Blood clotting is a normal homeostatic mechanism, the purpose of which is to prevent the loss of blood from the cardiovascular system and to ensure that blood vessels remain intact. This mechanism works very well in preventing haemorrhage from smaller blood vessels (e.g. capillaries, arterioles and venules). However, the mechanism is overwhelmed if bleeding occurs from the large vessels such as major veins or arteries. If such bleeding occurs, interventions from a first aid, medical or surgical perspective have to be employed in order to control the bleeding.
The word used for stopping haemorrhage from the body is haemostasis and, as stated above, is a normal homeostatic function of the body. The blood and damaged blood vessels have the ability to release components which work together to form a plug of solid matter which blocks the tear in the blood vessel. Haemostasis is divided into four processes, which will now be outlined.
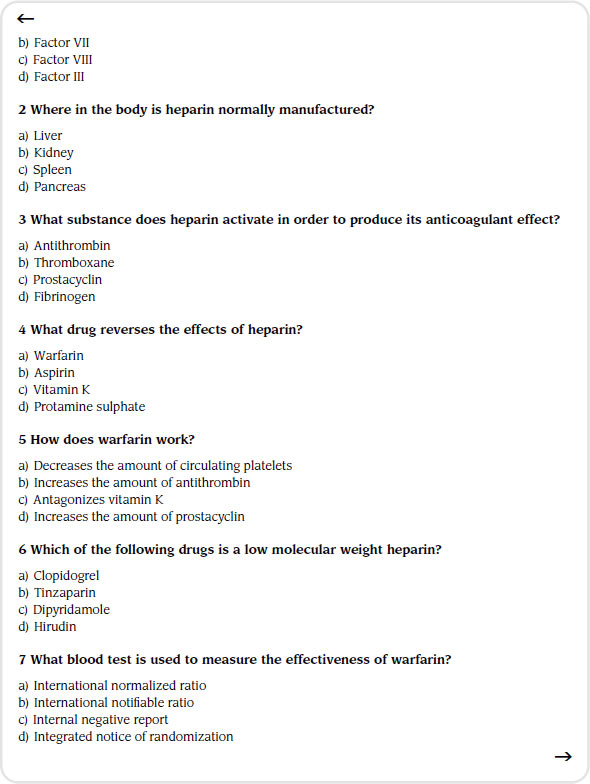
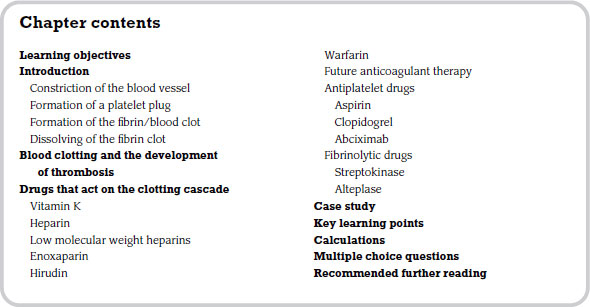
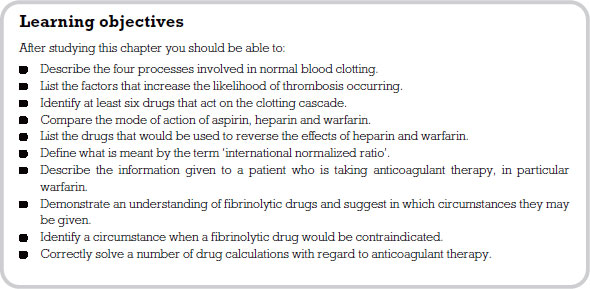
Constriction of the blood vessel
Following the tearing of a blood vessel, the body reflexively constricts the size of the vessel, which also leads to the contraction of the severed ends. The constriction of vessels spreads to affect other local small vessels. The blood flow through these small vessels is now reduced and this allows the platelets and the plasma to come into contact with the damaged area of the blood vessel. When this occurs the body is setting in motion a state of events, the first being a reduction in the likelihood of the plug of platelets being washed away.
Formation of a platelet plug
Damage to the wall of a blood vessel exposes proteins within the vessel wall. These are collagen and elastin fibres and lie underneath the thin inside layer of the vessel. The exposure of these important proteins causes platelets to adhere to the site of the injury. Adhesion of the platelets to themselves and the site of the injury is further helped by one of the plasma clotting factors called factor VIII.
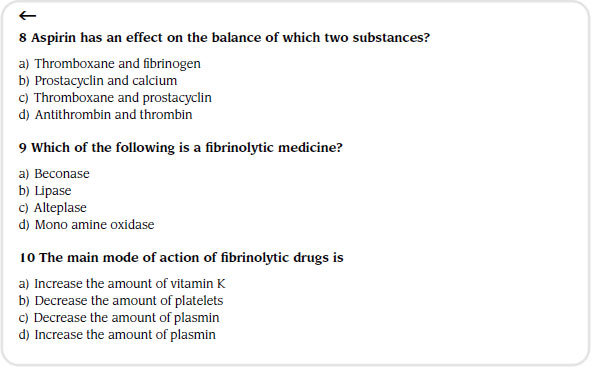
The process of platelet adhesion is reversible up to a point. Once the platelets have released the granules which they contain, white blood cells begin to stick to the platelets. During this build up of the foundation of the clot, the platelets also release a substance known as thromboxane (TXA2). This has two effects: first, it increases the ability of the cells to stick together; second, it makes the blood vessel smaller by vasoconstriction. At this point it should be noted that the cells that have been exposed under the intima lining of the blood vessels start to produce a substance known as prostacyclin. This works in the opposite way to thromboxane in that it stimulates vasodilation and stops the process of the cells sticking together. This is an important point as certain drugs are given to affect the balance between thromboxane and prostacyclin (e.g. Dipyridamole).
As the platelet cells continue to stick together, they release a platelet factor which acts as a platform on which various blood clotting factors can bind. The foundation is now secured for the next process to begin.
Formation of the fibrin/blood clot
The essential end point of this process is an insoluble protein called fibrin which will plug the tear in the vessel wall. Insoluble fibrin lays down a mesh of white fibres which stick to each other and to tissue cells. This mesh traps other blood cells and more platelets. The clot gradually constricts, squeezing out any serum and leaving a solid but elastic plug.
To get to this end point, the blood and platelets have to go through a complex chain reaction. Each phase of this reaction is brought about by what are called ‘plasma clotting factors’ (always referred to using Roman numerals: see Table 6.1).
Table 6.1 Plasma clotting factors
| Factor | Name |
| I | Fibrinogen |
| II | Prothrombin |
| III | Tissue factor or thromboplastin |
| IV | Calcium |
| V | Proaccelerin (labile factor) |
| VII | Proconvertin (stable factor) |
| VIII | Antihaemophilic factor A Antihaemophilic globulin |
| IX | Antihaemophilic factor B Plasma thromboplastin component Christmas factor |
| X | Stuart-Prower factor |
| XI | Plasma thromboplastin antecedent Haemophilia C Rosenthal syndrome |
| XII | Hageman factor |
| XIII | Fibrin stabilizing factor Laki-Lorand factor |
This cascade of events can be triggered in two distinct ways. First, damaged cells release a substance called thromboplastin or factor III. As thromboplastin is not part of the blood, this blood clotting pathway is known as the extrinsic pathway. The extrinsic pathway is therefore triggered by events such as physical injury to the blood vessels. The second triggering mechanism comes from contact of the blood with exposed collagen fibres, which are not usually exposed as they lie under the inner surface of the blood vessel. However, if damage occurs to this delicate lining, collagen fibres come into contact with blood products and the clotting mechanism commences. This particular set of events is known as the intrinsic pathway. The triggering of the extrinsic pathway would come from pathological states such as atherosclerosis (fatty deposits being laid down in the walls of arteries).
The key step in both systems is activation of a plasma factor called factor X. These systems work together to ensure that the body produces large enough amounts of thrombin to be effective in stemming blood loss.
A point to remember here is that the blood is thought to contain natural inhibitors of the clotting factors. It is these inhibitors that are believed to stop widespread clotting from taking place, therefore localizing events. The best known of these natural anticoagulants is antithrombin III.
Dissolving of the fibrin clot
Dissolving of a clot takes place much more slowly than does the building of one and the slow removal of the clot is part of life’s normal process. Fibrin is dissolved by a substance known as plasmin. This product is not normally present in the plasma but is derived from an inactive protein called plasminogen. Plasminogen can be activated by a number of triggers, for example, plasma clotting factor VII, red, white and certain renal cells. The body has natural plasmin inhibitors, such as antiplasmin. These ensure that widespread destruction of fibrin does not take place.
Blood clotting and the development of thrombosis
Thrombosis is the formation of a clot in a vessel within the cardiovascular system, which relates to or arises from a disease process. There are three factors that increase the likelihood of thrombosis occurring:
1. injury to the vessel wall;
2. altered blood flow;
3. increased likelihood of the blood to clot.
For example, people who have developed fatty plaques, who are physically immobile or who are being treated with certain contraceptives are more at risk of developing thrombosis. Thrombosis can occur in both arteries and veins. In arteries the clot is usually associated with a build up of fatty plaques (atherosclerosis) and has a large platelet component. Veins, in contrast, are usually associated with slow flow of blood through the vessels and there is a large fibrin component. Due to the make-up of the venous thrombosis, the clot has a large jelly-like tail that floats in the vessel. If this breaks off, it becomes what is known as an embolus. This embolus may then lodge in smaller vessels, causing death of tissue.
There are three categories of drugs that affect blood clotting and the formation of thrombosis:
1. drugs that affect fibrin formation;
2. drugs that affect platelet function;
3. drugs that affect dissolving of the clot.
Drugs that act on the clotting cascade
Drugs in this category can be used to manipulate the cascade system when there is a defect in the process of clotting, or when there is an unwanted coagulation taking place.
