Neurologic speech disorders comprise motor speech disorders, including the dysarthrias and apraxia of speech, and other independent speech disorders, which include, but are not limited to, neurogenic stuttering, pseudo-foreign accent syndrome, echolalia, palilalia, aprosodia, akinetic mutism, and locked-in syndrome. 1 Each of these disorders may be caused by damage to different areas in the nervous system. The neurologic speech disorders encountered most often by SLPs are motor speech disorders. Thus, in this chapter, the dysarthrias and apraxia of speech are the primary focus.
9.1.1 Motor Speech Disorders
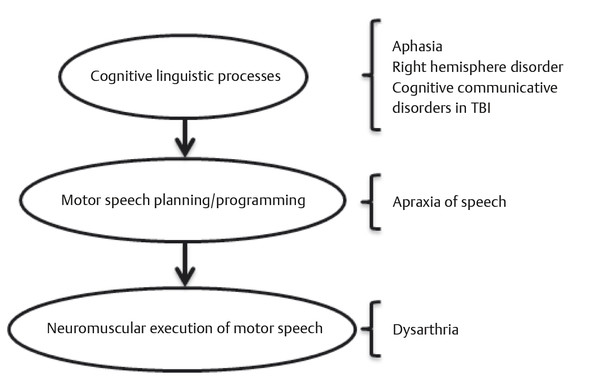
By far, the most common neurologic speech disorders encountered by SLPs are motor speech disorders (MSDs)—the dysarthrias and apraxia of speech. These disorders are caused by damage to the central and/or peripheral nervous system and influence the motor planning, motor programming, neuromuscular control, or execution of speech. To better understand MSDs, it is best to put them in context with the other neurologic communication disorders that are discussed in this book. ▶ Fig. 9.1 illustrates the conceptualization of the multiple processes of cognition, language, and motor speech programming and execution that are involved in communication.
Fig. 9.1 An illustration of the relationship between the categories and types of communication disorders
Dysarthria
The term dysarthria literally means abnormal articulation; however, in the medical setting, it is the term used to characterize a neurologic speech disorder that influences the neuromuscular control and/or execution of speech. More specifically, dysarthria is defined as
…a collective name for a group of neurologic speech disorders resulting from abnormalities in the strength, speed, range, steadiness, tone, or accuracy of movements, required for control of the respiratory, phonatory, resonatory, articulatory, and prosodic aspects of speech production. The responsible pathophysiologic disturbances are due to central or peripheral nervous system abnormalities and most often reflect weakness; spasticity; incoordination; involuntary movements; or excessive, reduced, or variable muscle tone. 1
As the definition suggests, dysarthria may be classified into different types based on the perceptual characteristics that reflect the changes in movement (strength, speed, range, steadiness, tone, accuracy) within the various systems involved in speech production (respiratory, phonatory, resonatory, articulatory, and prosodic). In addition, there is strong evidence that the types of dysarthria are associated with damage to specific areas within the nervous system. In medical speech-language pathology, the competent practitioner understands the differences in the types of dysarthria and is able to make an educated decision when applying a more specific label to a patient’s speech disturbance. In the following sections, the individual types of dysarthria are discussed in more detail. Specifically, the salient perceptual characteristics, pathophysiology, lesion localization, and common etiology are described.
Flaccid Dysarthria
Flaccid dysarthria results from damage to the lower motor neuron system, including the cranial nerves and/or spinal nerves. Overall, the most common perceptual characteristics of flaccid dysarthria reflect the muscle weakness that alters the quality of phonation, resonation, and prosody in connected speech. As it relates to phonation, patients may present with a breathy (and possibly harsh) vocal quality, short phrases during conversational speech, and audible inspiration. Resonatory incompetence may result in hypernasality, imprecise consonants, nasal emission, and short phrases. Altered prosody may present as speech that is monoloud and/or monopitch. The degree to which the components of the speech mechanism are affected depends upon the localization of damage in the peripheral nervous system. The cranial nerves that directly support speech motor movements and that are frequently implicated in flaccid dysarthria include the trigeminal (V), facial (VII), vagus (X), and hypoglossal (XII) nerves. Damage to the trigeminal nerve and facial nerve may result in significant changes in articulation and prosody when damage is bilateral rather than unilateral. The vagus nerve is most commonly implicated in flaccid dysarthria due to its involvement in motor control of the larynx and soft palate. Damage to the vagus nerve may result in changes in vocal quality (breathiness) and resonance (hypernasality). The hypoglossal nerve is involved in motor control of the tongue, thus damage to this nerve may result in changes in articulation and prosody. Damage to these cranial nerves may be due to variety of causes. Stroke, tumor, trauma, and viral infection (e.g., postpolio syndrome, herpes zoster) are potential etiologies. Diseases of the neuromuscular junction (e.g., myasthenia gravis, Lambert-Eaton myasthenic syndrome), demyelinating disease (e.g., Guillain-Barré), anatomical abnormalities (e.g., Chiari malformation), and degenerative diseases (e.g., amyotrophic lateral sclerosis, progressive bulbar palsy, muscular dystrophy, etc.) are also common causes of flaccid dysarthria.
Spastic Dysarthria
Spastic dysarthria results from bilateral damage to upper motor neurons within the central nervous system. The most common perceptual characteristics include a strained, strangled vocal quality, slow rate, and consonant imprecision, which reflect the influence of spasticity and weakness on the respiratory, laryngeal, velopharyngeal, and articulatory components of speech. In addition, patients may present as monopitch, monoloud, and hypernasal during speech tasks. During connected speech tasks, excess and equal stress (related to slowness of articulatory movement) and short phrases may be evident. The onset of the speech characteristics of spastic dysarthria may result from stroke, trauma, tumor, and infectious disease in the central nervous system. Degenerative diseases (e.g., amyotrophic lateral sclerosis, primary lateral sclerosis, progressive supranuclear palsy) and demyelinating diseases (e.g., multiple sclerosis) are also potential etiologies.
Ataxic Dysarthria
Individuals with ataxic dysarthria often present with complaints of “slurred,” “drunk,” or “intoxicated” speech. During perceptual evaluation, the most common characteristics include imprecise consonants, irregular articulatory breakdown, distorted vowels, excess and equal stress, prolonged phonemes, excessive loudness variations, slow rate, and monopitch voice, which reflect breakdown in the articulatory and prosodic components of speech. The characteristics of ataxic dysarthria are associated with deficits in motor execution and motor programming of speech 2 due to damage within the cerebellum, which is involved in the timing and coordination of movement. Frequently, ataxic dysarthria results from bilateral cerebellar damage or generalized cerebellar disease. However, unilateral focal lesions in the hemispheres and posteromedial or paravermal regions of the cerebellum, as well as lesions outside the cerebellum in the frontopontocerebellar pathways, may also produce an ataxic dysarthria. 1, 2 Common causes of ataxic dysarthria include stroke, degenerative diseases (e.g., Friedreich’s ataxia, olivopontocerebellar ataxia), demyelinating diseases (e.g., multiple sclerosis), trauma, tumor, and toxic/metabolic conditions (e.g., acute and chronic alcohol abuse, neurotoxic drugs).
Hypokinetic Dysarthria
Individuals with hypokinetic dysarthria may present with complaints of reduced loudness, fast speaking rate, mumbling, and/or stuttering during conversational speech. During the perceptual exam, the most common speech characteristics are monopitch and monoloud voice, reduced loudness, rapid rate of articulation, and short rushes of speech, which reflect impairments in the phonatory, respiratory, articulatory, and prosodic components of speech. Hypokinetic dysarthria results from damage to the basal ganglia control circuit, which is involved in regulating movement. Specifically, the basal ganglia regulate movement, in part, through excitation and/or inhibition of the direct activation pathway (promotes motor activity) and the indirect activation pathway (decreases motor activity). Hypokinesia, which may include akinesia (no movement) or bradykinesia (slow movement), results from decreased activity of the direct activation pathway and increased activity of the indirect activation pathway. In addition to hypokinesia, individuals with damage to the basal ganglia often demonstrate rigidity in all muscle groups. Together, these deficits influence the speed, range, force, and tone of muscle movements for speech. 3 By far, the most common cause of hypokinetic dysarthria is Parkinson’s disease and parkinsonism. Other degenerative diseases, including progressive supranuclear palsy 4 and multiple system atrophy, 5 may result in speech changes that are consistent with a hypokinetic dysarthria (often in combination with other types of dysarthria). Other, nondegenerative etiologies have been reported, including vascular (stroke, subarachnoid hemorrhage, subdural hematoma), toxic/metabolic conditions, trauma, infectious disease, and normal pressure hydrocephalus.
Hyperkinetic Dysarthria
Individuals with hyperkinetic dysarthria may present with complaints of effortful speech, involuntary and abnormal movements of their mouth and face, and difficulty with chewing and swallowing. 1 During perceptual exam, the most common perceptual characteristics include a strained-strangled-harsh vocal quality, consonant imprecision, irregular articulatory breakdowns, inappropriate and prolonged silent intervals, prolonged phonemes, excessive loudness variation, and voice stoppages. 1, 6 Together, these characteristics reflect potential changes in the respiratory, phonatory, articulatory, and prosodic components of speech. Like hypokinetic dysarthria, the clinical symptoms of hyperkinetic dysarthria result from damage to the control circuit of the basal ganglia. However, instead of an abnormal reduction in movement, or hypokinesia, there is an abnormal increase in movement, or hyperkinesia. The hyperkinesia is due to increased activity in the direct activation pathway and decreased activity in the indirect activation pathway. The most common causes of hyperkinetic dysarthria are toxic/metabolic disorders (e.g., tardive dyskinesia), degenerative diseases (e.g., Huntington’s chorea), infectious diseases (e.g., Sydenham’s chorea), vascular disease, trauma, Tourette’s syndrome, and orofacial dyskinesia. In some individuals with hyperkinetic dysarthria, the onset is due to an unknown etiology.
Unilateral Upper Motor Neuron Dysarthria
Individuals with unilateral upper motor neuron (UUMN) dysarthria often present with complaints of thick and slow speech, which deteriorates with fatigue and stress. They may also report issues with drooling and difficulty with chewing and swallowing. During perceptual exam, the most common characteristics are imprecise articulation, irregular articulatory breakdown, slow rate, and harsh vocal quality, which reflect changes in the phonatory, articulatory, and prosodic components of speech. UUMN dysarthria tends to be mild in severity and may be transient in some individuals. As its name suggests, it results from a unilateral lesion in the upper motor neuron system, including the cortex, subcortical structures, brainstem, thalamus, and the internal capsule. Common etiologies include vascular disorders, tumors, and trauma.
Mixed Dysarthria
The category of mixed dysarthria exists because it is possible that individuals may present with multiple types of dysarthria. This is due to the fact that neurologic disease is not always confined to a specific area of the brain and may influence multiple aspects of motor function. Thus, there are individuals who may present with mixed dysarthria types, including flaccid-spastic, ataxic-spastic, hypokinetic-spastic, ataxic-flaccid-spastic, and hyperkinetic-hypokinetic. Other combinations are possible, as well. Certain etiologies are more commonly associated with mixed dysarthria. Degenerative diseases, such as amyotrophic lateral sclerosis, multiple sclerosis, Friedreich’s ataxia, progressive supranuclear palsy, multiple system atrophy, and corticobasal degeneration, have been associated with mixed dysarthria due to the effects of these diseases on the upper motor neuron, lower motor neuron, and cerebellar systems. Toxic/metabolic conditions (e.g., Wilson’s disease), vascular disorders, trauma, and tumor may also result in a mixed dysarthria.
Apraxia of Speech
Apraxia of speech (AOS) is a neurogenic speech disorder that influences the motor planning and programming of speech. The definition and primary diagnostic characteristics have been debated and refined since the term was first proposed. The definition proposed by McNeil et al 7 is used in this chapter. The Academy of Neurologic Communication Disorders and Sciences (ANCDS) writing committee on AOS adopted this definition to determine inclusion of studies in its evaluation of the most current treatment literature, because it captures the current research findings regarding the most salient diagnostic characteristics. 8
McNeil et al 7 define AOS as
…a phonetic-motoric disorder of speech production caused by inefficiencies in the translation of a well-formed and filled phonologic frame to previously learned kinematic parameters assembled for carrying out the intended movement, resulting in intra and interarticulator temporal and spatial segmental and prosodic distortions. It is characterized by distortions of segment and intersegment transitionalization resulting in extended durations of consonants, vowels, and time between sounds, syllables, and words. These distortions are often perceived as sound substitutions and as the misassignment of stress and other phrasal and sentence-level prosodic abnormalities. Errors are relatively consistent in location within the utterance and invariable in type. It is not attributable to deficits in the processing of auditory, tactile, kinesthetic, proprioceptive, or language information. In its extremely infrequently occurring “pure” form, it is not accompanied by the above listed deficits of motor physiology, perception, or language.
Based on this definition, the ANCDS writing committee identified the primary diagnostic characteristics of AOS as
Slow rate of speech, typified by lengthened sound segments and intersegment durations.
Sound distortions.
Distorted, perceived, sound substitutions.
Errors that were relatively consistent in terms of type and invariable in terms of location.
Prosodic abnormalities.
In addition to these primary characteristics, individuals with AOS may also present with features that were originally thought to be core characteristics of AOS, but have been determined to be indistinguishable from other coexisting disorders, such as aphasia. These characteristics include articulatory groping, perseverative errors, increasing errors with increasing word length, speech initiation difficulties, awareness of errors, more errors in propositional speech, and islands of error-free speech. 8
9.2 Assessment
A proper assessment of oral motor and motor speech function is essential to the management of neurologic speech disorders. In general, assessment serves the following purposes:
Describes salient features and diagnose the presence of a specific speech disorder.
Determines severity of the speech disorder.
Indicates, confirms, or questions neurologic diagnosis and localization.
Formulates a prognosis.
Identifies treatment goals and potential treatment tasks.
Documents change over time.
Each of these purposes is important to the overall management of the patient with a neurologic speech disorder. Identifying the salient perceptual features of the patient’s speech is necessary to make a decision about the specific diagnosis of the speech disorder. For example, identifying that a patient presents with a weak, breathy vocal quality and hypernasal speech, but a relatively normal speaking rate, would lead the clinician to a diagnosis of a dysarthria and, more specifically, a flaccid dysarthria. Depending on the degree to which these features are present, the clinician will be able to provide a judgment of severity of the dysarthria. Moreover, the diagnosis of a particular type of dysarthria and the presenting features may suggest the lesion location. In the example of flaccid dysarthria, the lesion in the nervous system may be localized to the lower motor neuron system and, potentially, a more specific location (e.g., vagus nerve above the pharyngeal branch). It may also hint at a possible medical diagnosis. The history of presentation and the specific medical diagnosis will inform the prognosis for recovery, and repeated assessment may reveal change in performance over time.
9.2.1 Methods of Assessment
Three primary methods of assessment—auditory perceptual, acoustic, and physiologic—have been used to meet the purposes of assessment described above. The auditory-perceptual method is considered the gold standard of assessment, because determining the presence or absence of a speech disorder is based on whether or not it is perceived by the listener. In addition, compared to acoustic and physiologic measures, an auditory-perceptual assessment is available to all clinicians and is more cost effective, since specialized equipment—other than a microphone and a recording system—is not needed. 9, 10 However, the auditory-perceptual evaluation of speech and voice disorders, including neurologic speech disorders, is not without problems. In particular, the reliability of certain perceptual rating systems (e.g., the Mayo Clinic system for rating the dysarthrias) has been questioned. 11, 12 For the purposes of this chapter, the primary focus of the motor speech examination is on the assessment of auditory-perceptual features, followed by a discussion of recent advances in acoustic and physiologic measures.
Motor Speech Examination
The motor speech examination has multiple components, each of which is critical to the accurate description of signs and symptoms and the determination of the appropriate speech diagnosis. The components include obtaining a detailed history, examining the speech mechanism during nonspeech tasks, and assessing auditory-perceptual speech characteristics and intelligibility. The majority of these components may be completed in most clinical settings, including acute care, inpatient rehabilitation, outpatient clinic, and home health care settings.
History
A detailed patient history is important to understanding the nature of the speech disturbance. The initial history is the first time the clinician is able to learn about the patient’s personal history (education, occupation, marital status, children, etc.), listen to his or her speech during natural discourse, and make decisions regarding salient speech characteristics (e.g., articulation, phonation, respiration, resonance, and prosody). The history may yield information regarding the onset of the speech deficit. Patients who develop a change in speech function after stroke or traumatic brain injury will report an abrupt onset of symptoms that occurred immediately following the stroke or injury. A report of a gradual onset of symptoms may reflect the presence of a progressive neurologic condition. In some cases, a change in speech function may be the first symptom of a disease or disorder. The role of the SLP is to identify the timeframe for onset of the change in speech and the course of this change, that is whether it is stable, improving, or declining, according to the patient. The patient’s description of the change in speech may reveal his or her insight into the problem and/or his or her perception of how the problem has affected communication in different functional environments (e.g., home, community, avocational, vocational). The patient history provides an opportunity to examine the patient’s knowledge of potential medical diagnoses and the associated prognosis. This is important in all cases, but especially so in patients with progressive neurologic conditions, such as amyotrophic lateral sclerosis. The patient may or may not have come to terms with the potential progression of the disease.
9.2.2 Case Study 1
A 64-year-old woman was referred for a motor speech evaluation due to a reported change in speech function. During the interview, the patient stated that she first observed a change in her speech 8 months ago, although her family reports first observing a change more than 1 year ago. The patient noticed some imprecision in her speech in the evenings within a syllable or a sound within a word. In particular, it is most noticeable on the sounds /s/ and /sh/. She indicated that recently she has had to work to project her voice, but she has had issues with allergies over the past 3 weeks that have caused increased mucus, throat clearing, etc. The patient reported having dental surgery (a root canal) 2 years ago, after which the right side of her mouth was very sensitive and she developed a malocclusion. This caused her to chew on the left side of her mouth for an entire year. She began experiencing increased saliva production and when speaking would “spittle,” but this has decreased significantly.
The patient’s evaluation consisted of an oral-motor examination and auditory-perceptual assessment. Oral-motor examination was normal with the exception of mild lingual weakness. The auditory–perceptual assessment revealed the presence of a mild mixed (flaccid/spastic) dysarthria characterized by a slight breathiness to her vocal quality with intermittent mild strain and a noticeable vocal flutter during sustained phonation, mild inconsistent lingual articulatory imprecision, hypernasality, and her report of increased effort to talk and project her voice.
Given the patient’s history and presentation, a colleague with experience in assessing motor speech disorders was brought in for a second opinion. The two clinicians discussed the results of the evaluation and mentioned the terms upper motor neuron and lower motor neuron signs. At that moment, the patient stated, “I know what you’re talking about, and they’ve ruled out that diagnosis.” The patient was a retired nurse practitioner and was aware that the presence of upper and lower motor neuron signs is consistent with a possible ALS diagnosis. The patient became upset and the clinicians did their best to assure the patient that they were not making a medical diagnosis, but simply discussing the signs and symptoms observed during the assessment.
ALS had been ruled out by the patient’s neurologist. The patient was later seen by an otolaryngologist and a second neurologist, who diagnosed a progressive bulbar palsy, which later evolved into a confirmed ALS diagnosis.
Take-away message: Be careful how you discuss the results of an assessment with colleagues when the patient is present. In this case, it would have been better for the colleagues to excuse themselves and discuss the results privately. Instead, it resulted in increased anxiety for the patient related to the potential medical diagnosis. The clinicians’ identification of upper and lower motor neuron signs was accurate and confirmed by the ultimate diagnosis, but it was not their role to share this with the patient. Although there was a misstep in communication, this case also highlights the role of the SLP in identifying signs and symptoms that may lead to an accurate medical diagnosis.
Assessment of the Speech Mechanism during Nonspeech Activities
The assessment of the speech mechanism during nonspeech activities is commonly included in the assessment of motor speech disorders. The rationale for including such tasks during the motor speech examination is that they enhance the evaluation by isolating the movement of the lips, tongue, and jaw, which cannot be done during speech tasks. While this has been the prevailing practice since Darley and Aronson published their first textbook on motor speech disorders, 13 debate continues about the utility of nonspeech activities in informing the speech diagnosis and planning treatment (e.g., Weismer 14; Weismer & Liss 15). Weismer 14 argues that, while difficulty with nonspeech tasks may be associated with neurologic disease, there is little evidence that performance on these tasks informs the speech-production deficits in a patient with a motor speech disorder. Others acknowledge this view, but suggest that nonspeech tasks may be useful if the clinician has a clear rationale for implementing these tasks (e.g., to examine jaw movement more thoroughly) and recognizes the limitations of the assessment tasks. 16 In this chapter, we discuss patient performance during nonspeech activities not as an independent measure of motor speech function, but as a companion to the auditory–perceptual exam (discussed later in this chapter) to develop a complete picture of the patient’s speech disturbance.
Assessment of the oral mechanism. In general, an assessment of the speech mechanism during nonspeech tasks will include an examination of the oral mechanism (face, mouth, tongue, palate), the larynx, and the respiratory system. These tasks may be completed in any clinical environment (bedside, clinic room, patient’s home). The oral mechanism examination involves observing the patient’s face, mouth, tongue, and palate on a set of tasks in different conditions, including at rest, during sustained postures, during movement, and during elicitation of reflexes. In each condition, the purpose is to assess the movements in six domains:
Strength—the ability of the muscle to contract for extended period of time without excessive fatigue.
Symmetry—the appearance of both sides of the face at rest and during movement.
Range—the distance the oral structure can move during a task.
Tone—the continuous and passive partial contraction of muscles of the oral structures.
Steadiness—the degree to which the oral structure displays aberrant movement (e.g., tremor) at rest or during movement.
Speed—the rate at which the oral structure is able to move.
Accuracy—the successful execution of the motor movement.
▶ Table 9.1 includes a list of tasks that may be included in assessment of each of the oral structures. The tasks included in an assessment of the oral mechanism are simple to administer but require the SLP to observe the patient carefully and with purpose. Organizing the assessment in a structure similar to ▶ Table 9.1 and understanding the rationale behind each task will make interpretation of the information more meaningful. As is discussed later in the chapter, the Frenchay Dysarthria Assessment, 17 a commercially available assessment for motor speech disorders, includes similar tasks to assess the oral mechanism, as well as to assess the larynx, respiration, and reflexes.
Oral structure | Tasks |
Face at rest | Observe for symmetry, abnormal involuntary movement of eyes or lips, tremor-like movement of lips, fasciculations around the mouth or chin |
Face during sustained postures | Observe for the six domains during lip retraction, lip rounding/pursing, puffing of cheeks, and sustained mouth opening |
Face during movement | Observe for the six domains during speech, nonspeech tasks requiring rapid repetitions of the sustained posture tasks |
Jaw during rest | Observe the position at rest, presence of abnormal involuntary movements |
Jaw during sustained postures | Observe movement of jaw upon opening, ability to maintain closed mouth against examiner’s effort to open jaw, ability to maintain open mouth against examiner’s effort to close jaw |
Jaw during movement | Observe for the six domains during opening and closing of the jaw during nonspeech and speech tasks |
Tongue during rest | Observe for symmetry, abnormal involuntary movement, fasciculations |
Tongue during sustained postures | Observe for the six domains during sustained anterior protrusion past the lips and lateral protrusion into the cheeks, with and without resistance |
Tongue during movement | Observe for the six domains during rapid side to side movement of the tongue |
Velopharynx at rest | Observe for symmetry, abnormal involuntary movement of palate during wide-open mouth position |
Velopharynx during movement | Observe for symmetry of movement during sustained phonation (“ah”) |
Adapted from Duffy JR. Motor Speech Disorders: Substrates, Differential Diagnosis, and Management. Elsevier Health Sciences; St. Louis, Missouri; 2013. | |
Assessment of the larynx and respiration. If potential laryngeal and respiratory dysfunction is of concern during the assessment, a careful examination of the larynx and respiratory system during nonspeech tasks may be warranted. 18 Changes in these components of the speech mechanism due to neurologic damage or disease may be reflected in the patient’s speech during the auditory- perceptual examination. The purpose of assessing these components during nonspeech tasks is to determine the relative impact of changes to the larynx and respiration on the patient’s speech. The ANCDS guideline on the behavioral management of phonatory and respiratory dysfunction from dysarthria 18 included nonspeech tasks as one component of the physical examination associated with a comprehensive assessment of motor speech function.
The assessment of the larynx during nonspeech tasks may provide information about the integrity of vocal fold adduction and the potential interaction of the larynx and respiratory system on voicing. 1 This may be completed by having the patient produce a cough and/or glottal coup (sounds like a glottal stop). To ensure that the patient is able to perform each task properly, the clinician should provide the patient with a model for each activity. On both tasks, the clinician should attend to the sharpness of the sound and not the loudness, since the purpose is to assess vocal fold adduction. 1 If the sound produced on these tasks is less sharp or crisp, there may be weakness at the level of the vocal folds that is influencing vocal fold adduction. In addition to engaging the patient in a forced vocal fold adduction task, it is important to observe the patient during quiet breathing and when taking a deep breath to assess the presence or absence of inhalation stridor. Finally, in some cases, when there is concern about possible vocal fold pathology or potential paralysis or paresis of the vocal folds, instrumental studies, such as visualization of the vocal folds using a rigid or a flexible endoscope, may be employed.
The assessment of the respiratory system during nonspeech tasks may provide information about potential respiratory dysfunction and whether dysfunction is due to weakness, incoordination, involuntary movements, or maladaptive strategies. 18 Duffy 1 suggests clinicians look for the following potential characteristics of respiratory dysfunction while observing quiet breathing:
Posture while seated—slouching, forward, or side-bent posture.
Breathing—shortness of breath; rapid, shallow, or labored breathing; irregular breathing rate.
Abdominal and thoracic movements—limited in range; abrupt or slow movements.
Shoulder and neck movements—excessive movement, extension, or retraction.
Assessment of reflexes. During a motor speech examination, an SLP will evaluate the presence or absence of normal reflexes—those that are expected in a typical, intact nervous system—and primitive reflexes—those that are typical in infants, but disappear with development of the nervous system—in order to examine for potential damage in the central nervous system and the peripheral nervous system. Information gathered from an assessment of reflexes may aid in, or confirm, general lesion localization. Duffy 1 suggests assessing four reflexes: the gag reflex, jaw jerk, sucking reflex, and snout reflex. The gag reflex is a normal reflex whose primary purpose is airway protection. The reflex may be elicited by stroking the posterior tongue, the faucial pillar, or the posterior pharyngeal wall. The sensory input for the reflex is mediated by the glossopharyngeal nerve (CN IX) and the motor output is mediated by the vagus nerve (CN X). The reflex is present in approximately two-thirds of adults, 19 thus the absence of the reflex in a patient must be interpreted with caution. In some cases, the absence of the reflex may reflect damage to the glossopharyngeal and/or vagus nerve. The jaw jerk reflex is a primitive, dynamic stretch reflex that is mediated by the trigeminal nerve (CN V) for both sensory input and motor output. It is elicited by tapping the lower jaw, just below the lips while the patient is maintaining a slightly open mouth position. In most adults, this reflex is absent or very slight in response. When a brisk movement of the jaw is observed in a patient, it suggests the presence of upper motor neuron disease in the brainstem above the level of the trigeminal nerve nuclei. 1 The sucking reflex and snout reflex are primitive reflexes that are present in infants up to 1 year old but are absent in adults. 20 The sucking reflex is elicited by lightly touching or tapping the lips with a tongue blade. Duffy 1 recommends eliciting the reflex by placing the edge of a tongue blade at the corner of the upper lip and sweeping medially toward the philtrum. A positive reflex response results in a pursing of the patient’s lips. The snout reflex is elicited by lightly tapping the upper lip. A positive response is the protrusion of the patient’s lips. 20 The presence of the sucking or snout reflex is often consistent with frontal lobe disease, specifically lesions of the supplemental motor area, and is considered a “frontal release” sign. These reflexes are often seen in patients with dementias, encephalopathies, closed head injuries, and hydrocephalus. 20
Assessment of Auditory-Perceptual Speech Characteristics
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


