Anxiety Disorders I: Generalized Anxiety, Panic, and Social Anxiety Disorders
KEY CONCEPTS
![]() The long-term goal in treatment of generalized anxiety disorder is remission with minimal or no anxiety symptoms and no functional impairment.
The long-term goal in treatment of generalized anxiety disorder is remission with minimal or no anxiety symptoms and no functional impairment.
![]() Antidepressants are the agents of choice for the management of generalized anxiety disorder.
Antidepressants are the agents of choice for the management of generalized anxiety disorder.
![]() Antidepressants have a lag time of 2 to 4 weeks or longer before antianxiety effects occur in generalized anxiety disorder.
Antidepressants have a lag time of 2 to 4 weeks or longer before antianxiety effects occur in generalized anxiety disorder.
![]() When monitoring the effectiveness of antidepressants in panic disorder, it is important to allow an adequate amount of time (8 to 12 weeks) to achieve full therapeutic response.
When monitoring the effectiveness of antidepressants in panic disorder, it is important to allow an adequate amount of time (8 to 12 weeks) to achieve full therapeutic response.
![]() Clonazepam and alprazolam extended-release are alternatives to alprazolam immediate-release for patients with panic disorder having breakthrough panic symptoms at the end of a dosing interval.
Clonazepam and alprazolam extended-release are alternatives to alprazolam immediate-release for patients with panic disorder having breakthrough panic symptoms at the end of a dosing interval.
![]() The optimal duration of panic therapy is unknown; 12 to 24 months of pharmacotherapy is recommended before gradual drug discontinuation over 4 to 6 months is attempted.
The optimal duration of panic therapy is unknown; 12 to 24 months of pharmacotherapy is recommended before gradual drug discontinuation over 4 to 6 months is attempted.
![]() Social anxiety disorder is a chronic long-term illness requiring extended therapy. After improvement, at least a 1-year medication maintenance period is recommended.
Social anxiety disorder is a chronic long-term illness requiring extended therapy. After improvement, at least a 1-year medication maintenance period is recommended.
![]() The selective serotonin reuptake inhibitors or venlafaxine are considered first-line pharmacotherapy for social anxiety disorder.
The selective serotonin reuptake inhibitors or venlafaxine are considered first-line pharmacotherapy for social anxiety disorder.
![]() An adequate trial of antidepressants in generalized social anxiety disorder lasts at least 8 weeks, and maximal benefit may not be seen until 12 weeks.
An adequate trial of antidepressants in generalized social anxiety disorder lasts at least 8 weeks, and maximal benefit may not be seen until 12 weeks.
![]() The three principal domains in which improvement should be observed in generalized social anxiety disorder are symptoms, functionality, and well-being.
The three principal domains in which improvement should be observed in generalized social anxiety disorder are symptoms, functionality, and well-being.
Anxiety is an emotional state commonly caused by the perception of real or perceived danger that threatens the security of an individual. It allows a person to prepare for or react to environmental changes. Everyone experiences a certain amount of nervousness and apprehension when faced with a stressful situation. This is an adaptive response and is transient in nature.
Anxiety can produce uncomfortable and potentially debilitating psychological (e.g., worry or feeling of threat) and physiologic arousal (e.g., tachycardia or shortness of breath) if it becomes excessive. Some individuals experience persistent, severe anxiety symptoms and possess irrational fears that significantly impair normal daily functioning. These persons often suffer from an anxiety disorder.1
Anxiety disorders are among the most frequent mental disorders encountered in clinical practice. Healthcare professionals often mistake anxiety disorders for physical illnesses, and only one quarter of patients receive appropriate treatment.2 Failure to diagnose and manage anxiety disorders results in negative outcomes including overuse of healthcare resources, increased morbidity, and mortality.3 Individuals with anxiety disorders develop cardiovascular, cerebrovascular, gastrointestinal, and respiratory disorders at a significantly higher rate than the general population.4
To treat anxiety appropriately, the clinician must make a reliable diagnosis. It is essential that the distinction between short-term symptoms of anxiety and anxiety disorders be understood. Common or situational anxiety is a normal response to a stressful circumstance. Although symptoms can be severe, they are temporary and usually last no more than 2 or 3 weeks. Although short-term, “as-needed” treatment with an anxiolytic agent such as a benzodiazepine is common and can provide some symptomatic relief, prolonged drug therapy is not recommended for situational anxiety.5
EPIDEMIOLOGY
Anxiety disorders, as a group, are the most commonly occurring psychiatric disorders. According to the National Comorbidity Survey Replication of the prevalence, severity, and comorbidity estimates of mental disorders in the United States, the most recent 1-year prevalence rate for anxiety disorders was 19.1% in persons aged 18 years and older. Specific phobias were the most common anxiety disorder, with a 12-month prevalence of 9.1%. The 1-year prevalence of generalized anxiety disorder (GAD) was 2.7%, that of panic disorder was 2.7%, and that of social anxiety disorder (SAD) was 7.1%.6
In general, anxiety disorders are a group of heterogeneous illnesses that develop before age 30 years and are more common in women, individuals with social issues, and those with a family history of anxiety and depression. Patients often develop another anxiety disorder, major depression, or substance abuse.1–3 The clinical picture of mixed anxiety and depression is much more common than an isolated anxiety disorder.7
ETIOLOGY
The differential diagnosis of anxiety disorders includes medical and psychiatric illnesses and certain drugs.7 Hypotheses on the etiology of anxiety disorders are based on interactions between a combination of factors including vulnerability (e.g., genetic predisposition and early childhood adversity) and stress (e.g., occupational and traumatic experience). The vulnerability may be associated with genetic factors and neurobiologic adaptations of the central nervous system (CNS).8
Medical Diseases Associated with Anxiety
Anxiety symptoms are an inherent part of the initial clinical presentation of several diseases, thus complicating the distinction between anxiety disorders and medical disorders.4,7 Anxiety disorders are strongly and independently associated with chronic medical illness, low levels of physical health-related quality of life (QOL), and physical disability.4 If anxiety symptoms are secondary to a medical illness, they usually will subside as the medical situation stabilizes. However, the knowledge that one has a physical illness can trigger anxious feelings and further complicate therapy. Persistent anxiety subsequent to a physical illness requires further assessment for an anxiety disorder. Common somatic symptoms of anxiety that frequently present in medical disorders include abdominal pain, palpitations, tachycardia, sweating, flushing, tremor, chest pain or tightness, and shortness of breath. Although less specific, symptoms of muscle tension, headache, and fatigue are also common manifestations of anxiety. Medical disorders most closely associated with anxiety are listed in Table 53-1.4,9,10
TABLE 53-1 Common Medical Illnesses Associated with Anxiety Symptoms
Psychiatric Diseases Associated with Anxiety
Anxiety can be a presenting feature of several major psychiatric illnesses. Anxiety symptoms are extremely common in patients with mood disorders, schizophrenia, dementia, and substance-use disorders. Most psychiatric patients will have two or more concurrent psychiatric disorders (comorbidity) within their lifetime.6 It is important to diagnose and treat all comorbid psychiatric conditions in patients with anxiety disorders.
Drug-Induced Anxiety
Drugs are a common cause of anxiety symptoms (Table 53-2). Anxiety occurs during the use of CNS-stimulating drugs in a dose-dependent manner, but ingestion of minimal amounts can result in marked anxiety, including panic attacks, in some individuals. The onset of drug-induced anxiety is usually rapid after the initiation of therapy. A thorough medication history evaluating for a recent drug or dosage change is important to rule out a drug-induced etiology for the anxiety.
TABLE 53-2 Drugs Associated with Anxiety Symptoms
Anxiety occurs occasionally during the use of CNS depressants, especially in children and the elderly; however, anxiety complaints are more common as complications of drug withdrawal after the abrupt discontinuation of these agents.7,10
PATHOPHYSIOLOGY
Data from biochemical and neuroimaging studies indicate that the modulation of normal and pathologic anxiety states is associated with multiple regions of the brain and abnormal function in several neurotransmitter systems, including norepinephrine (NE), γ-aminobutyric acid (GABA), serotonin (5-HT), corticotropin-releasing factor (CRF), and cholecystokinin.11 Current neuroanatomic models of fear (i.e., the response to danger) and anxiety (i.e., the feeling of fear that is disproportionate to the actual threat) include some key brain areas. The amygdala, a temporal lobe structure, plays a critical role in the assessment of fear stimuli and learned response to fear.11,12 The locus ceruleus (LC), located in the brain stem, is the primary NE-containing site, with widespread projections to areas responsible for implementing fear responses (e.g., vagus, lateral and paraventricular hypothalamus). The hippocampus is integral in the consolidation of traumatic memory and contextual fear conditioning. The hypothalamus is the principal area for integrating neuroendocrine and autonomic responses to a threat.11,12
Neurochemical Theories
Noradrenergic Model
The basic premise of the noradrenergic theory is that the autonomic nervous system of anxious patients is hypersensitive and overreacts to various stimuli. Many anxious patients clearly display symptoms of peripheral autonomic hyperactivity. In response to threat or fearful situations, the LC serves as an alarm center, activating NE release and stimulating the sympathetic and parasympathetic nervous systems. Chronic central noradrenergic overactivity downregulates α2-adrenoreceptors in patients with GAD. This receptor is hypersensitive in some patients with panic disorder.11 By administering drugs that have a relatively specific effect on the LC, researchers have further explored the NE theory of anxiety and panic disorder. Drugs with anxiogenic effects (e.g., yohimbine [an α2-adrenergic receptor antagonist]) stimulate LC firing and increase noradrenergic activity. NE in turn increases glutamate release (an excitatory neurotransmitter).11 This produces subjective feelings of anxiety and can precipitate a panic attack in those with panic disorder, but not in normal volunteers.11 Drugs with anxiolytic or antipanic effects (e.g., benzodiazepines and antidepressants) inhibit LC firing, decrease noradrenergic activity, and block the effects of anxiogenic drugs.11
GABA Receptor Model
There are two superfamilies of GABA protein receptors: GABAA and GABAB. Drugs that reduce anxiety and produce sedation target the GABAA receptor. The GABAB receptor is a G-protein–coupled receptor postulated to be involved in the presynaptic inhibition of GABA release.11–13 GABAA receptors are ligand-gated ion channels composed of five protein subunits. Several classes of subunits (i.e., α1–6, β1–3, γ1–3, δ, ε, θ, π, ρ1–3) surround a central pore, and the receptor is connected to the cytoskeleton.14 Benzodiazepine ligands enhance the inhibitory effects of GABA.14 GABA, the major inhibitory neurotransmitter in the CNS, has a strong regulatory or inhibitory effect on the 5-HT, NE, and dopamine (DA) systems. When GABA binds to the GABAA receptor, neuronal excitability is reduced.
The specific role of the GABA receptors in anxiety disorders has not been established. The number of GABAA receptors can change with alterations in the environment (e.g., chronic stress), and the subunit expression can be altered by hormonal changes.14 In patients with GAD, benzodiazepine binding in the left temporal lobe is reduced.14 Abnormal sensitivity to antagonism of the benzodiazepine binding site and decreased binding was demonstrated in panic disorder.11,14 This is consistent with the suggestion that panic disorder is secondary to a lack of central inhibition that results in uncontrolled elevations in anxiety during panic attacks.13 Examination of whole brain and regional GABA in patients with SAD using proton magnetic resonance spectroscopy showed impairment of the GABA system.15
Serotonin Model
Although there are data suggesting that the 5-HT system is dys-regulated in patients with anxiety disorders, definitive evidence that shows a clear abnormality in 5-HT function is lacking. 5-HT is primarily an inhibitory neurotransmitter that is used by neurons originating in the raphe nuclei of the brain stem and projecting diffusely throughout the brain (e.g., cortex, amygdala, hippocampus, and limbic system). Abnormalities in serotonergic functioning through release and uptake at the presynaptic autoreceptors (5-HT1A/1D), the serotonin reuptake transporter (SERT) site, or effect of 5-HT at the postsynaptic receptors (e.g., 5-HT1A, 5-HT2A, and 5-HT2C) may play a role in anxiety disorders.11,13 Preclinical models suggest that greater 5-HT function facilitates avoidance behavior; however, primate studies show that reducing 5-HT increases aggression.11,13 It is postulated that greater 5-HT activity reduces NE activity in the LC, inhibits defense/escape response via the periaqueductal gray (PAG) region, and reduces hypothalamic release of CRF. The selective serotonin reuptake inhibitors (SSRIs) acutely increase 5-HT levels by blocking the SERT to increase the amount of 5-HT available postsynaptically, and are efficacious in blocking the manifestations of panic and anxiety.11
Low 5-HT activity may lead to a dysregulation of other neurotransmitters. NE and 5-HT systems are closely linked, and interactions between the two are reciprocal and vary. NE may act at presynaptic 5-HT terminals to decrease 5-HT release, and its activity at postsynaptic receptors can cause increased 5-HT release.
Buspirone is a selective 5-HT1A partial agonist that is effective for GAD but not for panic disorder. Because the selective 5-HT1A partial agonists reduce serotonergic activity, GAD symptoms may reflect excessive 5-HT transmission or overactivity of the stimulatory 5-HT pathways.16 There is circumstantial evidence for the involvement of serotonergic and dopaminergic systems in the pathophysiology of generalized SAD.17
Neuroimaging Studies
Functional neuroimaging studies support the crucial role of the amygdala, anterior cingulate cortex (ACC), and insula in the pathophysiology of anxiety.12 In GAD there is an abnormal increase in the brain’s fear circuitry, as well as increased activity in the prefrontal cortex, which appears to have a compensatory role in reducing GAD symptoms.18 Patients with panic have abnormalities of midbrain structures, including the PAG. Neuroimaging studies have shown activation of insula and upper brain stem (including the PAG), as well as deactivation of the ACC during experimental panic attacks.19 Patients with SAD have greater activity than matched comparison subjects in the amygdala and insula, structures linked to negative emotional responses.20,21 Both pharmacotherapy and psychotherapy decreased cerebral blood flow in the amygdala, hippocampus, and surrounding cortical areas in patients with SAD.21
CLINICAL PRESENTATION
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision classifies anxiety disorders into several categories: GAD, panic disorder (with or without agoraphobia), agoraphobia, SAD, specific phobia, obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), and acute stress disorder.1 The characteristic features of these illnesses are anxiety and avoidance behavior. Anxiety symptoms must cause significant distress and impairment in social, occupational, or other areas of functioning, and should not be secondary to a drug or illicit substance or a general medical disorder, or occur solely as part of another psychiatric disorder.1 OCD and PTSD are discussed in Chapter 54.
Generalized Anxiety Disorder
The diagnostic criteria for GAD require persistent symptoms for most days for at least 6 months.1 The essential feature of GAD is unrealistic or excessive anxiety and worry about a number of events or activities.1 The anxiety or apprehensive expectation is accompanied by at least three psychological or physiologic symptoms. Anxiety and worry are not confined to features of another psychiatric illness (e.g., having a panic attack, being embarrassed in public).1
The onset, course of illness, and comorbid conditions of GAD are important considerations. GAD has a gradual onset with an average age of 21 years; however, there is a bimodal distribution. Onset occurs earlier when GAD is the primary presentation and later when GAD is secondary. GAD can be exacerbated or precipitated in later life by severe psychological stressors. Most patients present between the ages of 35 and 45 years, with women twice as likely to have GAD as men. The course of the illness is chronic (i.e., episodes can last for a decade or longer); there is a high percentage of relapse and low rates of recovery. The likelihood of remission at 2 years is 25%.1 Patients report substantial interference with their lives and have a high probability of seeking treatment.9 Lifetime comorbidity with another psychiatric disorder occurs in 90% of patients with GAD, with depression being found in over 60%.9
CLINICAL PRESENTATION Generalized Anxiety Disorder
CLINICAL PRESENTATION A Panic Attack
Panic Disorder
Panic disorder begins as a series of unexpected (spontaneous) panic attacks involving an intense, terrifying fear similar to that caused by life-threatening danger. The unexpected panic attacks are followed by at least 1 month of persistent concern about having another panic attack, worry about the possible consequences of the panic attack, or a significant behavioral change related to the attacks.1 During an attack, patients describe at least four physiologic and physical symptoms. Panic attacks usually last no more than 20 to 30 minutes, with the peak intensity of symptoms within the first 10 minutes. Often patients seek help at a physician’s office or emergency department, only to have their symptoms resolve before or on arrival. Because panic symptoms mimic those present in several medical conditions, patients often are misdiagnosed, and multiple referrals are common.1
CLINICAL PRESENTATION Social Anxiety Disorder
Secondary to the panic attacks, up to 70% of patients develop agoraphobia.23,24 Agoraphobia is anxiety about being in places or situations in which escape might be difficult or where help might not be available in the event of a panic attack.1 As a result, patients often avoid specific situations (e.g., being in a crowd or flying) in which they fear a panic attack might occur.1
Complications of panic disorder include depression (10% to 65% have major depressive disorder), alcohol abuse, and high use of health services and emergency rooms.1 Patients with panic disorder have a high lifetime risk for suicide attempts compared with the general population.23,24 The usual course is chronic but waxing and waning.
Social Anxiety Disorder
SAD is characterized by an intense, irrational, and persistent fear of being negatively evaluated or scrutinized in at least one social or performance situation. Exposure to the feared circumstance usually provokes an immediate situation-related panic attack. In generalized SAD, fear and avoidance extend to various social situations, whereas in the nongeneralized form of SAD, fear is confined to only one or two social situations. Blushing is the principal physical indicator and distinguishes SAD from other anxiety disorders. Adults with SAD usually recognize their fear is excessive and unreasonable; however, they are unable to overcome it without treatment. If necessary, the feared situation is avoided or endured with significant distress.1 In individuals younger than 18 years of age, the duration of symptoms must be at least 6 months to meet the diagnostic criteria.1
The mean age of onset of SAD is during the mid-teens. Rates of SAD are slightly higher among women than among men and more frequent in younger cohorts. It is a chronic disorder with a mean duration of 20 years.1 People with SAD can be reluctant to seek professional help despite the existence of beneficial treatments because consultation with a clinician is perceived as a feared social interaction.25
Differentiating SAD from other anxiety disorders can be difficult. Panic attacks occur in both SAD and panic disorder, but the distinction between the two is the rationale behind fear; fear of anxiety symptoms is characteristic of panic disorder, whereas fear of embarrassment from social interaction typifies SAD.1,26 A majority of SAD patients eventually develop a concurrent mood, anxiety, or substance abuse disorder.25,26
Specific Phobia
Specific phobia is marked and persistent fear of a circumscribed object or situation (e.g., insects or heights). Apart from contact with the feared object or situation, the patient is usually free of symptoms. Most persons simply avoid the feared object and adjust to certain restrictions on their activities.1
TREATMENT
Generalized Anxiety Disorder
Desired Outcomes
The goals of therapy in the acute management of GAD are to reduce the severity and duration of the anxiety symptoms and to improve overall functioning. ![]() The long-term goal in GAD is remission with minimal or no anxiety symptoms, no functional impairment, and increased QOL.9 Prevention of recurrence is another long-term consideration.
The long-term goal in GAD is remission with minimal or no anxiety symptoms, no functional impairment, and increased QOL.9 Prevention of recurrence is another long-term consideration.
General Approach to Treatment
Once GAD is diagnosed, a patient-specific treatment plan, which usually consists of both psychotherapy and drug therapy, is developed. The plan depends on the severity and chronicity of symptoms, age, medication history, and comorbid medical and psychiatric conditions.9 Factors such as anticipated adverse effects, history of prior response in the patient or family member, patient preference, and cost should be considered when treatment is initiated. Psychotherapy is the least invasive and safest treatment modality. Antianxiety medication is indicated for patients experiencing symptoms severe enough to produce functional disability. Table 53-3 lists drug choices for GAD, panic disorder, and SAD.
