■ When an antrectomy is performed for complicated peptic ulcer disease, a vagotomy may be included to reduce the chance of anastomotic ulcer formation in patients who are not candidates for H. pylori treatment and lifelong proton pump inhibitor therapy due to unreliability, noncompliance, or medication side effects.5,6
■ Antrectomy is named by the type of gastrointestinal (GI) anastomosis performed.
■ Billroth I procedure—antrectomy and gastroduodenostomy
■ Billroth II procedure—antrectomy and gastrojejunostomy
■ A modification of the Billroth II procedure that involves a gastrojejunostomy via a Roux limb and is known as a Roux-en-Y gastrojejunostomy
DIFFERENTIAL DIAGNOSIS
■ Complicated peptic ulcer disease and distal gastric neoplasms, both benign and malignant, account for the vast majority of the antral resections performed today. These diagnoses will be discussed separately.
■ Peptic ulcer disease
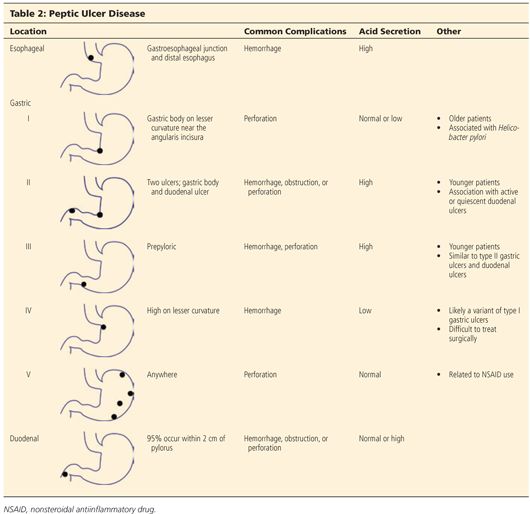
■ Peptic ulcer disease refers to irritation of GI mucosa from gastric acid due to either increased acid presence or weakness in the mucosal protection and typically presents with epigastric pain.2,4 Peptic ulcers can occur anywhere in the GI tract, but duodenal and gastric ulcers are most common. Duodenal ulcers typically arise within 2 cm of the pylorus, are highly associated with H. pylori infection (>90%), and frequently resolve with appropriate H. pylori therapy. Gastric ulcers are less likely to be associated with H. pylori infection and are classified into five types based on their location and association with acid secretion (Table 2).7
■ The differential diagnosis of epigastric pain similar to that found in complicated peptic ulcer disease is chronic cholecystitis, acute pancreatitis, chronic pancreatitis, functional indigestion or dyspepsia, gastritis, and reflux esophagitis. Complicated peptic ulcer disease can also present with upper GI hemorrhage, and a differential should include esophagitis (reflux and infectious); gastroesophageal varices, arteriovenous malformations; Mallory-Weiss tear; stress gastritis; and neoplasm of the esophagus, stomach, duodenum, pancreas, and biliary tree.
■ Lastly, pyloric obstruction due to chronic inflammation and scarring will cause nausea, emesis, and early satiety. The differential for these symptoms includes gastric motility disorders (i.e., gastroparesis), gastroenteritis, small bowel obstruction, electrolyte abnormalities, and extrinsic compression from pancreatic pseudocysts or neoplasms.
■ Distal gastric neoplasms—Gastric neoplasms include benign polyps, adenocarcinoma, neuroendocrine tumors, lymphoma, B-cell mucosa-associated lymphoid tissue (MALT) lymphomas, GI stromal tumors, leiomyomas, and leiomyosarcomas. Any gastric neoplastic process can cause upper GI bleeding, epigastric pain, and luminal obstruction, and a differential similar to peptic ulcer disease should be considered.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ All patients should undergo a thorough history and physical exam with questions focusing on the nature of the symptoms, specifically determining the relationship between symptoms and eating, deciphering whether symptoms are acute or chronic, and determining the severity of the symptoms. A vast majority of patients will have abdominal pain. Pain related to peptic ulcer disease that results from the corrosive effect of gastric acid on vulnerable GI mucosa and typically occurs in the epigastrium is described as gnawing or burning and follows a daily cycle. This pain typically arises shortly after eating breakfast and persists until lunch at which time the oral intake alleviates the pain. Relief is transient and pain recurs in the early afternoon and again persists until dinner. Meals, specifically ones consisting of milk and dairy products, and antacids provide temporary relief from ulcer pain. Acute, severe epigastric pain can signify ulcer perforation, whereas back pain suggests ulcer penetration into the pancreas.8
■ Nausea and vomiting can be seen with ulcer disease even in the absence of pyloric obstruction. Nausea that is chronic in nature and associated with early satiety and weight loss suggests inflammation and scarring of the pyloric channel due to chronic ulceration.
■ It is not uncommon for complicated peptic ulcers to present with upper GI bleeding, perforation, or obstruction in a patient with no history of peptic ulcer disease.
■ Bleeding—hematemesis, melena, recent diagnosis of anemia
■ Perforation—acute onset upper abdominal pain and peritonitis
■ Obstruction—nausea, emesis, food regurgitation, early satiety, weight loss
■ Acute or chronic upper GI bleeding can signify complicated ulcer disease and may present as melena, weakness, fatigue, general malaise, or a recent diagnosis of anemia.
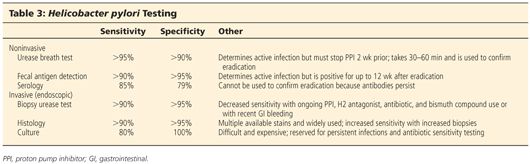
■ Risk factors for developing ulcer disease include a history of H. pylori infection; smoking; Zollinger-Ellison syndrome; and use of nonsteroidal antiinflammatory drugs (NSAIDs), steroids, and other immunosuppressive medications.1,8 Therefore, an accurate medication list should be obtained and reviewed with the patient. History of previous ulcer disease should be elicited, and the success and timing of previous treatment modalities should be documented. Presence of H. pylori infection, completion of antibiotic therapy, and documentation of eradication is crucial (Table 3). Ulcers that persist despite appropriate treatment of H. pylori, cessation of NSAID use, or are found in H. pylori–negative patients should raise suspicion for underlying malignancy.
■ A gastric lesion can also present with epigastric pain and obstruction. This pain is typically vaguer in nature and lacks a gnawing or burning component. Furthermore, these patients may describe a sensation of persistent fullness and early satiety despite hunger.
■ A subjective assessment of nutrition and functional status is necessary to evaluate the patient’s ability to tolerate a major surgical procedure.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Diagnostic evaluation of suspected peptic ulceration and upper GI lesions can include endoscopy, contrast radiography, and computed tomography (CT) (FIG 1).
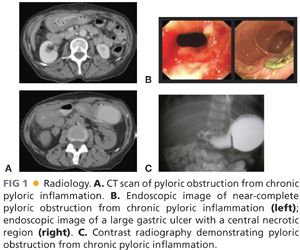
■ Endoscopy is felt to be superior because it allows for tissue sampling. Sampling of gastric mucosa can be used to confirm the presence of H. pylori. On endoscopy, ulcers are sharply demarcated; often have exposed underlying submucosa; and frequently occur in the first portion of the duodenum, the prepyloric area, and the pyloric channel. All gastric ulcers should be biopsied at least six times at the ulcer edge and brush biopsied to evaluate for underlying malignancy. Even if negative for malignancy, repeat endoscopy after medical treatment is indicated to evaluate for therapeutic response, and in instances of persistent or intractable disease, ulcer resection is indicated.8
■ Other relevant imaging modalities include contrast radiography and CT. Double-contrast radiography of the upper GI tract detects roughly 90% of gastric and duodenal ulcers but does not allow for tissue sampling. In the acute setting, CT is helpful in identifying gastric or duodenal ulcer perforation. Additionally, CT can identify wall thickening in chronic ulcer inflammation or neoplastic situations but again lacks the ability to provide tissue sampling.
■ Zollinger-Ellison syndrome is a rare condition of increased serum gastrin levels secondary to a gastrinoma with resulting severe ulcer disease. In nonsmoking patients who are negative for H. pylori, serum fasting gastrin levels should be obtained to evaluate for Zollinger-Ellison syndrome. Normal basal gastrin levels average to 50 to 100 pg/mL, and levels over 200 pg/mL can almost always be considered high. Diagnosis of Zollinger-Ellison syndrome can alter your treatment approach.9
SURGICAL MANAGEMENT
■ The indications for antrectomy are listed in Table 1. As explained earlier, an antrectomy is rarely performed for its original purpose of removing the antrum and reducing acid secretion.
■ Antrectomy is not the primary treatment option for bleeding or perforated peptic ulcers. A vast majority of bleeding ulcers is controlled endoscopically and, in the 5% to 10% that require operative intervention, a formal antrectomy is rarely needed. Roughly 90% of perforated ulcers can be safely controlled with primary closure and omental patching. Thus, antrectomy for bleeding or perforated ulcers is reserved for cases when less invasive treatment options are ineffective.
Preoperative Planning
■ All patients should undergo preoperative endoscopy to identify the extent of disease and preoperative nutritional assessment. All patients should receive preoperative antibiotics in a timely fashion to reduce the risks of perioperative infectious complications from gram-positive cocci and enteric gram-negative bacilli pathogens.
■ Several factors must be considered when deciding between performing a Billroth I and Billroth II procedure. The advantage to a Billroth I procedure is that the anatomic arrangement of the GI tract is preserved, which maintains the innate regulatory pathways of bicarbonate and pancreatic enzymes and significantly decreases the rate of postprandial dumping. Unfortunately, the lack of a pylorus results in bile reflux gastritis in a majority of patients. A Billroth I procedure cannot always be performed due to inflammation and scarring from prepyloric, pyloric, or duodenal ulcers. In these instances, the Billroth II procedure allows for a tension-free anastomosis of noninflamed tissue but introduces the problems of potential afferent loop syndrome and bile reflux gastritis, whereas a Roux-en-Y gastrojejunostomy diminishes the occurrence of bile reflux at the cost of a second anastomosis. Lastly, in cases of invasive neoplasms or concerning gastric masses, a Billroth II procedure with or without reconstruction with a Roux-en-Y gastrojejunostomy is preferred as it allows for dissection of much wider margins and is less likely to obstruct in the unfortunate setting of recurrent disease.10,11
Positioning
■ The patient should be positioned supine with arms out. A urinary catheter and a nasogastric tube should be placed to decompress the stomach. Positioning should allow for attachment of a self-retaining retractor system to the operating room table.



