43
Antifungal Agents
This chapter will be most useful after having a basic understanding of the material in Chapter 57, Antifungal Agents in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. In addition to the material presented here, the 12th Edition contains:
• Structural formulas for each of the antifungal agents in addition to the figures reproduced here
• Table 57-1 Pharmacotherapy of Mycoses which lists the drugs used for different mycoses
• Table 57-7 Pharmacokinetics of Echinocandins in Humans which shows the pharmacokinetic differences among caspofungin, micafungin, and anidulafungin
DRUGS INCLUDED IN THIS CHAPTER
• Amphotericin B (FUNGIZONE); colloidal dispersion (AMPHOTEC, AMPHOCIL); liposomal formulation (AMBISOME); lipid complex (ABELCET)
• Anidulafungin (ERAXIS)
• Butenafine (MENTAX, LOTRIMIN ULTRA)
• Butoconazole (FEMSTAT 3, others)
• Caspofungin (CANCIDAS)
• Ciclopirox olamine (LOPROX, others)
• Clotrimazole (LOTRIMIN, MYCELEX, GYNE-LOTRIMIN, others)
• Fluconazole (DIFLUCAN, others)
• Flucytosine (ANCOBON)
• Griseofulvin (GRIFULVIN and GRIS-PEG)
• Haloprogin (HALOTEX)
• Isavuconazole (BAL 8557) (investigational)
• Itraconazole (SPORANOX, others)
• Ketoconazole (NIZORAL, others)
• Micafungin (MYCAMINE)
• Miconazole (MICATIN, ZEASORB-AF, MONISTAT 7, MONISTAT 3, MONISTAT 1, others)
• Naftifine (NAFTIN)
• Nystatin (MYCOSTATIN, NILSTAT, NYOTRAN, others)
• Oxiconazole (OXISTAT)
• Posaconazole (NOXAFIL)
• Sertaconazole (ERTACZO)
• Sulconazole (EXELDERM, SULCOSYN)
• Terbinafine (LAMISIL, others)
• Terconazole (TERAZOL, others)
• Tioconazole (VAGISTAT 1, others)
• Tolnaftate (AFTATE, TINACTIN, others)
• Undecylenic acid (DESENEX, others); Calcium undecylenate (CALDESENE, CRUEX)
• Voriconazole (VFEND)
• Whitfield’s Ointment
LEARNING OBJECTIVES
 Understand the mechanisms of action and resistance of antifungal agents.
Understand the mechanisms of action and resistance of antifungal agents.
 Describe the therapeutic uses of antifungal agents in the context of treatment for fungal diseases.
Describe the therapeutic uses of antifungal agents in the context of treatment for fungal diseases.
 Develop knowledge of the common and unique toxicities of antifungal agents.
Develop knowledge of the common and unique toxicities of antifungal agents.
 Understand the drug–drug interactions that can occur with the use of azole antifungal agents.
Understand the drug–drug interactions that can occur with the use of azole antifungal agents.
 Know the differences in treating invasive fungal infections with systemic drugs versus superficial infections with topical antifungal agents.
Know the differences in treating invasive fungal infections with systemic drugs versus superficial infections with topical antifungal agents.
MECHANISMS OF ACTION AND RESISTANCE OF ANTIFUNGAL DRUGS
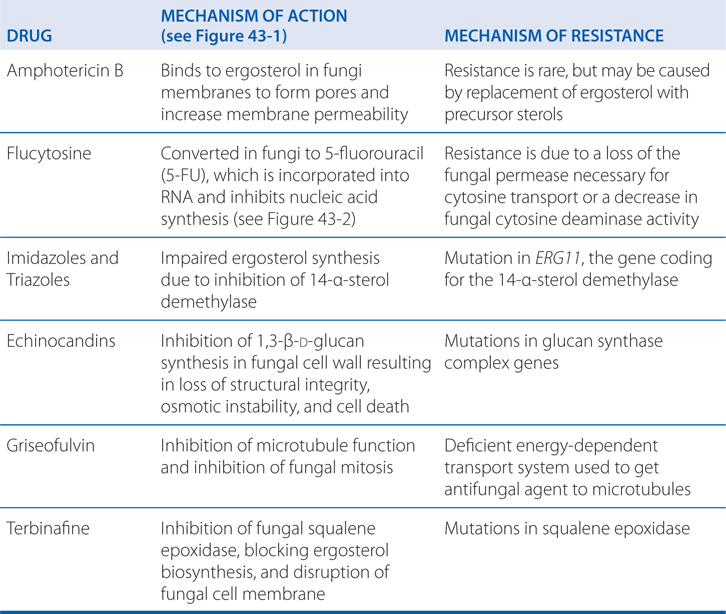
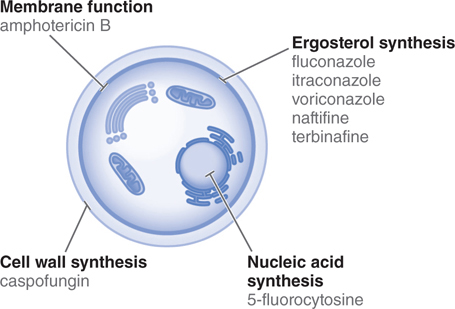
FIGURE 43-1 Sites of action of antifungal drugs. Amphotericin B and other polyenes, such as nystatin, bind to ergosterol in fungal cell membranes and increase membrane permeability. The imidazoles and triazoles, such as itraconazole and fluconazole, inhibit 14-α-sterol demethylase, prevent ergosterol synthesis, and lead to the accumulation of 14-α-methylsterols. The allylamines, such as naftifine and terbinafine, inhibit squalene epoxidase and prevent ergosterol synthesis. The echinocandins, such as caspofungin, inhibit the formation of glucans in the fungal cell wall.
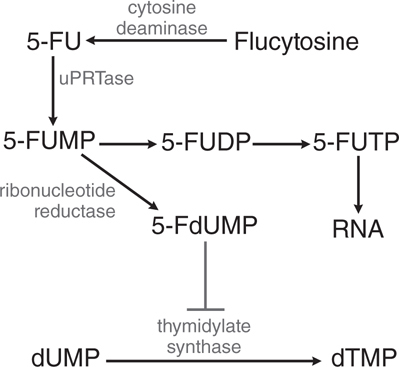
FIGURE 43-2 Action of flucytosine in fungi. Flucytosine is transported by cytosine permease into the fungal cell, where it is deaminated to 5-fluorouracil (5-FU). The 5-FU is then converted to 5-fluorouracil-ribose monophosphate (5-FUMP) and then is either converted to 5-fluorouridine triphosphate (5-FUTP) and incorporated into RNA or converted by ribonucleotide reductase to 5-fluoro-2’-deoxyuridine-5’-monophosphate (5-FdUMP), which is a potent inhibitor of thymidylate synthase. 5-FUDP, 5-fluorouridine-5’-diphosphate; dUMP, deoxyuridine-5’-monophosphate; dTMP, deoxythymidine-5’-monophosphate.
A 56-year-old woman is diagnosed with mucormycoses involving the maxillary sinuses. An infectious disease consultant recommends that she be treated with amphotericin B.
a. What different formulations of amphotericin B are available for her treatment?
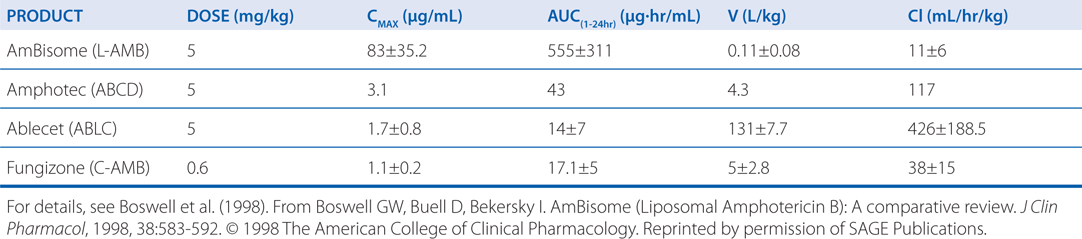
There are currently 4 formulations of amphotericin B commercially available: conventional amphotericin B (C-AMB), liposomal amphotericin B (L-AMB), amphotericin B lipid complex (ABLC), and amphotericin B colloidal dispersion (ABCD). Table 43-1 summarizes the pharmacokinetic properties of these different preparations.
TABLE 43-1 Pharmocokinetic Parameters for Amphotericin B Formulations after Multiple Administrations in Humans
b. What are the major differences in these formulations?
C-AMB is insoluble in water, but is formulated for intravenous use by complexing it with the bile salt, deoxycholate. ABCD forms a colloidal solution when dispersed in water and provides much lower blood concentrations than C-AMB. Infusion reactions of chills and fever are more common with ABCD than with C-AMB. L-AMB is supplied as a lyophilized powder and has equivalent blood concentrations as C-AMB. L-AMB is approved for empirical therapy of fever in the neutropenic host not responding to appropriate antibacterial agents, as well as for salvage therapy of aspirgillosis and candidiasis. ABLC provides blood concentrations of amphotericin B that are much lower than with the same dose of C-AMB. ABLC is approved for salvage therapy of deep mycoses.
The lipid formulations appear to reduce the risk of nephrotoxicity during therapy. The cost of the lipid formulations of amphotericin B greatly exceeds that of C-AMB.
c. What is the mechanism of action of amphotericin?
The anitifungal activity of amphotericin B depends principally on its binding to a sterol moiety, primarily ergosterol, in the membrane of sensitive fungi. By virtue of their interaction with these sterols, polyenes, appear to form pores or channels that increase the permeability of the membrane, allowing the outward leakage of a variety of small molecules (see Figure 43-1).
d. What untoward effects should be watched for in this patient?
Major untoward effects of amphotericin B are infusion-related reactions such as fever and chills. These are most severe with ABCD, slightly less with C-AMB, even less with ABLC, and least with L-AMB.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree