25 Asthma
Asthma means ‘laboured breathing’ in Greek and was first described 3000 years ago. It is a broad term used to refer to a disorder of the respiratory system that leads to episodic difficulty in breathing. The national UK guidelines (BTS/SIGN, 2009) define asthma as ‘a chronic inflammatory disorder of the airways which occurs in susceptible individuals; inflammatory symptoms are usually associated with widespread but variable airflow obstruction and an increase in airway response to a variety of stimuli. Obstruction is often reversible either spontaneously or with treatment’.
Epidemiology
The exact prevalence of asthma remains uncertain because of the differing ways in which airway restriction is reported, diagnostic uncertainty (especially for children under 2 years) and the overlap with other conditions such as chronic obstructive pulmonary disease (COPD). Over 5 million people in the UK have asthma (Asthma UK, 2001) and around 300 million worldwide. Mortality from asthma is estimated at approximately 0.4 per 100,000 with around 1400 deaths per annum in the UK. Most deaths occur outside hospital; the most common reasons for death are thought to be inadequate assessment of the severity of airway obstruction by the patient and/or clinician and inadequate therapy with inhaled or oral steroids.
Aetiology
The two main causes of asthma symptoms are airway hyperresponsiveness and bronchoconstriction. Hyperresponsiveness is an increased tendency of the airway to react to stimuli or triggers to cause an asthma attack. Bronchoconstriction is a narrowing of the airways that causes airflow obstruction. Possible triggers are listed in Table 25.1. One of the most common trigger factors is the allergen found in the faeces of the house dust mite, which is almost universally present in bedding, carpets and soft furnishing. Pollen from grass (prevalent in June and July) can lead to seasonal asthma. The role of occupation in the development of asthma has become apparent with increased industrialisation. There are many causes of occupational asthma, and bronchial reactivity may persist for years after exposure to the trigger factor. Drug-induced asthma can be severe and the most common causes are β-blocker drugs and prostaglandin synthetase inhibitors. The administration of β-adrenoceptor blockers to a patient, even in the form of eye drops, can cause β2-receptor blockade and consequent bronchoconstriction. Selective β-adrenoceptor blockers are thought to pose slightly less risk, but as these lose their selectivity at higher doses, it is generally recommended that this group of drugs is avoided altogether in asthma patients. Aspirin and related non-steroidal anti-inflammatory drugs can cause severe bronchoconstriction in susceptible individuals. Aspirin inhibits the enzyme cyclo-oxygenase, which normally converts arachidonic acid to (bronchodilatory) prostaglandins. When this pathway is blocked, an alternative reaction predominates, leading to an increase in production of bronchoconstrictor (cys-) leukotrienes. Figures from differing studies vary, but between 2% and 20% of the adult asthma population are thought to be sensitive to aspirin.
Table 25.1 Examples of asthma triggers
| Trigger | Examples |
| Allergens | Pollens, moulds, house dust mite, animals (dander, saliva and urine) |
| Industrial chemicals | Manufacture of, for example, isocyanate-containing paints, epoxy resins, aluminium, hair sprays, penicillins and cimetidine |
| Drugs | Aspirin, ibuprofen and other prostaglandin synthetase inhibitors, β-adrenoceptor blockers |
| Foods | A rare cause but examples include nuts, fish, seafood, dairy products, food colouring, especially tartrazine, benzoic acid and sodium metabisulfite |
| Environmental pollutants | Traffic fumes. cigarette smoke, sulphur dioxide |
| Other industrial triggers | Wood or grain dust, colophony in solder, cotton, dust, grain weevils and mites |
| Miscellaneous | Cold air, exercise, hyperventilation, viral respiratory tract infections, emotion or stress, swimming pool chlorine |
Pathophysiology
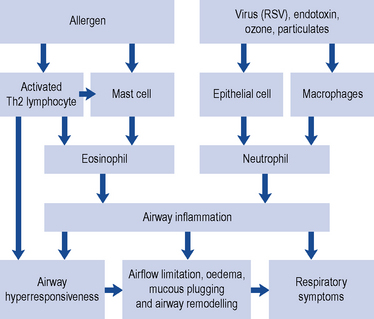
Asthma can be classified according to the underlying pattern of airway inflammation with the presence or absence of eosinophils in the airways (eosinophilic vs. non-eosinophilic). Traditionally patients are described as having ‘extrinsic asthma’ when an allergen is thought to be the cause of their asthma. This is more common in children with a history of atopy, where triggers, such as dust mite, cause IgE production. Other environmental factors are also important, such as exposure to rhinovirus during the first 3 years of life (Holgate et al., 2010). ‘Intrinsic asthma’ develops in adulthood, with symptoms triggered by non-allergenic factors such as a viral infection, irritants which cause epithelial damage and mucosal inflammation, emotional upset which mediates excess parasympathetic input or exercise which causes water and heat loss from the airways, triggering mediator release from mast cells. In practice, patients often have features of both types of asthma and the classification is unhelpful and oversimplifies the pathogenesis of asthma.
Mucus production is normally a defence mechanism, but in asthma patients, there is an increase in the size of bronchial glands and goblet cells that produce mucus. Mucus transport is dependent on its viscosity. If it is very thick, it plugs the airways, which also become blocked with epithelial and inflammatory cell debris. Mucociliary clearance is also decreased due to inflammation of epithelial cells. The environmental insults causing asthma are also thought to affect the structure and function of the airway epithelium. The exact role of these cytokines, cellular mediators and the interrelationships with each other and with the causative allergenic or non-allergenic mechanisms has, however, yet to be fully determined and may vary over time (Douwes et al., 2002; Holgate et al., 2010). Fig. 25.1 outlines the main cellular mechanisms involved.
Investigations
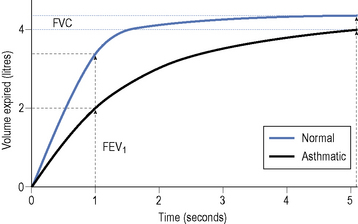
The most useful test for abnormalities in airway function is the forced expiratory volume (FEV). This is measured by means of lung function assessment apparatus such as a spirometer. The patient inhales as deeply as possible and then exhales forcefully and completely into a mouthpiece connected to a spirometer. The FEV1 is a measure of the FEV in the first second of exhalation. The forced vital capacity (FVC) can also be measured, which is an assessment of the maximum volume of air exhaled with maximum effort after maximum inspiration. The FEV1 is usually expressed as a percentage of the total volume of air exhaled, reported as the FEV1/FVC ratio. This ratio is a useful and highly reproducible measure of the capabilities of the lungs. Normal individuals can exhale at least 70% of their total capacity in 1 s. In obstructive lung disorders, such as asthma, the FEV1 is usually decreased, the FVC normal or slightly reduced and the FEV1/FVC ratio decreased, usually <0.7 (Fig. 25.2).
The diagnosis of asthma can be confirmed by measuring the response to a bronchodilator or by examining a patient’s day-to-day variation in PEF readings. A diurnal variability of 60 L/min (or more than 20%) is highly suggestive of asthma (GINA, 2009). However, individuals may not have airflow obstruction at the time of the test, so the absence of an improvement does not rule out asthma. In this situation, peak flow readings can be done at home with repeated pre- and post-bronchodilator readings taken at various times of the day.
Treatment
As asthma involves inflammation and bronchoconstriction, treatment should be directed towards reducing inflammation and increasing bronchodilation. Treatment aims should include a lack of day and nighttime symptoms, no asthma exacerbations, no need for rescue medication, normal PEFs and no unwanted side effects from medication (BTS/SIGN, 2009; GINA, 2009). Anti-inflammatory drugs should be given to all but those with the mildest of symptoms. Other measures, such as avoidance of recognised trigger factors, may also contribute to the control of this disease. The lowest effective dose of drugs should be given to minimise short-term and long-term side effects. It should, however, always be remembered that asthma is a potentially life-threatening illness, is often undertreated and not all patients will achieve optimal control. Common therapeutic and practice problems encountered in the management of asthma are outlined in Box 25.1.
Box 25.1 Management of common practice problems
Chronic asthma
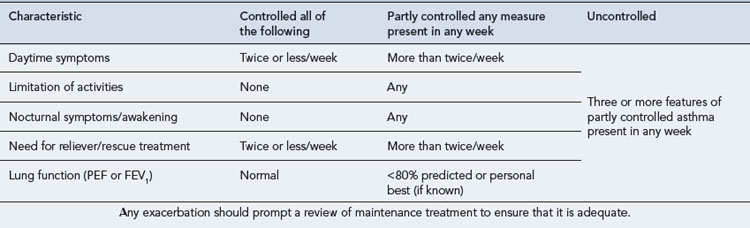
Treatment of chronic asthma should be managed in a stepwise progression. This section concentrates on management in adults, as outlined in Fig. 25.3, but corresponding management steps for children are available (BTS/SIGN, 2009). Therapy is moved up the steps according to the severity of the patient’s asthma symptoms and response to current treatment. When a patient has been stable for at least 3 months (GINA, 2009), therapy should be stepped back down; for example, by halving the inhaled corticosteroid (ICS) dose. International guidelines aim for management to achieve and maintain clinical control, which is defined in Table 25.2. A model for patient review and adjustment of therapy, based on assessment of asthma control, has been suggested (Crompton et al., 2006) and is shown in Fig. 25.4. To help in patient education, the terms used to describe the effects of asthma medication are similar across all manufacturers and sources of education. ‘Reliever’ is used for agents that give immediate relief of symptoms. Agents that act to reduce inflammation or give long-term bronchodilation are referred to as ‘controllers’ or ‘preventers’.
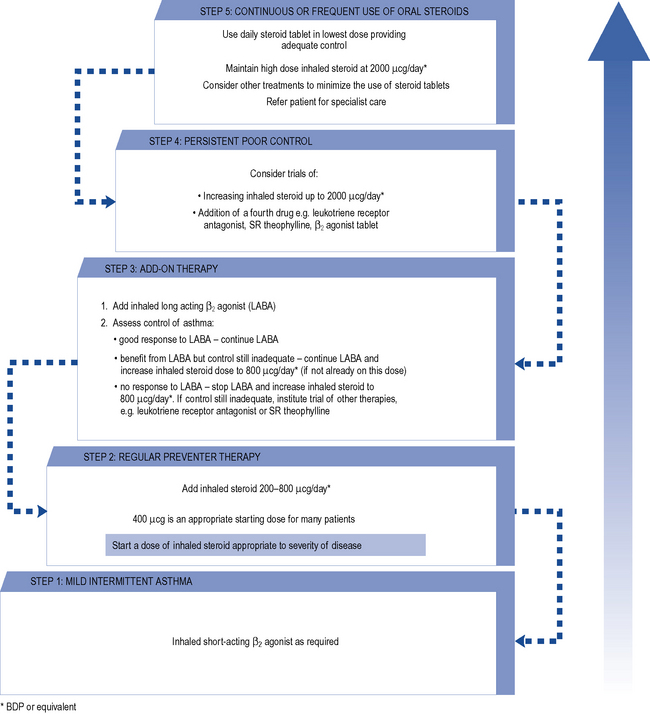
Fig. 25.3 Summary of stepwise management in adults
(reproduced by permission of the BMJ Publishing Group, from BTS/SIGN, 2009).
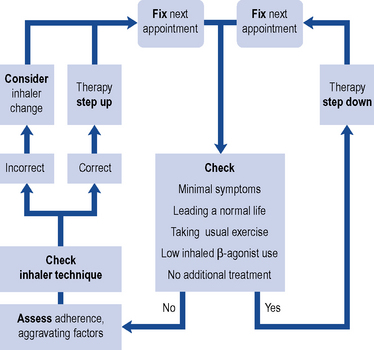
Fig. 25.4 Adjusting therapy to achieve asthma control
(from Crompton et al., 2006 reproduced by permission. Copyright Elsevier publishing).
Reliever medication
Additional bronchodilators
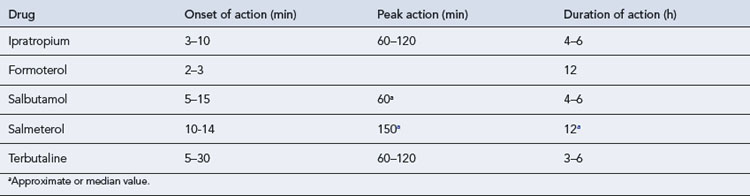
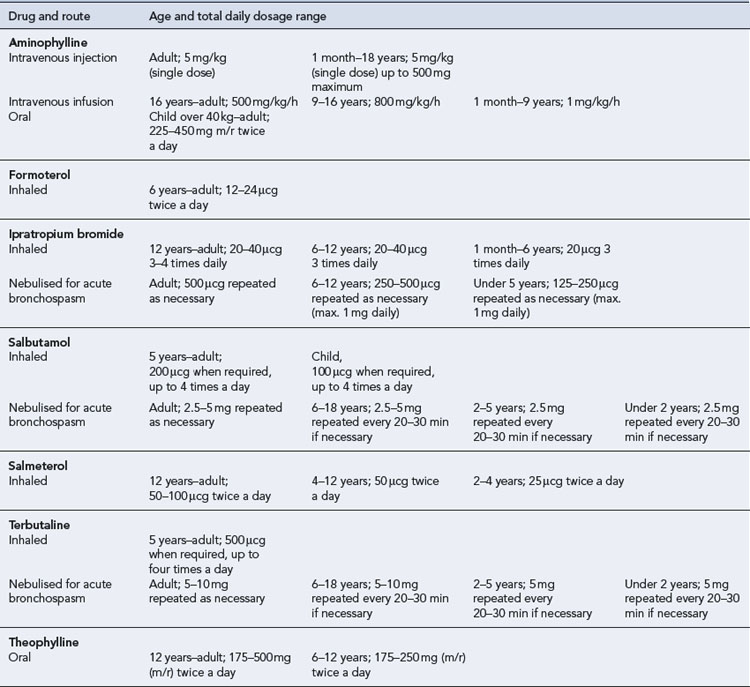
Additional bronchodilators may be required if the above therapy does not adequately control symptoms (Tables 25.3 and 25.4).
Long acting β-adrenoreceptor agonist bronchodilators
Meta-analysis of LABA trials has shown a potential increase in asthma deaths of 1 death in 1000 patient-years of use, but this increased risk is lessened when used alongside ICSs (Saltpeter et al., 2006). Taking this evidence into account, it is advised that LABAs should
A formoterol and budesonide combination inhaler can be given both as maintenance therapy and for symptomatic relief. Current trial evidence shows that this dosing method is an alternative at step 3 for adults who are poorly controlled on SABA and ICS, have experienced one or more severe exacerbations in the previous 12 months, or as an alternative to increasing the ICS dose to above 2 mg/day at step 4 (NPC, 2008).
Oral bronchodilators
Theophylline should be started at a dose of 400–500 mg/day in adults and, if required, increased after 7 days to 800–1000 mg/day. In children, higher doses may be required but this will be determined by the age of the child (see Chapter 10).
Theophylline has a narrow therapeutic index and its hepatic metabolism varies greatly between individuals. Theophylline clearance is affected by a variety of factors, including disease states and concurrent drug therapy. The dose used should, therefore, take into account these factors, which are listed in Table 25.5. Plasma levels may be taken after 3–4 days at the higher dose, and it has been normal practice to adjust the dose to keep the plasma level within a therapeutic window of 10–20 mg/L, although improvements in respiratory function are seen at levels as low as 5 mg/L in some patients. As the bronchodilating effects of theophylline are proportional to the log of the plasma concentrations, there is proportionally less bronchodilation as the plasma level increases. The mild side effects such as nausea and vomiting are seen at concentrations as low as 13 mg/L but are more common over 20 mg/L. Significant cardiac symptoms, tachycardia and persistent vomiting are usually seen at concentrations of 40 mg/L while severe CNS effects, such as seizures, have been seen at 30 mg/L but are more common above 50 mg/L.
Table 25.5 Factors affecting theophylline clearance
| Decreased clearance | Increased clearance |
|---|---|
| Congestive cardiac failure | Cigarette smoking |
| Cor pulmonale | Children 1–12 years |
| Chronic obstructive pulmonary disease | High-protein, low-carbohydrate diet |
| Viral pneumonia | Barbecued meat |
| Acute pulmonary oedema | Carbamazepine |
| Cirrhosis | Phenobarbital |
| Premature and term babies | Phenytoin |
| Elderly | Sulfinpyrazone |
| Obesity | |
| High-carbohydrate, low-protein diet | |
| Cimetidine | |
| Erythromycin | |
| Oral contraceptives | |
| Ciprofloxacin | |
| Propranolol |
Preventer medication
Anti-inflammatory agents
Regular anti-inflammatory treatment should be used for patients who are not controlled on a SABA alone (BTS/SIGN, 2009). Corticosteroids are the most commonly used anti-inflammatory agents (Table 25.6), but others such as the cromones are available.
Table 25.6 Inhaled corticosteroids used for the prophylaxis of asthma
| Total daily dosage range (MDI) | ||
|---|---|---|
| Drug and age range | Standard dose | High dose |
| Beclometasone diproprionate or budesonidea | ||
| Adult | 100–400 μcg twice a day | 400–1000 μcg twice a day |
| 12–18 years | ||