard of care.
![]() Topical corticosteroids are the drugs of first choice for atopic dermatitis.
Topical corticosteroids are the drugs of first choice for atopic dermatitis.
![]() Topical calcineurin inhibitors (tacrolimus and pimecrolimus) are alternate treatment options for adults and children over the age of 2 years.
Topical calcineurin inhibitors (tacrolimus and pimecrolimus) are alternate treatment options for adults and children over the age of 2 years.
![]() This chronic illness has substantial socioeconomic impact. The cost may be magnified by undertreatment.
This chronic illness has substantial socioeconomic impact. The cost may be magnified by undertreatment.
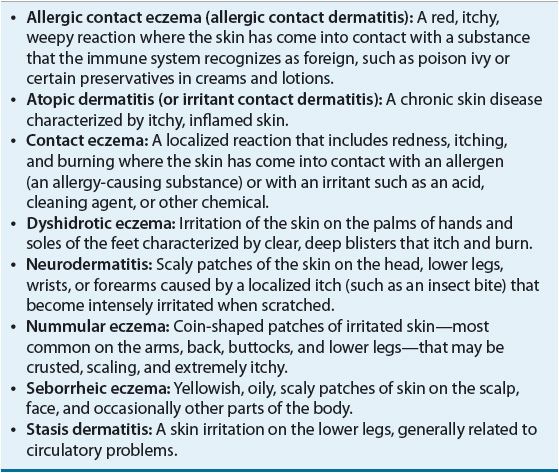
![]() Atopic dermatitis (AD) is a common skin disease. It is often referred to as eczema, which is a general term for several types of skin inflammation. AD is the most common type of eczema (Table 79–1).1 It is a chronic skin disorder involving inflammation with pruritus as the hallmark symptom and presentation. This disorder is often the prelude to atopic diathesis, which includes asthma and other allergic diseases.
Atopic dermatitis (AD) is a common skin disease. It is often referred to as eczema, which is a general term for several types of skin inflammation. AD is the most common type of eczema (Table 79–1).1 It is a chronic skin disorder involving inflammation with pruritus as the hallmark symptom and presentation. This disorder is often the prelude to atopic diathesis, which includes asthma and other allergic diseases.
![]() This form of dermatitis is commonly associated with other atopic disorders, such as allergic rhinitis and asthma. AD, allergic rhinoconjunctivitis, and asthma are known collectively as the atopic triad.2 AD has also been defined as the cutaneous manifestation of atopy.2
This form of dermatitis is commonly associated with other atopic disorders, such as allergic rhinitis and asthma. AD, allergic rhinoconjunctivitis, and asthma are known collectively as the atopic triad.2 AD has also been defined as the cutaneous manifestation of atopy.2
The disease can have periods of exacerbation, or flareups, followed by periods of remission. These flareups may be disruptive to the patient’s quality of life and may affect the entire family. Disease flareups are difficult to manage and may be complicated by secondary infections. About one-half (estimate up to 65%) of cases in children first manifest before age 1 year1–4; these cases are termed early onset atopic dermatitis.5 Approximately 85% of patients develop symptoms before age 5 years.1
Of the children with AD diagnosed before age 1 year, approximately 40% to 60% will have the same skin condition continuing into their adulthood.1,3
Onset after age 30 years is much less common and is often caused by exposure to harsh or wet conditions1 such as repeated skin trauma or exposure to harsh chemicals. In adults, the prevalence is believed to be 1% to 3%, with an overall lifetime prevalence of approximately 7%.1
EPIDEMIOLOGY
![]() The prevalence of AD is generally said to have increased two- to threefold in developed and developing countries during the last three decades.5 Currently in developed countries, an estimated 15% to 30% of children and 2% to 10% of adults are affected.5,6 The prevalence appears to be increasing worldwide, as earlier prevalence rates were estimated at 10% to 15% in children.4
The prevalence of AD is generally said to have increased two- to threefold in developed and developing countries during the last three decades.5 Currently in developed countries, an estimated 15% to 30% of children and 2% to 10% of adults are affected.5,6 The prevalence appears to be increasing worldwide, as earlier prevalence rates were estimated at 10% to 15% in children.4
![]() The largest international study of the prevalence of AD found both age and country differences in prevalence rates.7 This international study was the International Study of Asthma and Allergies in Childhood (ISAAC), which was conducted in three phases.8 ISAAC Phase One included 700,000 children from 156 centers in 56 countries between 1992 and 1998. ISAAC Phase Two studied allergic causes from 30 centers in 22 countries. ISAAC Phase Three repeated a multicountry cross-sectional survey (1999 to 2004) and included 187,943 children aged 6 to 7 years from 64 centers in 35 countries and 302,159 adolescents aged 13 to 14 years from 105 centers in 55 countries. For children aged 6 to 7 years, most countries showed an increase of 2 standard deviations (SDs) in mean annual prevalence over a 5- to 10-year period. In contrast, for adolescents aged 13 to 14 years, the trends differ from country to country. Large increases in prevalence were seen in developing countries (e.g., Mexico, Chile, Kenya, and Algeria, and seven countries in Southeast Asia). But in other countries with formerly very high prevalences, the mean annual prevalence in eczema symptoms has either leveled off or decreased. Most of the largest decreases (SD ≥2) in prevalence were reported from developed countries in northwest Europe, (e.g., the United Kingdom, Ireland, Sweden, Germany) and New Zealand.7 The ISAAC study has suggested that a maximum prevalence plateau of approximately 20% has emerged.7,8
The largest international study of the prevalence of AD found both age and country differences in prevalence rates.7 This international study was the International Study of Asthma and Allergies in Childhood (ISAAC), which was conducted in three phases.8 ISAAC Phase One included 700,000 children from 156 centers in 56 countries between 1992 and 1998. ISAAC Phase Two studied allergic causes from 30 centers in 22 countries. ISAAC Phase Three repeated a multicountry cross-sectional survey (1999 to 2004) and included 187,943 children aged 6 to 7 years from 64 centers in 35 countries and 302,159 adolescents aged 13 to 14 years from 105 centers in 55 countries. For children aged 6 to 7 years, most countries showed an increase of 2 standard deviations (SDs) in mean annual prevalence over a 5- to 10-year period. In contrast, for adolescents aged 13 to 14 years, the trends differ from country to country. Large increases in prevalence were seen in developing countries (e.g., Mexico, Chile, Kenya, and Algeria, and seven countries in Southeast Asia). But in other countries with formerly very high prevalences, the mean annual prevalence in eczema symptoms has either leveled off or decreased. Most of the largest decreases (SD ≥2) in prevalence were reported from developed countries in northwest Europe, (e.g., the United Kingdom, Ireland, Sweden, Germany) and New Zealand.7 The ISAAC study has suggested that a maximum prevalence plateau of approximately 20% has emerged.7,8
There were no differences according to the sex of the study participant, or with gross national income at a country level.7 This is consistent with other reports that AD affects males and females at approximately the same rate.1 There appears to be a lower prevalence of AD in rural areas when compared with urban areas, suggesting a link to the hygiene hypothesis, which postulates that the absence of early childhood exposure to infectious agents increases susceptibility to allergic diseases.9–11 In contrast, children attending daycare centers before 3 months of age have less atopy and asthma in later childhood,11,12 and areas with diffuse and chronic helminth infestations have a low prevalence of allergic diseases.11 In addition, a recent European birth cohort study involving 1,133 newborns showed that children born to farm families had a lower prevalence of sensitization to seasonal inhaled allergens such as grass pollen.13 Maternal exposure during pregnancy (i.e., prenatal exposure) to animal sheds correlated with the lower prevalence rate in the farm children.12 However, there were no differences in prevalence related to inhaled perennial allergens.