TABLE 53-3 Drug Choices for Anxiety Disorders
Nonpharmacologic Therapy
Nonpharmacologic treatment modalities in GAD include psychoeducation, short-term counseling, stress management, psychotherapy, meditation, or exercise. Psychoeducation includes information on the etiology and management of GAD. Anxious patients should be instructed to avoid caffeine, nonprescription stimulants, diet pills, and excessive use of alcohol. Most patients with GAD require psychological therapy, alone or in combination with antianxiety drugs, to overcome fears and to learn to manage their anxiety and worry.5 Cognitive behavioral therapy (CBT) is the most effective psychological therapy in GAD patients. CBT for GAD includes self-monitoring of worry, cognitive restructuring, relaxation training, and rehearsal of coping skills.5 Psychotherapy or medication alone has comparable efficacy in acute treatment.22 The relapse rate with CBT is less than with other types of psychological modalities.22 Controlled trials comparing the efficacy of combining drug and psychotherapy over long-term treatment are lacking.22 Advantages of CBT over pharmacotherapy include patient preference and lack of troubling adverse effects. However, CBT is not widely available, requires specialized training, and entails weekly sessions for an extended time period (i.e., 12 to 20 weeks).5
Pharmacologic Therapy
The benzodiazepines are the most effective and commonly prescribed drugs for the rapid relief of acute anxiety symptoms (Table 53-4). All benzodiazepines are equally effective anxiolytics, and consideration of pharmacokinetic properties and the patient’s clinical situation will assist in the selection of the most appropriate agent.5,33
TABLE 53-4 Benzodiazepine Antianxiety Agents
Because of the lack of dependency and tolerable adverse effect profile, antidepressants have emerged as the treatment of choice for the management of chronic anxiety, especially in the presence of comorbid depressive symptoms. Buspirone is an additional anxiolytic option (Table 53-5) in patients without comorbid depression or other anxiety disorders (e.g., panic disorder and SAD). Because of the high risk of adverse effects and toxicity, barbiturates, antipsychotics, antipsychotic–antidepressant combinations, and antihistamines generally are not indicated in the treatment of GAD.3 The benzodiazepines are more effective in treating the somatic and autonomic symptoms of GAD as opposed to the psychic symptoms (e.g., apprehension and worry), which are reduced by antidepressants.3
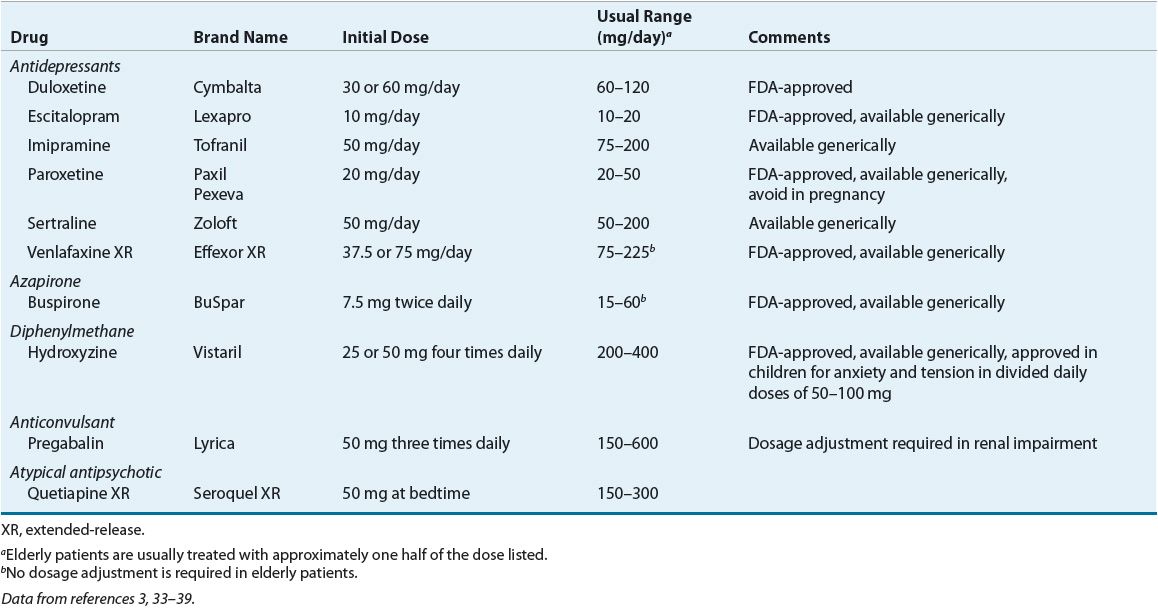
TABLE 53-5 Nonbenzodiazepine Antianxiety Agents for Generalized Anxiety Disorder
The most recent treatment guidelines from the World Federation of Societies of Biological Psychiatry and the National Institute for Health and Clinical Evidence are evidence-based.3,28 A descriptive flowchart with recommendations based on levels of evidence from the International Psychopharmacology Algorithm Project for the psychosocial and pharmacologic management of GAD is shown in Figure 53-1.40
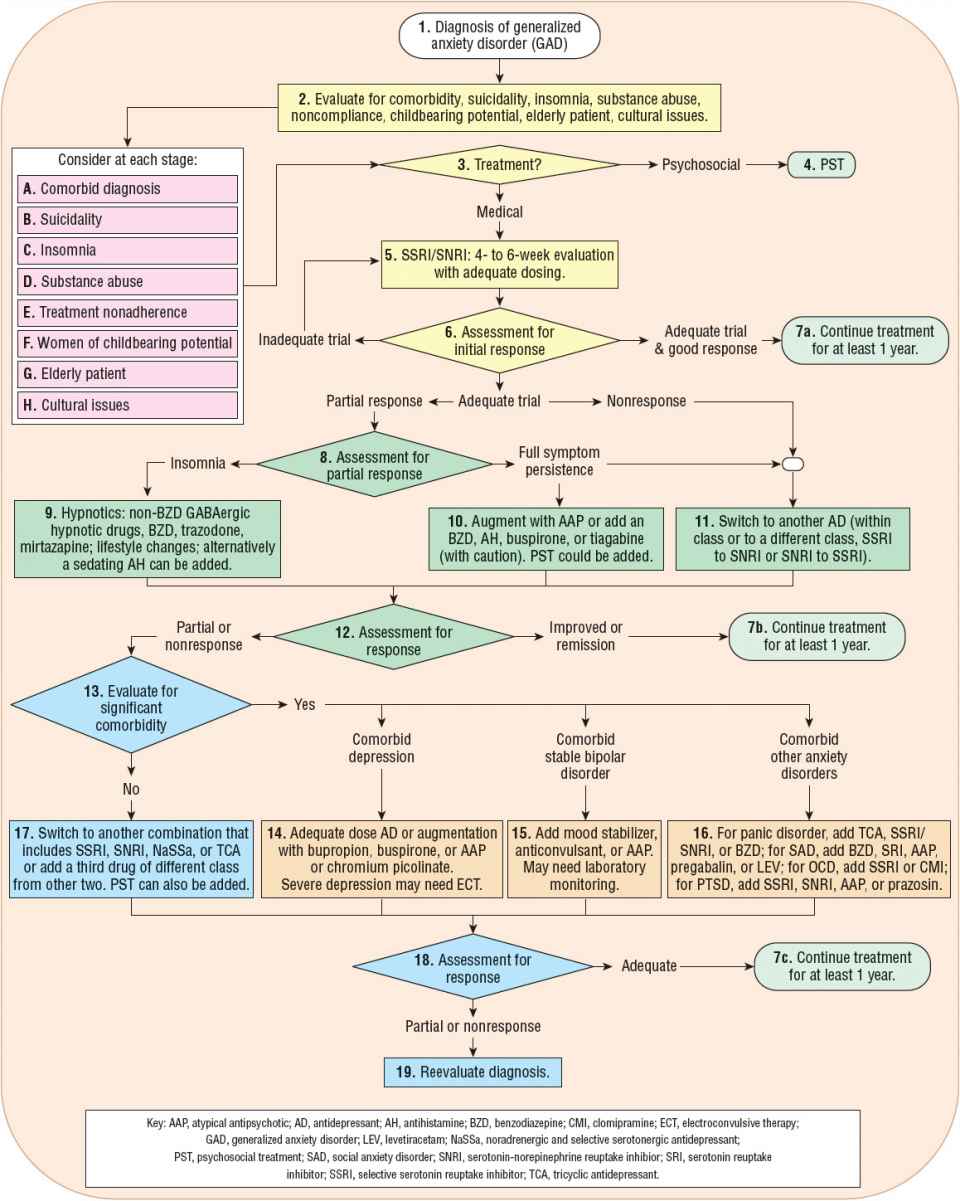
FIGURE 53-1 International Psychopharmacology Algorithm Project (IPAP) generalized anxiety disorder (GAD) algorithm flowchart. Yellow, first-line treatment (nodes 3–6); green, second-line treatment (nodes 8–12); blue, third-line treatment, no comorbidity (nodes 13–16); orange, third-line treatment, with comorbidity (nodes 14–16); light green, assessment and evaluation. Levels of evidence used in development of the flowchart were: 1, more than one placebo-controlled trial with sample sizes over 30; 2, one placebo-controlled trial (or active vs. active drug comparison) with sample size of 30 or greater; 3, one or small (n <30) placebo-controlled trial; 4, case reports or open-label trials; and 5, expert consensus without published evidence. (Flowchart is used by permission of the International Psychopharmacology Algorithm Project, http://www.ipap.org.40)
Alternative Drug Treatments
Hydroxyzine, pregabalin, and atypical antipsychotics are alternatives.9,22,34 The antihistamine hydroxyzine was effective in studies conducted for as long as 12 weeks in patients with GAD. Hydroxyzine is commonly used in the primary care setting, but it is considered be to be a second-line agent because of adverse effects and lack of efficacy for comorbid disorders.9 Pregabalin, which binds to the α2δ subunit of voltage-gated calcium channels to reduce nerve terminal calcium influx, acts on “hyperexcited” neurons. Pregabalin produced anxiolytic effects similar to lorazepam, alprazolam, and venlafaxine in acute efficacy trials.33 Quetiapine extended-release 150 mg/day monotherapy was superior to placebo in three studies, and as effective as paroxetine 20 mg/day and escitalopram 10 mg/day but with an earlier onset of action.34 In a 52-week treatment of GAD, quetiapine extended-release was superior to placebo in the prevention of anxiety relapse.34 Quetiapine is not FDA-approved for GAD, and the long-term risks and benefits of atypical antipsychotics in the treatment of GAD are unclear.34 Analysis of data from a pooled sample of trials found kava kava to be no more effective than placebo.41 Because of reports of hepatotoxicity, kava kava is not recommended as an anxiolytic.41 Although valerian, St. John’s wort, and passionflower have been used to manage GAD, there is insufficient evidence of their effectiveness and safety.42
Clinical Controversy
Antidepressant Therapy
![]() Antidepressants are considered first-line agents in the management of GAD. Venlafaxine extended-release, duloxetine, paroxetine, and escitalopram are FDA-approved antidepressants for GAD (see Table 53-5). Imipramine is considered a second-line agent, despite its efficacy, because of higher toxicity and adverse effect rates.3
Antidepressants are considered first-line agents in the management of GAD. Venlafaxine extended-release, duloxetine, paroxetine, and escitalopram are FDA-approved antidepressants for GAD (see Table 53-5). Imipramine is considered a second-line agent, despite its efficacy, because of higher toxicity and adverse effect rates.3 ![]() The antianxiety response of antidepressants is delayed by 2 to 4 weeks or longer.3 The pharmacology, pharmacokinetics, and drug interactions of the antidepressants are reviewed in Chapter 51.
The antianxiety response of antidepressants is delayed by 2 to 4 weeks or longer.3 The pharmacology, pharmacokinetics, and drug interactions of the antidepressants are reviewed in Chapter 51.
Efficacy Antidepressants are efficacious in the acute and long-term management of GAD. Data support the use of the SSRIs (e.g., escitalopram, paroxetine, sertraline), and the serotonin–norepinephrine reuptake inhibitors (SNRIs) (e.g., venlafaxine extended-release and duloxetine), for acute therapy (8- to 12-week trials) with response rates between 60% and 68%, and remission rates of 30%.3,22 A recent meta-analysis indicated that fluoxetine was most likely to achieve remission of GAD symptoms and sertraline was the most well tolerated. In a subanalysis comparing duloxetine, escitalopram, paroxetine, venlafaxine, and pregabalin, duloxetine was most likely to produce a beneficial response, escitalopram most likely to establish a remission, and pregabalin was best tolerated.43
Mechanism of Action The mechanism of action of antidepressants in anxiety disorders is not fully understood. Research indicates that antidepressants modulate receptor activation of neuronal signal transduction pathways connected to the neurotransmitters 5-HT, DA, and NE. In an animal model of anxiety, a number of candidate genes were identified that were normalized by fluoxetine treatment selectively in the hypothalamus.44 It is theorized that by activating stress-adapting pathways, SSRIs and SNRIs reduce the somatic anxiety symptoms and the general distress experienced by patients.
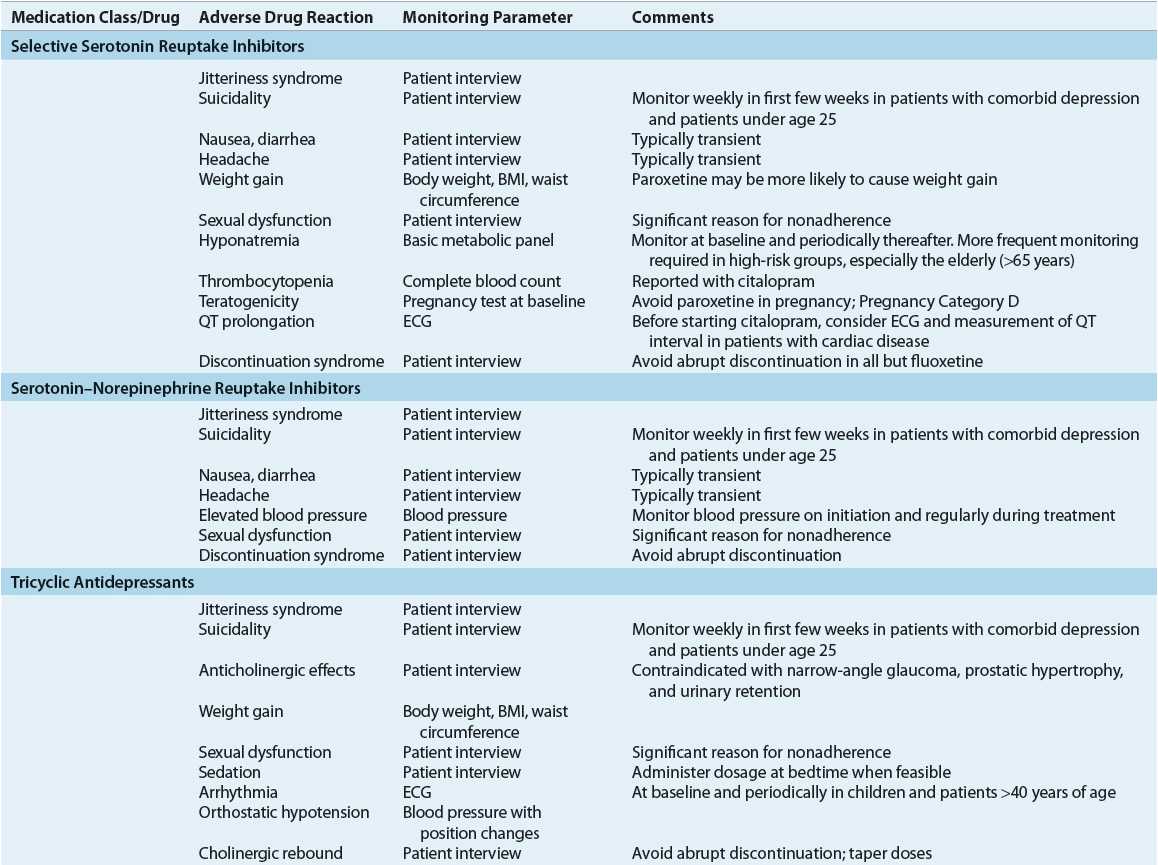
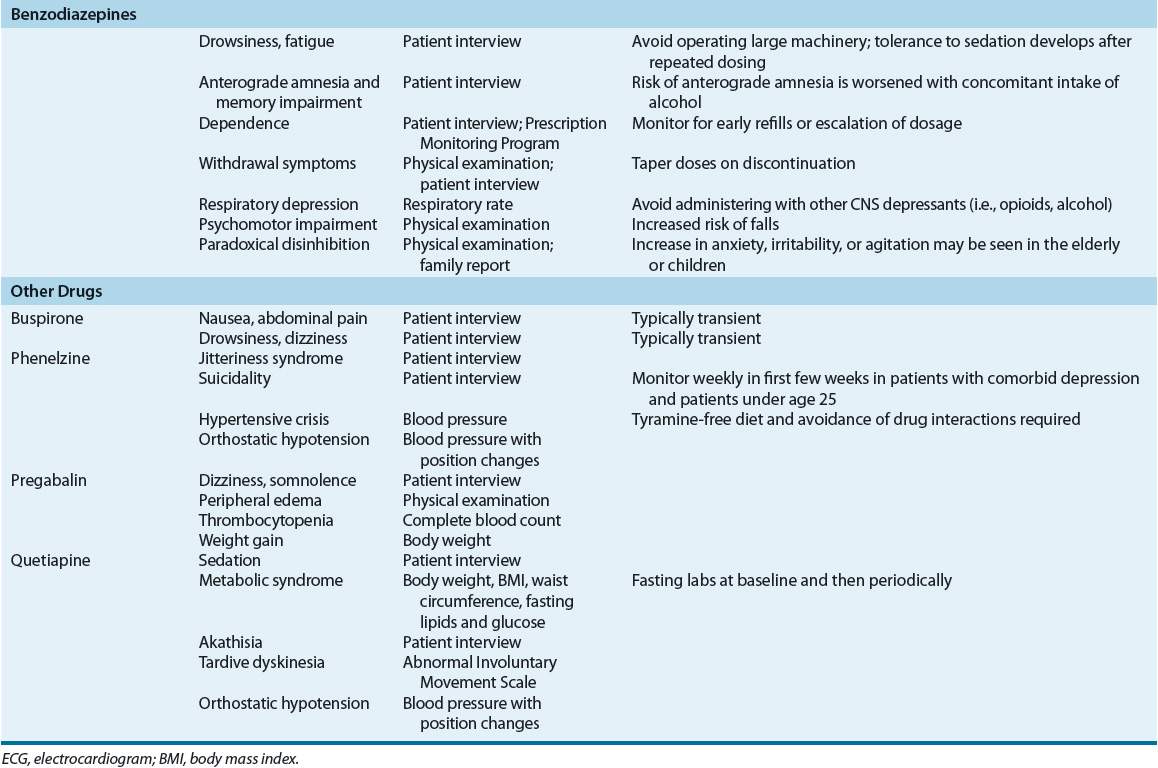
Adverse Effects The adverse effects of medications used to treat generalized anxiety are given in Table 53-6. SSRIs and SNRIs are generally well tolerated, with GI adverse effects and sleep disturbances being the most commonly reported. Headaches and diaphoresis occur early in treatment and are often transient, whereas weight gain and sexual dysfunction may continue in long-term treatment. The use of tricyclic antidepressants (TCAs) is limited by troublesome adverse effects (e.g., sedation, anticholinergic effects, and weight gain) in some patients and the risk of toxicity in overdose.
TABLE 53-6 Monitoring of Adverse Effects Associated with Medications Used in the Treatment of Anxiety Disorders