28 Anxiety disorders
Definitions and epidemiology
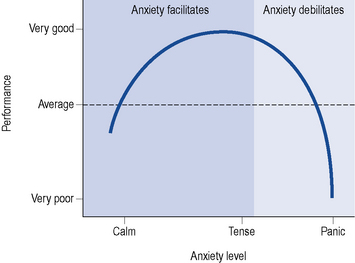
Anxiety is a normal, protective, psychological response to an unpleasant or threatening situation. Mild to moderate anxiety can improve performance and ensure appropriate action is taken. However, excessive or prolonged symptoms can be disabling, lead to severe distress and cause much impairment to social functioning. Figure 28.1 shows that as anxiety levels increase performance/actions increase. However, as the anxiety level increases beyond acceptable or tolerated levels, the performance declines.
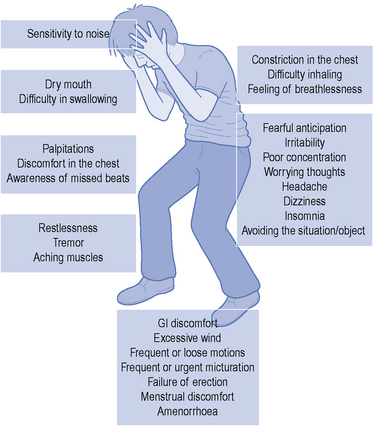
The term ‘anxiety disorder’ encompasses a variety of complaints which can either exist on their own or in conjunction with another psychiatric or physical illness. Symptoms of anxiety vary but generally present with a combination of psychological, physical and behavioural symptoms (Fig. 28.2). Some of these symptoms are common to many anxiety disorders while others are distinctive to a particular disorder. Anxiety disorders are broadly divided into generalised anxiety disorder (GAD), panic disorder, social phobia, specific phobias, post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD), see Table 28.1. Patient testimonials are presented in Box 28.1. Approximately two-thirds of sufferers of an anxiety disorder will have another psychiatric illness. This is most commonly depression and often successful treatment of an underlying depression will significantly improve the symptoms of anxiety. Many patients will also present with more than one anxiety disorder at the same time which can further complicate treatment. Anxiety disorders are the most commonly reported mental illness and as a whole have a lifetime prevalence of 21% (Baldwin et al., 2005) with specific phobias the most commonly reported.
Table 28.1 A brief description of the common anxiety disorders
| Symptoms common to all anxiety disorders | Fear or worry, sleep disturbances, concentration problems, dry mouth, sweating, palpitations, GI discomfort, restlessness, shortness of breath, avoidance behaviour |
| Generalised anxiety disorder (GAD) | Persistent (free floating), excessive and inappropriate anxiety on most days for at least 6 months. The anxiety is not restricted to a specific situation |
| Panic disorder (with or without agoraphobia) | Recurrent, unexplained surges of severe anxiety (panic attack). Most patients develop a fear of repeat attacks or the implications of an attack. Often seen in agoraphobia (fear in places or situations from which escape might be difficult) |
| Social phobia (or social anxiety disorder) | A marked, persistent and unreasonable fear of being observed, embarrassed or humiliated in a social or performance situation (e.g. public speaking or eating in front of others) |
| Specific phobia | Marked and persistent fear that is excessive or unrealistic, precipitated by the presence (or anticipation) of a specific object or situation (e.g. flying, spiders). Sufferers avoid the feared object/subject or endure it with intense anxiety |
| Post-traumatic stress disorder (PTSD) | Can occur after an exposure to a traumatic event which involved actual or threatened death, or serious injury or threats to the physical integrity of self or others. The person responds with intense fear, helplessness or horror. Sufferers can re-experience symptoms (flashbacks) and avoid situations associated with the trauma. Usually occurs within 6 months of the traumatic event |
| Obsessive-compulsive disorder (OCD) | Persistent thoughts, impulses or images (obsessions) that are intrusive and cause distress. The person attempts to get rid of these obsessions by completing repetitive time-consuming purposeful behaviours or actions (compulsions). Common obsessions include contamination while the compulsion may be repetitive washing or cleaning |
Box 28.1 Patient testimonies (NICE, 2005a,b)
Symptoms described by a sufferer of post-traumatic stress disorder:
Thoughts from a sufferer of obsessive-compulsive disorder:
A slow recovery described by a post-traumatic stress disorder and panic attack sufferer:
Pathophysiology
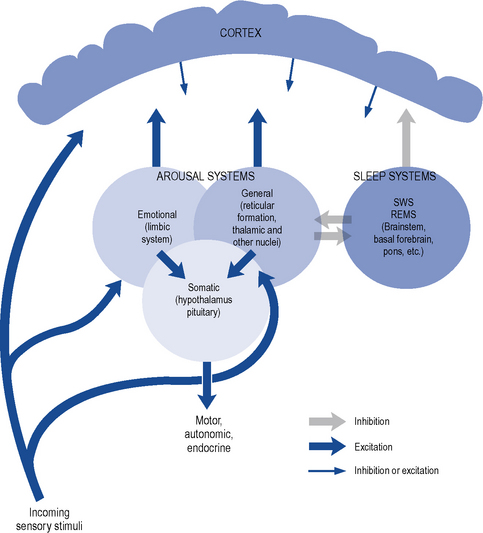
Anxiety occurs when there is a disturbance of the arousal systems in the brain. Arousal is maintained by at least three interconnected systems: a general arousal system, an ‘emotional’ arousal system and an endocrine/autonomic arousal system (Fig. 28.3). The general arousal system, mediated by the brainstem reticular formation, thalamic nuclei and basal forebrain bundle, serves to link the cerebral cortex with incoming sensory stimuli and provides a tonic influence on cortical reactivity or alertness. Excessive activity in this system, due to internal or external stresses, can lead to a state of hyperarousal as seen in anxiety. Emotional aspects of arousal, such as fear and anxiety, are contributed by the limbic system which also serves to focus attention on selected aspects of the environment. There is evidence that increased activity in certain limbic pathways is associated with anxiety and panic attacks.
Treatment
Psychotherapy
Other psychotherapies, although occasionally tried, have a poorer evidence base than CBT and are, therefore, not usually recommended. Self-help is one alternative technique which is recommended (NICE, 2007) for GAD and panic disorder. It involves using materials either alone or in part under professional guidance to learn skills to help cope with the anxiety. The materials such as books, tapes or computer packages can be accessed at home and in the patients’ own time. Some self-help material, however, is of poor quality, so it is probably best used in those who have mild symptoms and who do not need more intensive treatments.
Pharmacotherapy
Benzodiazepines
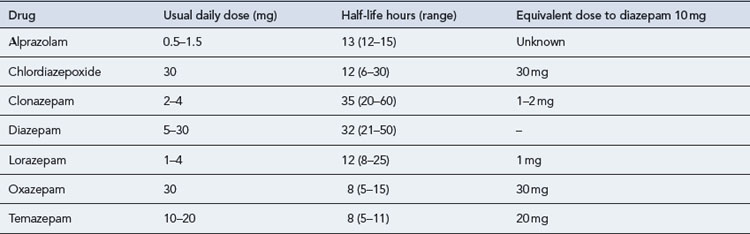
Benzodiazepines are commonly prescribed to provide immediate relief of the symptoms of severe anxiety. A number of different benzodiazepines are available (Table 28.2). These drugs differ considerably in potency (equivalent dosage) and in rate of elimination but only slightly in clinical effects. All benzodiazepines have sedative/hypnotic, anxiolytic, amnesic, muscular relaxant and anticonvulsant actions with minor differences in the relative potency of these effects.
Pharmacokinetics
Most benzodiazepines are well absorbed and rapidly penetrate the brain, producing an effect within half an hour after oral administration. Rates of elimination vary; however, with elimination half-lives from 8 to 35 h (see Table 28.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree