Introduction
Infectious disease is a major cause of death and disability throughout the world. Many micro-organisms live either inside or on the outside of the human body. These cause disease only when our resistance is lowered through other diseases or when our natural barriers have been affected by disease or trauma. Other micro-organisms are present in the external environment and are taken into our bodies through eating and drinking, breathing or on physical contact.
Micro-organisms that live in or on our bodies for the most part have a harmless relationship with us and can be beneficial – for example, bacteria in the GI system break down foodstuffs allowing us to absorb vitamin K. Unfortunately, at times of vulnerability these same organisms can cause infection and damage. Many other micro-organisms not normally present in the body attempt to invade our tissues, causing damage which can be life-threatening. Any invasion or abnormal growth pattern of micro-organisms which causes our body to defend itself is an infection. An example would be peritonitis – the inflammation of the delicate serous membrane which lines the abdominal and pelvic cavities and covers the organs which lie within.
Infectious micro-organisms are categorized into four main groups: bacteria, viruses, protozoa and fungi. Bacteria and fungi are capable of existing independently of their host – i.e. us. Some protozoa and certainly viruses need the mechanisms from our cells in order to replicate and grow. A further category of infectious agent is called a prion. These have been particularly press-worthy over the years as they cause bovine spongioform encephalopathy (BSE).
This chapter is designed to give you an introduction to some of the medicines used in combating infections caused by micro-organisms. Drugs used to combat the variety of micro-organisms which may cause us harm are referred to as antimicrobials. The chapter is in no way comprehensive and is intended to whet your appetite to read further, so increasing your knowledge. The chapter covers antibiotic therapy, antiviral therapy, antiprotoza therapy and finally antifungal therapy. We have tried to give examples of common drugs that you may come across in practice rather than concentrate on a range of drugs that you may only encounter rarely.
Bacterial infection
We are surrounded by bacteria, most of which are harmless. Having said this, it is probably safe to say that more deaths and disease have been caused by bacteria than any other cause.
Bacteria are classified into a number of types based on how they appear through a microscope – i.e. the shape of them. Some look like rods, and are called bacilli. Some are round in shape and are called cocci. Others have a spiral or corkscrew shape and are known as spirochaetes. Bacteria are also categorized by whether they take up a stain called gram stain. Bacteria that absorb this stain are termed gram positive, while those that do not are gram negative.
The reason for the difference in the uptake of gram stain is a difference in the cell walls of the bacteria. Gram positive bacteria have a simple cell wall whereas the cell wall of gram negative organisms is much more complex. Difficulty in penetrating this complex wall is likely to be why some antibiotics are less effective against gram negative than gram positive bacteria.
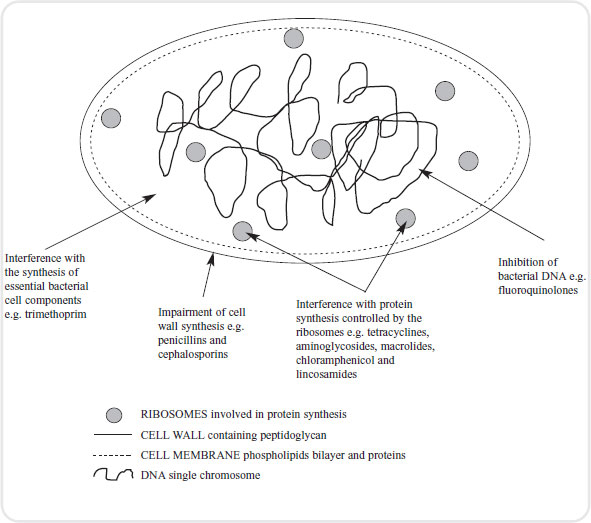
Bacteria cells are different from those of humans. Bacteria do not have a nucleus and so are called prokaryotes. Our cells do have a nucleus and are called eukaryotes. This and other differences between bacteria and human cells is important as antibiotics are designed to target these differences, thus destroying the bacteria while leaving our own cells intact.
On the very outside of a bacterium is a wall made largely from a sugar called peptidoglycan. This is unique to prokaryotic cells. Beneath this wall is a plasma membrane very similar to our own and consisting of a sandwich of phospholipids and proteins. The cell wall and plasma membrane together are called the bacterial envelope.
A bacterium contains cytoplasm which carries similar organelles to our own. However the genetic material is arranged in one long strand that floats around in the cytoplasm. A prokaryotic cell does not have any mitochondria and energy production is carried out in the plasma membrane (see Figure 4.1).
Antibiotics are often described as being bactericidal: in other words, they kill bacteria, usually very rapidly. They are also bacteriostatic, which means that the antibiotic prevents the growth of an infection but does not eradicate it totally. Instead it gives the body’s natural defence mechanisms time to recognize and deal with the infection. The distinction between these two terms is not black and white because in certain conditions a bactericidal antibiotic may only have a bacteriostatic effect and vice versa. Their effects are somewhat governed by dosage, outside influences and the health of the patient.
Selective toxicity is the ability of the antimicrobial to harm a pathogen (bacteria) without harming our own cells. Therefore, when discussing selective toxicity in terms of an antibiotic, health care practitioners are referring to the range between the dose necessary to inhibit or destroy the bacteria and the dose at which our own cells become harmed. Thus an antibiotic that is far more toxic to the bacteria than our cells is said to have a greater selective toxicity.
Interference with folate
Folate is a vitamin required by both bacterial and human cells. Human cells have evolved a mechanism to directly take up folate from the interstitial fluid. Bacteria on the other hand have to make their own folate and cannot absorb it directly from the environment.
A group of antibiotics called sulfonamides exploit this difference between bacterial and mammalian cells. Bacteria need a substance called PABA (see Chapter 3) in order to make the folate they need. Sulfonamides fool the bacteria into taking up a substance that looks identical to PABA but cannot be used by the bacteria. In this way, they prevent the cell reproducing and are therefore bacteriostatic in nature.
Trimethoprim
This sulfonamide drug is sometimes given as a combination called co-trimoxazole. Trimethoprim is given orally as it is well absorbed by the GI system. The drug is usually given to treat urinary and respiratory infections and may be prescribed with sulfamethoxazole as co-trimoxazole. However, this tends to be limited to treating patients with acquired immuno-deficiency syndrome (AIDS) for a particular type of pneumonia.
Beta-lactam antibiotics
Peptidoglycan makes up to 50 per cent of the cell wall in bacteria. In some cells this wall is very thick. However, certain antibiotics stop the bacterial cell from making this substance, thus rendering the cell useless. This is how drugs such as penicillins and cephalosporins work.
Penicillins
The first penicillin was the naturally occurring benzylpenicillin, and is still used today. The main drawback with this drug is that it is poorly absorbed from the GI tract so can only be administered by injection. Also, due to the length of time it has been used, many bacteria have developed enzyme systems to combat its effects. Therefore, various semi-synthetic versions have been prepared by altering the basic biochemistry of the drug. You will no doubt come across many of these in your experiences within health care settings. Examples include flucloxacillin, ampicillin and amoxicillin. The -illin suffix is a useful way of identifying these types of drugs. They can be given orally in a number of forms (tablet, syrup and suspension).
Penicillins are the drugs most likely to cause anaphylactic reactions, and are thought to be responsible for 75 per cent of anaphylactic deaths. It is sometimes feasible to carry out a skin test for hypersensivity. However the results are not always conclusive and the patient may suffer a severe reaction to only a small amount of the drug. Cefuroxime appears to be a safe alternative but not 100 per cent safe, so care must be taken.
Penicillins can have an adverse effect on the normal bacteria that live in our digestive systems. Sometimes this results in diarrhoea which can lead to a lack of vitamin K absorption. In addition, infections by micro-organisms not sensitive to penicillin can take place. In other words, the fine balance in the digestive system between good and bad bacteria can be altered by penicillin therapy.
Cephalosporins
These drugs are chemically related to the penicillin group. Similarly, many semi-synthetic drugs have also been developed. As a result there is a large range of medicines in this group that can be prescribed for infections.
These drugs work in the same way as penicillin in that they affect the production of the peptidoglycan wall of the bacterium. Today they are extremely important, due to the production of enzymes against the biochemical make-up of penicillins which have made those drugs less effective in preventing infection.
Some cephalosporins may be given orally; for example, cefalexin. However, most of this group of drugs are given via the IV or SC routes; for example, cefuroxime and cefotaxime are administered in this way. After being absorbed, cephalosporins are widely distributed in the tissues of the body. Some can actually cross over the BBB; for example, cefuroxime. This drug therefore is useful for infections in the central nervous system. Excretion is mainly by the kidneys but some cephalosporins, for example, cefoperazone, are eliminated in the bile. These drugs can work on both gram negative and gram positive bacteria but this depends on which drug is prescribed.
Side-effects are similar to those of the penicillin group, so hypersensitivity reactions can occur. Between 0.5 and 6.5 per cent of penicillin-sensitive patients will also be allergic to cephalosporins, so it is essential to check for any documentation of allergies when assessing the patient. Diarrhoea is also a significant side-effect with this group of medicines.
Clavulanic acid
Clavulanic acid is a beta-lactamase inhibitor. Beta-lactamases are enzymes that are produced by some bacteria and are responsible for their resistance to beta-lactam antibiotics like penicillins (cephalosporins are relatively resistant to beta-lactamase). These antibiotics have a common element in their molecular structure: a four-atom ring known as a beta-lactam. The lactamase enzyme breaks the ring open, deactivating the molecule’s antibacterial properties.
Clavulanic acid itself has only a weak antimicrobial activity, despite sharing the β-lactam ring that is characteristic of beta-lactam antibiotics. However, when combined with a penicillin group antibiotic it gives the potential to overcome certain types of antibiotic resistance including resistance in bacteria that secrete beta-lactamase, and which otherwise would inactivate most penicillins. In its most common form, the potassium salt potassium clavulanate is combined with amoxicillin (co-amoxiclav, commercially known as Augmentin). Despite this, some bacterial strains have emerged that are resistant even to such combinations.
The use of clavulanic acid with penicillins is not risk-free however, and there has been an associated increased incidence of cholestatic jaundice and acute hepatitis during therapy or shortly after − in particular in men and those over the age of 65. The associated jaundice is usually self-limiting and very rarely fatal.
The UK Committee on Safety of Medicines (CSM) recommends that amoxicillin/clavulanic acid preparations be reserved for bacterial infections likely to be caused by amoxicillin-resistant β-lactamase-producing strains, and that treatment should not normally exceed 14 days.
Interference with protein synthesis
Protein synthesis takes place in the ribosomes. However, ribosomes are different in eukaryotes (i.e. our cells) than in prokaryotes (i.e. bacterial cells). This is another difference that can be exploited by antibiotic therapy.
Tetracyclines
This group of drugs acts by stopping bacterial cells from making essential proteins. The group includes tetracycline, oxytetracycline and minocycline. The spectrum of these medicines is wide and they are effective against both gram negative and gram positive bacteria.
Tetracyclines are usually given by mouth but can be administered by other routes. Absorption is better if they are given on an empty stomach as they can be absorbed erratically and this is not helped by the presence of food.
GI problems are probably the most common unwanted effect from this group of antibiotics. This is usually due to direct irritation by the medicine and also a decrease in the balance of normal intestinal bacteria (flora). Because they bind calcium, it is possible for tetracycline drugs to be deposited in growing bones and teeth. This can cause staining of teeth, underdevelopment of the teeth (hypoplasia) and bone deformities. For these reasons tetracyclines should not be given to children, pregnant women or nursing mothers.
As with other antibiotics many strains of micro-organisms have now developed resistance to this group, therefore making them less useful in clinical practice.
Chloramphenicol
This antibiotic is similar in action to the tetracycline group. It is a broad spectrum antibiotic which can be used against gram positive and gram negative organisms. It is rapidly and completely absorbed when given orally and reaches its maximum effect in the plasma in two hours. If necessary it can be given by other routes – for example, topically into the eye for conjunctivitis. The drug has a wide distribution in the tissues of the body including the cerebrospinal fluid, around the brain and spinal cord.
The most important unwanted effect of this drug is that it causes a severe depression of the bone marrow. This results in a fall in all blood cell elements. This side-effect is rare but can occur in low doses in some individuals. Chloramphenicol should only be given to babies with extreme caution as they do not have the capacity to metabolize and excrete the drug. This may result in a combination of signs and symptoms called ‘grey baby syndrome’ in which the baby vomits, has diarrhoea, is flaccid, has a low temperature and is ashen grey in colour. This syndrome carries a high mortality rate of 40 per cent. However the drug is given for certain acute or serious infections, for example gram negative bacteria which cause meningitis.
Aminoglycosides
This group of antibiotics includes gentamycin, streptomycin, tobramycin and neomycin and acts by inhibiting bacterial protein synthesis. Aminoglycosides are useful against both gram negative and gram positive organisms. However, these drugs are only bacteriacidal in the presence of oxygen. Therefore, bacteria that thrive in oxygen-poor environments (anaerobes) are only minimally affected. As with other groups the resistance of micro-organisms to these drugs is increasing all the time.
One of the most common drugs in this group is gentamycin. This is given by either the IV or IM route as it is not absorbed by the GI system. The drug has a fairly rapid half life of two to three hours, necessitating the dose being given three times daily. The main problem with this drug is its serious toxic effects. It can have a devastating effect on the apparatus in the inner ear (ototoxicity). This means that the patient may suffer damage to either their hearing or their ability to balance. The second major side-effect is damage to the kidney tubules (nephrotoxicity). This can be reversed if the drug is stopped.
Due to these major problems it is important that gentamycin is kept within a therapeutic range in the plasma. The plasma level half an hour following injection should be between 5 and 10mg per litre and the level just prior to injection should be 2mg per litre.
Macrolides
Erythromycin was the only drug in this group for many years. However, several new drugs have been developed that you may come across – for example, clarithromycin and azithromycin. As with the other antibiotics in this section macrolides inhibit protein synthesis in the bacterium.
Erythromycin destroys a similar range of micro-organisms as penicillin and is the first drug of choice if a patient has a penicillin allergy. The drug is mainly prescribed for gram positive organisms and spirochaetes. It has very limited success with gram negative organisms.
All drugs in this group can be given orally and they spread throughout most tissues of the body. They do not cross the BBB into the central nervous system and they do not penetrate synovial fluid. Macrolides possess different half lives which is why some are given more often in a day than others. They have an unusual action in that they are taken up and concentrated in phagocytic cells – the group of white cells responsible for digesting bacteria. Inside these phagocytic cells there are pockets of cell-destroying enzymes called lysosomes. Macrolides are absorbed into these pockets and therefore considerably enhance the phagocytic killing capacity of these cells.
Unwanted GI problems are the main issue when taking these medicines. If erythromycin is administered intravenously rather than orally, a degree of inflammation and damage to the vessel that the drug is entering (thrombophlebitis) can be expected.
Lincosamides
The drug of note in this group is called clindamycin. Its mechanism of action involves inhibition of protein synthesis in bacteria. It works against a range of organisms which include gram positive cocci and a range of anaerobic bacteria.
The drug can be given orally or by other routes and becomes well distributed in the body tissues, including bone. Like a number of other antibiotics it does not have the capacity to cross the BBB. The usual dose is 150mg four times daily.
Unwanted effects are mainly GI in nature and the patient may suffer from diarrhoea. In rare cases this may become life-threatening as they develop a condition called pseudomembranous colitis. This is an acute inflammation of the colon caused by toxins released from micro-organisms that are resistant to clindamycin; an example would be infection with a bacteria called clostridium difficile.
Inhibition of bacterial DNA
You will be aware from your non-stop reading of anatomy and physiology texts that DNA stands for deoxyribonucleic acid, which is found in all living cells and carries the organism’s genetic information. In bacteria this information is what we call supercoiled. Some writers have likened this to putting 15 metres of cotton material into a matchbox. In order for the bacteria to survive through replication this information needs to be copied. To do this an enzyme is needed to uncoil parts of the supercoiled material. The enzyme that brings this about in the bacterial cell is called topoisomerase II. A group of antibiotics called fluoroquinolones affect the ability of the bacteria to use topoisomerase II.
Fluoroquinolones
The most common antibiotic in this group is called ciprofloxacin, which is a broad spectrum antibiotic. It is useful as it is effective against micro-organisms that have become resistant to penicillins, cephalosporins and aminoglycosides. This drug can be given orally and is well absorbed. It enters many tissues and particularly concentrates in the kidneys, prostate gland and lungs, making it ideal for fighting infection in these areas of the body.
Unwanted effects are not frequent, usually mild in nature and disappear rapidly once the drugs have been stopped. In the main, GI problems like diarrhoea are reported. Sometimes people also complain of developing a skin rash, headaches and dizziness. One of the main interactions with this drug develops if it is given to asthmatic patients who are receiving a drug called theophylline. The ciprofloxacin inhibits enzymes in the liver that are normally responsible for the metabolism of theophylline. This results in a build up of theophylline in the plasma, eventually reaching toxic proportions.
One of the foremost concerns in modern medicine is antibiotic resistance. Simply put, if an antibiotic is used long enough, bacteria will emerge that cannot be killed by that antibiotic. Infections exist today that are caused by bacteria resistant to some antibiotics, and existence of antibiotic-resistant bacteria creates the danger of life-threatening infections that don’t respond to antibiotic treatment.
There is an alarming rise in the occurrence of antimicrobial resistance. For example, Staphylococcus aureus is a prevalent bacterium carried by humans that can cause a number of problems, from mild skin infections to serious diseases including food poisoning, wound infections, pneumonia and toxic shock syndrome. In 2002, the WHO reported that more than 95 per cent of this bacterium worldwide is resistant to penicillin, and 60 per cent to its derivative methicillin.
Causes of antibiotic resistance
Misuse of antibiotics occurs in medicine, agriculture and household products. Common examples include erroneous antibiotic prescriptions for non-bacterial infections and the addition of antibiotics to livestock feed and cleaning agents, which have helped create a reservoir of antibiotic-resistant bacteria.
Sometimes irregular combinations of bacteria have perpetuated drug-resistant microbes. One example was when staphylococcus aureus was shown to develop vancomycin resistance genes through cohabitation with the vancomycin-resistant bacteria, enterococcus faecalis, in the wound of a hospitalized patient. Through mechanisms of genetic exchange between bacterial species, the mere coexistence of these two particular bacteria helped to bring about drug resistance in the staphylococcus aureus.
Enhanced transmission of resistance factors, or the increased efficiency with which resistance genes are exchanged, is another important way that antibiotic resistance is perpetuated. Factors that contribute to enhanced transmission include the survival of patients with chronic disease, an increased number of immunosuppressed individuals, substandard hospital hygiene, more international travel and budget cuts in health care administration.
Profit also has a role to play in the development of drug resistance. The pharmaceutical industry has increasingly been busy with hugely profitable ‘blockbuster’ drugs for allergies and depression, and ‘lifestyle’ drugs for conditions such as baldness and impotence. This has led to decreased antibiotic and vaccine research and development.
In many cases, drug-resistant bacteria have been met with antibiotics that are nothing more than replicas of earlier drugs. There is an urgent need for new avenues of therapeutic treatment, and a new era of prophalytic (preventative) treatment has now begun.
Issues with neonates and children
Antibiotic misuse is most likely to occur in children with ear infections (otitis media), the number one reason a child is brought to a doctor. Antibiotic therapy is the most common treatment of ear infections, with amoxicillin being the first choice. The side-effects of amoxicillin include upset stomach, diarrhoea, allergic reactions and nappy rash.
Research suggests that when antibiotics are used at the beginning of an ear infection, the frequency of recurrence may be almost three times greater than if antibiotics are delayed or not used (AHRQ (2000)). Antibiotics do not just go after the pathogenic or ‘bad’ bacteria. They also destroy the beneficial bacteria necessary and vital to good health. Among the more important beneficial bacteria are lactobacillus acidophilus and bifidobacterium bifidus. They help protect the body against infection. Depleting these organisms can disrupt the balance of the body and lead to increased susceptibility to infection by fungi, bacteria, viruses and parasites. Additionally, when antibiotics are used excessively, depleting the beneficial bacteria, there may be an overgrowth of yeast in the body. This may lead to candida infection (thrush).
Children are growing and therefore require adequate nutrition; however, antibiotics adversely affect many nutrients, particularly those needed by the immune system to fight infection, such as vitamins A and C. One of the most common side-effects of antibiotics is diarrhoea. This causes a loss of nutrients, especially magnesium and zinc, which are important in growth and repair.
Sweeteners, dyes, flavourings and other additives are found in antibiotics prescribed to children. These may include saccharin, sucrose and red dye. Some dyes may be reactive with medicines such as aspirin and paracetamol, which are commonly given to a child during an illness. Even tiny amounts of the chemical additives in antibiotics can cause an allergic reaction in a sensitive child.
Drugs used to treat tuberculosis
Despite hopes that tuberculosis (TB) might be eradicated from the UK, in recent years there has been an increase of the disease in this country and it is not uncommon to be nursing someone suffering from TB.
TB is usually caused by inhaling the mycobacterium tuberculosis organism. This bacteria has a very tough envelope and can survive for long periods in dry conditions. This coating also protects the organism, making it resistant to destruction by the body’s natural defences. The bacterium can invade and survive within our phagocytic cells. The damage to our tissues is usually due to the body’s inflammatory response to the infection rather than the result of any toxin released by the organism.
Initial infection of the lungs is called primary TB. The bacteria is engulfed by phagocytic cells in our lungs. These cells attempt to communicate with T lymphocytes which attempt to resist the infection but the increase in phagocytic cells at the site of infection is relatively ineffective. Instead, more and more of the phagocytic cells become infected by the bacteria and are carried into the lymphatic system where they eventually reach what is known as the hilar lymph nodes within the lungs.
The body manages to ‘wall off‘ these infected phagocytes by creating pockets which are known as tubercles. These are balls of infection with a necrotic (dead) centre surrounded by infected phagocytic cells wrapped in a capsule of collagen (protein) fibres. These tubercles may then remain in the lungs but the patient suffers no further symptoms of the disease.
The tubercles are now little time bombs ready to explode. If the person’s immune system becomes compromised the condition is activated again from its dormant state. Reactivation may take place under a number of circumstances − for example, poor nutrition, the age of the patient and lowered immune system.
This reactivation is called secondary TB. The lung tissue itself now becomes necrotic, creating large cavities. As with the tubercles, these cavities remain encapsulated by connective tissue and may lie dormant or become reactivated once again.
Miliary TB is a condition in which the patient cannot make an adequate response to the initial infection. This leads to weight loss, extreme tiredness (lethargy) and coughing. The organism is now invading the blood and sets up camp in a variety of tissues including the lungs, meninges, spleen, liver and bone marrow. If this is not treated, death ensues. It is with this in mind that we will now look at the treatment of TB. First line drugs will be discussed and include isoniazid, rifampicin and pyrazinamide.
Isoniazid
This drug is specific against mycobacteria and is therefore very helpful in the treatment of TB. It is bacteriostatic when the organisms are not active, but becomes bacteriocidal when they start to divide and multiply. The drug diffuses through cells and crosses the BBB into the cerebrospinal fluid. This point is important as it penetrates well into the tubercles described earlier.
The normal dose for an adult is up to 300mg per day and is usually given as a tablet. Some people break down this drug rapidly in the liver and some do not. The latter group tend to have a better therapeutic response as the drug manages to reach a more constant level in the plasma.
Side-effects are related to the dose given, the commonest being skin problems. Patients who metabolize isoniazid more slowly are more at risk of side-effects if they are dosed too often. Isoniazid affects enzymes in the liver that break down certain anti-convulsant drugs. Phenytoin, ethosuximide and carbamazepine can all be increased in the plasma if given with isoniazid.
Rifampicin
Rifampicin acts by interfering with a substance called ribonucleic acid (RNA) in the bacteria so affecting protein synthesis within the organism. This antibiotic has a broad range of activities and is effective against both gram positive and gram negative organisms. It is the most active agent in the fight against TB to date. It has the ability to get right inside the phagocytic cells that have ingested the tubercle bacillus. Once inside, it can destroy the tubercle bacillus at will.
The drug is well absorbed by the GI system and therefore is given in tablet form, usually in a dose of between 450 and 600mg daily prior to eating breakfast. It is able to gain entry to a wide group of tissues and fluids.
Unwanted effects are not common. Some patients may suffer skin problems, a raised temperature and GI upsets such as nausea and diarrhoea. Liver damage, with a yellow discoloration of the skin (jaundice), whites of the eyes (sclerae) and mucous membranes has been reported and can prove fatal.
As with isoniazid, rifampicin affects enzymes in the liver that help to break down certain drugs. Rather than inhibiting the pathways, rifampicin induces them. In other words, drugs such as warfarin, glucocorticoids, opiates, oral hypoglycaemic agents and oestrogen are all broken down more rapidly. This means dosing needs to be adjusted accordingly.
Finally, you will find that rifampicin is often given alongside other antibiotics to combat TB. This is in order that we do not give the organism the opportunity to develop resistance. As this is the most active treatment the last thing we want to do is render it useless.
Pyrazinamide
Pyrazinamide is well absorbed orally and becomes widely distributed in the tissues and fluids of the body. It penetrates well into the meninges so is particularly useful if the disease spreads into this area.
Pyrazinamide works in a similar way to rifampicin in that it gains entry to the phagocytes that have ingested the bacteria and destroys it. Side-effects include the raising of plasma uric acid levels, so causing gout. GI symptoms and a raised temperature have also been reported. Liver failure is also a possibility especially if the drug is given in high doses. However, high doses are uncommon as a combination of drugs is the preferred technique in treating the organism (see above). Liver function tests should, however be carried out prior to drug commencement.
Viral disease
Viruses are very different from bacteria. They are a lot smaller and essentially have a core of either DNA or RNA surrounded by a coat of protein (capsid). The coat plus its contents are referred to as the nucleocapsid. Some viruses are even more protected in that they have developed a further coat of phospholipids from the host cell (the cell in which virus lives), and some of the viruses own glycoproteins.
At some point in their lifetime, everyone in the world will have been infected by a virus. Conditions such as chickenpox, shingles, conjunctivitis, warts, measles, mumps and rubella are all caused by viral infections.
Viral mechanisms
A virus is basically a type of parasite that gets into a cell and then uses the cell’s machinery for its own purposes. Viruses do not have the ability to reproduce and replicate themselves so they have to borrow these mechanisms from their host cell. Certain viruses also carry the mechanisms to reproduce (replicate) inside the host cell without using the host cell’s machinery to help them. This particle of potential infection is called a virion.
The virus gains access to the cell by locking onto a receptor that carries out some normal activity. The virus is then taken into the interior of the cell by a process of endocytosis. Basically, the cell swallows the infective virus and allows it to enter the cytoplasm. Once inside the host cell the nucleic acid centre of the virus starts to use the host cell’s machinery to help it replicate more of its kind (viral replication). This can take various forms depending on the type of virus.
Some viruses are called DNA viruses. This means that they replicate by latching into and becoming part of the host cell’s DNA. Once they have achieved this they can direct the manufacture of more viruses. Other viruses are called RNA viruses and use the host’s RNA, linking with the viral RNA code so that the cell manufactures the proteins that go into building new viruses within the cell. Finally, retroviruses work by copying a viral blueprint onto a piece of DNA. This viral DNA is then linked into the host’s DNA and so the host starts creating new viruses as part of its normal activity.
Compared to bacterial treatment with antibiotics it is very difficult to produce antiviral drugs because viruses live within our own cells. Once inside, they can also switch off mechanisms for their detection, along with the self-destruct mechanisms that our cells contain. This leads to a very slippery customer indeed when trying to develop treatment. A further problem in dealing with viruses is that by the time the body has recognized it has been invaded, a large amount of the virus has been manufactured.
Human immunodeficiency virus
This virus causes acquired AIDS, which is a growing problem in some parts of the world. The worst affected area is sub-Saharan Africa. In the UK in the 1980s the number of people with HIV diminished, some argue due to large television campaigns informing the population about the disease. However, the incidence levels in many sexually transmitted diseases (STDs) including HIV and AIDS are on the increase, in particular with men and women in the older age range.
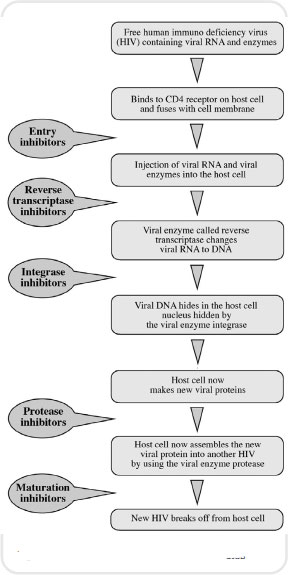
HIV is the result of the invasion of a particular lymphocyte called a helper T cell (T4 cells). These cells are very important in defending the body and are linked to the immune response. Once the person has been infected with the virus it can be transmitted to other people in a variety of ways: through sexual intercourse, blood or transplanted organs and tissues, from an infected mother to her foetus and by breastfeeding.
HIV may remain dormant within the body for many years and most people are quite unaware that they have contracted the disease. However, it is possible by blood testing to confirm within a few weeks of infection whether the person has acquired the virus. The time taken for this ticking bomb to explode in terms of loss of immune response in the individual varies from months to years. An average time from diagnosis of HIV to death from AIDS is about two years in an untreated patient.
The virus targets cells with certain receptors on their surface. Examples of these cellular ‘name badges’ are CD4 and CCR5. The virus attaches itself to receptors on these cells and is taken in. Once inside it works on the principles of a retrovirus. In other words, it produces its own DNA by using a viral enzyme and then embeds the viral DNA into the host’s DNA. The host cell then begins to make proteins which will be made into new viruses. These will then eventually leave the cell and gain access to cells of their own by recognizing the ‘name badges’ on them. As the cells divide the integrated viral DNA also divides and becomes part of the new cell. This is called proviral DNA. It effectively means that any helper T cell on division passes on the ability of the daughter cells to produce more viruses.
Antiretroviral therapy
Antiviral therapy is aimed at using a combination of agents that act at different points in the replication of the virus within the human cell. One of the main reasons for using a combination of drugs is to delay the onset of resistance in any one of the therapies. Currently, antiviral drugs used in the treatment of AIDS fall into two broad categories: reverse transcriptase inhibitors and protease inhibitors. We will now focus on each of these drug classes.
Nucleoside reverse transcriptase inhibitors
Reverse transcription is the second phase in the HIV life cycle. HIV genes are carried on two strands of RNA; however, in order to enter the nucleus of a human cell the virus must change the genetic code into a strand of DNA. It does this by using a viral enzyme called reverse transcriptase. Nucleoside reverse transcriptase inhibitors are designed to block the action of reverse transcriptase.
Some examples of drugs from this class are zidovudine, abacavir and lamividine. All may be given orally but there are some differences in the frequency of administration. Zidovudine and abacavir have short half lives and lamividine has a long half life which affects dosing. All these drugs diffuse through a range of tissues, however, zidovudine achieves the best concentration in the cerebrospinal fluid, about 65 per cent of that which it achieves in the plasma.
Adverse reactions to this family of drugs are not pleasant. Zidovudine can cause bone marrow depression leaving the patient open to all types of infection. Abacavir may cause hypersensitivity reactions including rashes and high temperatures. Lamividine in comparison has only mild side-effects such as headaches and some GI symptoms.
Non-nucleoside reverse transcriptase inhibitors
These drugs have the same effect as the nucleoside reverse transcriptase inhibitors but have a different method of achieving the response. Quite often, you will find both types of drugs being given alongside each other. There are two main drugs in this family: nevirapine and efavirenz.
Both are given orally. Nevirapine is 100 per cent bioavailable compared to efavirenz which is between 50 and 60 per cent bioavailable. The half lives of nevirapine and efavirenz, compared with their relatives, are considerably longer. Both drugs have elimination half lives of between 30 and 40 hours.
The main adverse affect of nevirapine is the development of a rash. This occurs in up to 20 per cent of patients taking the drug. Other common side-effects are headaches, a high temperature and lethargy. Efavirenz has similar problems in that about 25 per cent of people taking it will develop a rash. This drug may also lead to disorientation and lack of concentration.
Protease inhibitors
If the viral RNA manages to make a copy of its genetic blueprint onto DNA, then this is carried into the nucleus of the human cell. Here, another viral enzyme called integrase joins the viral DNA onto the human DNA, and hides it. Then, when the cell tries to make new proteins, it also makes new viral proteins. A new class of drugs is currently being developed that will be aimed at blocking the actions of integrase.
Eventually, these proteins are assembled into new HIVs in the endoplasmic reticulum and golgi apparatus of the cell. This assembly-line relies on an enzyme called protease to cut the proteins into either functional units of the virus or viral enzymes.
Protease inhibitors block this stage of viral replication in the cell. Examples of current protease inhibitors are saquinavir and indinavir (there are six inhibitors currently available in the UK). All these drugs are given orally, however saquinavir is subject to metabolic breakdown by an extensive first pass effect. In terms of distribution, cerebrospinal fluid levels are very low with saquinavir whereas with indinavir they rise to 76 per cent of that which the drug achieves in the plasma.
All these drugs cause GI disorders and endocrine disturbances such as insulin resistance, high blood sugar levels and hyperlipidaemia. These symptoms are not good news if you happen to be diabetic and have HIV.
All the drugs in this family also cause enzyme inhibition, especially to pathways which break down benzodiazepines. Therefore, the concentration of these drugs will rise if given together with protease inhibitors.
The combination of drugs now given for HIV has dramatically improved the prognosis (see Figure 4.2). This has obviously had a lessening effect on AIDS cases and deaths in industrialized countries. However, as noted above, in many developing countries cases of both disease processes continue to rise in number.
< div class='tao-gold-member'>