Reported risk factors associated with higher prevalence include urban environment, higher socioeconomic status, higher level of family education, a family history of AD, female gender (after age 6 years), and smaller family size.8
ETIOLOGY
![]() AD is a complex genetic disease that arises from gene–gene and gene–environment interactions. There are two major groups of genes involved. First, there are the genes encoding for epidermal or other epithelial structural proteins. Second, there are genes encoding for the major elements of the immune system.5
AD is a complex genetic disease that arises from gene–gene and gene–environment interactions. There are two major groups of genes involved. First, there are the genes encoding for epidermal or other epithelial structural proteins. Second, there are genes encoding for the major elements of the immune system.5
The inheritance pattern is not straightforward. More than one gene is likely involved in the disease. There is an increased risk for a child to have AD if there is a family history of other atopic diseases, such as hay fever or asthma. The risk is significantly higher if both parents have an atopic disease.1 Studies of identical twins show that a person whose identical twin has AD is seven times more likely to have AD than someone in the general population.1 And a person whose fraternal twin has AD is three times more likely to have AD than someone in the general population.1 Another estimate is 80% concordance in monozygous twins and 20% in heterozygous twins.10
Thus, genetic predispositions to developing AD exist. Specifically, there are several possible genes on the chromosomes 3q21, 1q21, 16q, 17q25, 20p, and 3p26. Of these chromosomes, 1q21 has the highest linkage region. This region has a family of epithelium-related genes called the epidermal differentiation complex.5 One of these genes, the filaggrin gene (FLG), on chromosome 1q21.3, was initially identified as the gene involved in ichthyosis vulgaris, and several mutations of this gene were subsequently identified in European and Japanese patients with AD.14 FLG encodes for a key protein in epidermal differentiation. Mutations or deficiency of FLG results in an abnormality in permeability barrier function.15
Epidermal barrier dysfunction is a prerequisite for the penetration of high-molecular-weight allergens in pollens, house dust mite products, microbes, and food.5 In mice studies, this barrier abnormality alters thresholds for irritant and acute allergic contact dermatitis, and FLG deficiency predisposes to the development of an AD-like dermatosis.15 In humans, two common FLG variants (R501X and 2282de14) with an estimated combined allele frequency of about 6% have been identified in individuals of European descent.16 Eighteen other less common variants have also been identified in Europeans, with an additional 17 mutations restricted to individuals of Asian descent.16 Each of these variants leads to nonsense mutations which either prevent or severely diminish the production of filaggrin in the epidermis.16 Mutations of FLG seem to occur mainly in early onset AD patients and may be associated with the development of asthma in patients with AD.5,16 However, FLG mutations are identified in only 30% of European patients with AD; implying that other genetic mutations affecting other epidermal structures may be important (e.g., changes in the cornified envelope proteins involucrin and loricrin, or lipid composition).5
There are other genes encoding for the immune system that may be associated with AD, especially those found on chromosome 5q31-33.5 These genes code for cytokines that regulate IgE synthesis. Cytokines are produced mainly by type 1 and type 2 helper T cells. T-helper type 1 (TH1) cells produce cytokines, which suppress immunoglobulin E (IgE) production (e.g., interferon-γ and interleukin-12 [IL-12]).5 T-helper type 2 (TH2) cells produce cytokines, which increase IgE production (e.g., IL-5 and IL-13).5,17 In patients with AD, there is an imbalance between TH1 and TH2 immune responses. These patients are genetically predisposed to TH2 predominance, seen as increased TH2 cell activity.2,5,17 Increased TH2 activity causes the release of IL-3, IL-4, IL-5, IL-10, and IL-13, resulting in blood eosinophilia, increased serum IgE, and increased growth and development of mast cells.2,5,17,18 In addition, these cytokines affect the maturation of B cells and cause a genomic rearrangement in these cells that favors isotype class switching from immunoglobulin M (IgM) to IgE.5
In summary, recent data suggest that FLG deficiency alone can provoke a barrier abnormality in the epidermis and predispose to the development of dermatitis by enhancing allergen absorption through the skin.19 Furthermore, there appears to be complex relationships, including genetic and nongenetic risk factors, that modify an individual’s susceptibility to allergic disease.20 Complex genetic factors contribute to the increased susceptibility to AD (FLG mutations and gene–gene interactions). These, along with environmental factors (gene–environment interactions), result in the pathophysiologic changes and clinical presentations associated with AD.
PATHOPHYSIOLOGY
The initial mechanisms that trigger inflammatory changes in the skin in patients with AD are unknown. Neuropeptides, irritation, or pruritus-induced scratching may be causing the release of proinflammatory cytokines from keratinocytes. Alternatively, allergens in the epidermal barrier or in food may cause T-cell mediated but IgE-independent reactions. Allergen-specific IgE is not a prerequisite.5 Characteristic features in pathophysiology are skin barrier dysfunction, and immune deviation toward TH2 with subsequent increased IgE.10 The disease is further complicated by microbial colonization with pathologic organisms resulting in increased susceptibility for skin infections.10
Skin barrier dysfunction plays a critical role in the development of AD,10,21,22 and loss of function mutations in the skin structural protein filaggrin is a major risk factor.22 Other factors may include a deficiency of skin barrier proteins, increased peptidase activity, lack of certain protease inhibitors, and lipid abnormalities.22 There must be epidermal barrier dysfunction for high-molecular-weight allergens in pollens, house dust mite particles, microbes, and foods to penetrate the skin barrier. Atopic skin has reduced antimicrobial peptides (AMPs). AMPs are normally produced by keratinocytes, sebocytes, and mast cells, and they form a chemical shield on the surface of the skin. Reduced AMPs result in a diminished antimicrobial barrier, which correlates with increased susceptibility to infections and superinfections seen in these patients.23
On penetration of the epidermal barrier, allergens are met by dendritic cells (DCs). DCs are antigen-presenting cells populating the skin, respiratory tract, and mucosa of the GI tract (i.e., at the front line of pathogen entry).24 DCs then enhance TH2 polarization, resulting in increased production of IgE. Keratinocytes in the skin of patients with AD also produce high levels of an IL-7–like protein, which again drives dendritic cells to enhance TH2 polarization. Epidermal dendritic cells in patients with AD bear IgE and express its high-affinity receptor (FcεRI).25–27 Serum IgE is often elevated in patients with AD,1,18 especially during an exacerbation.
However, on initial presentation, patients with early onset AD generally do not have increased IgE levels (i.e., there is no detectable IgE-mediated allergic sensitization). IgE-mediated allergic sensitization may occur several weeks or months after the initial AD lesions appear. Although in some children—mostly girls—this sensitization never occurs.5
Predisposing Factors
Several factors can predispose patients to development of AD. These include climate, infection, genetics, environmental aeroallergens, and food.
Hot and extremely cold climates are both poorly tolerated by patients with this condition. Dry weather, common in the winter, causes increased skin dryness. Hot weather causes increased sweating, resulting in pruritus.
Patients with AD are commonly colonized by Staphylococcus aureus bacteria. Clinical infections with S. aureus frequently cause flareups of AD.
As discussed previously, genetics plays a role in AD. Family history of AD is common.
Exposure to environmental aeroallergens is another risk factor. Dust mites, pollens, molds, cigarette smoke, and dander from animal hair or skin may worsen the symptoms of AD.1,18
The role of food as antigens in the pathogenesis of AD is controversial. Small amounts of environmental foods (low-dose exposure from foods on tabletops, hands, dust) may penetrate the skin barrier and be taken up by Langerhans cells, leading to TH2 responses and IgE production.28 However, early high-dose oral food consumption induces oral tolerance. The timing and balance of cutaneous and oral exposure determines whether a child will have allergy or tolerance.28 Increased serum IgE antibodies to a particular food is evidence of sensitization to a food and is consistent with although not proof of a food allergy.1,29 Eczema may frequently be a manifestation of food allergy,28 and patients with AD have a higher prevalence of food allergy than those in the general population.1 Conversely, a current belief is that food allergy may be caused by AD, and in most patients with coexisting AD and food allergy, AD precedes the food allergy. Regardless, the two conditions coexist, and the likelihood of an infant or child with AD also having food allergy or allergies must be kept in mind.29
There is a known epidermal barrier dysfunction in AD, allowing for increased low-level skin permeability to allergenic foods. Certain foods may trigger acute reactions, including urticaria and anaphylaxis. The most commonly reported allergenic foods are eggs, milk, peanuts, wheat, soy, tree nuts, shellfish, and fish.1 Individual food allergies, such as peanut allergy, have increased in prevalence in the last decade;28,29 new food allergies may also be increasing in prevalence, particularly kiwi allergy28,30 and sesame seed allergy.28,31 Consistent with the oral tolerance concept, early results from recent studies using sublingual and oral immunotherapy to specific food allergens (e.g., milk or peanut) appear to indicate that it may be possible to induce oral tolerance, and that it may be possible to desensitize children to some allergenic foods. Currently, these treatment protocols have only been done in highly supervised research settings and with small numbers of patients.32 For more information about management of food allergies the reader is directed to the 2010 National Institute of Allergy and Infectious Diseases (NIAID)-sponsored expert panel’s report, available at www.niaid.nih.gov.29
CLINICAL PRESENTATION
Diagnosis of AD is generally based on clinical presentation (Table 79–2).1 There is no objective diagnostic test for the clinical confirmation of AD.1,33 Filaggrin gene mutations may be associated with persistent and more severe AD as well as early onset cases.22
TABLE 79-2 Skin Features Associated with Atopic Dermatitis1
Clinical Controversy…
![]() The course of AD varies significantly over time. Studies reviewing the natural course of the disease usually describe the disease pattern as persistent, intermittent, or in remission.8 A 2004 study found that 43% were in complete remission after age 2 years, with 19% having persistent disease and 38% an intermittent pattern.8
The course of AD varies significantly over time. Studies reviewing the natural course of the disease usually describe the disease pattern as persistent, intermittent, or in remission.8 A 2004 study found that 43% were in complete remission after age 2 years, with 19% having persistent disease and 38% an intermittent pattern.8
The clinical presentation of AD differs depending on the age of the patient. In infancy, the earliest onset of AD usually occurs between 2 and 6 months of age, and especially between the 6th and 12th weeks of life.1,2 It has been reported that 75% of cases have their onset within the first 6 months.2 A more conservative estimate is that at least 65% of patients develop symptoms within the first year of life, and at least 85% will have developed symptoms before the age of 5 years.1 The initial presentation in infancy is an erythematous, papular skin rash that may first appear on the cheeks and chin as a patchy facial rash1,2 and that can progress to red, scaling, oozing skin.1 The rash shows a centrifugal distribution affecting the malar region of the cheeks, forehead, scalp, chin, and behind the ears while sparing the central areas (i.e., the nose and paranasal creases).2 Lesions occur in the flexor surfaces, such as antecubital and popliteal fossae. Over the next few weeks and as the infant becomes more mobile and begins crawling, the lesions spread to the extensors of the lower legs, and eventually the entire body may be involved, with sparing of the diaper area and the nose.1 These lesions are associated with uncontrollable itchiness, and the infant will become irritable and may try to rub his or her face to relieve the itch. Scratching may occur quite early, and infants with AD may scratch themselves continuously, mainly when they are undressed or during sleep.2 Excessive rubbing or scratching may result in excoriation and development of secondary infections.
In childhood, the skin often appears dry, flaky, rough, cracked, and may bleed because of scratching. With repeated scratching and rubbing the skin becomes lichenified. Lichenification, usually localized to the flexural folds of the extremities,33 is characteristic of childhood AD in older children and adults.33,34 Lichenification signifies repeated rubbing of the skin and is seen mostly over the folds, bony protuberances, and forehead.34 Excoriations and crusting are also commonly seen, along with secondary infections. Sometimes increased folds are seen underneath the eyes (so-called Dennie–Morgan folds).34 Lesions are still most commonly seen in the flexor surfaces of the body, particularly the flexural creases of the antecubital and popliteal fossae.34
Sleep disturbances also occur. One study reported that there are both brief and longer awakenings associated with scratching episodes that affect sleep efficiency in school-age children with AD.35
In adulthood, lesions are more diffuse with underlying erythema. The face is commonly involved and may be dry and scaly. Lichenification may again be seen. A brown macular ring around the neck, representing a localized deposit of amyloid, is typical but not always present.34
Although no objective diagnostic test confirms presence of AD,1 some signs, symptoms, and other factors are commonly used in its diagnosis. These include pruritus, early age of onset, eczematous skin lesions that vary with age, chronic and relapsing courses, dry and flaky skin, IgE reactivity, family or personal history of asthma or hay fever, or other atopic diseases (Table 79–3).18 In addition, allergy skin testing may be helpful in identifying factors that trigger flares of AD.1 Negative results may help rule out certain substances as triggers; however, positive results may be unrelated to disease activity, and false positives are common.1
< div class='tao-gold-member'>