Fortunately, deficiencies in clotting factors rarely happen. However, two examples need to be mentioned here: haemophilia A, caused by lack of factor VIII and ‘Christmas’ disease or haemophilia B, caused by lack of factor IX or the ‘Christmas’ factor (named after Stephen Christmas, the first patient to be diagnosed). These missing factors can be replaced by either giving fresh plasma or giving concentrated preparations of factors VIII and IX. Other problems that lead to an inability of the cascade mechanism to produce clotting are acquired. These tend to be more common in origin and include liver diseases, vitamin K deficiency (especially in neonates) and excessive oral anticoagulants being prescribed. These three situations require the person to be given treatment by administering vitamin K.
Vitamin K
This vitamin is named after ‘K’ for ‘Koagulation’ in the German language. It occurs naturally in plants and is essential for the plasma clotting factors we discussed earlier. It is particularly important for formation of factors II, VII, IX and X.
Naturally occurring vitamin K or phytomenadiole can be given by mouth or by IV infusion. If it is given orally its absorption will rely on the person’s digestive system being normal so that what are known as bile salts are being produced and excreted into the duodenum. However, if this is not the case, such as in obstructive jaundice, a synthetic preparation is available that does not require these bile salts in order to be absorbed into the body. This drug is known as menadiol sodium phosphate. Vitamin K is used clinically in a range of situations, for example, overdose with warfarin, in babies to prevent haemorrhagic disease and in diseases which cause vitamin K deficiency.
Heparin
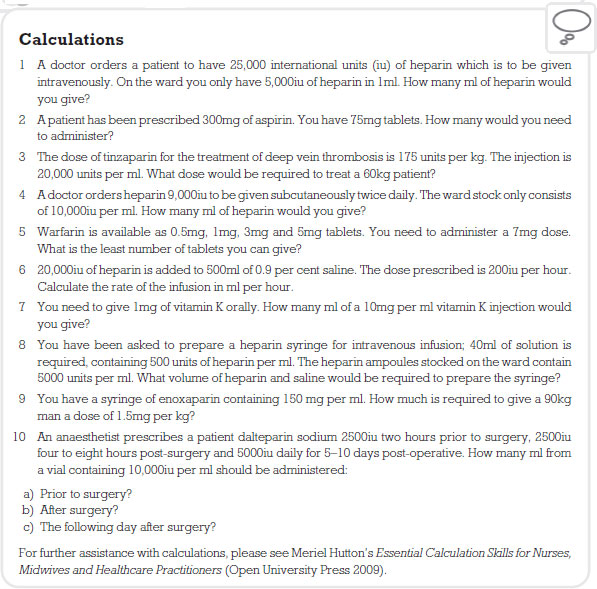
Heparin is a complex protein and is found in the liver and mast cells. It is a powerful anticoagulant but is broken down by digestive enzymes; therefore, it is given by IV infusion. Heparin leads to anticoagulation of blood both inside and outside the blood vessels. It works by activating antithrombin III. As you will remember, we discussed the role of this in the section on formation of the fibrin clot. Antithrombin III is a naturally occurring anticoagulant in the body and heparin accelerates its rate of action significantly. This in turn stops the cascade at the thrombin stage, so inhibiting the fibrinogen to fibrin stage of blood clotting from taking place.
Heparin acts immediately following IV administration and its elimination half life is approximately 40 to 90 minutes. In emergency situations, therefore, it is usually given by a bolus dose, followed by a constant rate infusion via a pump mechanism. It is important that the patient is not given too much heparin or they will haemorrhage. A special blood test is performed so that this does not happen. The appropriate blood examination is called an activated partial thromboplastin time test. This test will monitor the effects of heparin on blood clotting. Basically, the test measures in seconds how long it takes the blood sample to clot. The dose of heparin is adjusted so that a value of 1.5–2.5 times the normal sample is achieved.
A rare complication of heparin is a decrease in the amount of circulating platelets (thrombocytopenia). The patient’s platelet count should be ascertained if they remain on the therapy for more than five days. Osteoporosis has been reported in people who have been receiving long-term administration of heparin, although why this occurs is not understood.
Low molecular weight heparins
These are relatively new additions to the anticoagulant drugs available. Basically, they are heparin but broken into smaller parts. This has significant advantages: for example, these drugs are more predictable than their larger cousin, which means that blood tests such as the activated partial thromboplastin time test do not need to be monitored and the dosage does not need to be adjusted. Since this group of drugs can be given satisfactorily by a SC and usually twice-daily route, the need to bring patients into hospital for treatment has been removed. Many of them are treated on an outpatient basis from nurse-led clinics which is far more cost effective.
Low molecular weight heparins can be given to lessen the risk of thrombosis development post-surgery (prophylaxis). The drug is given via the SC route twice a day until the patient is able to mobilize well. It is effective in treating deep vein thrombosis and pulmonary embolism and as the drug does not cross the placental barrier can be used safely in pregnancy. Examples of drugs in this group are Tinzaparin, Enoxaparin, Dalkeparin and Certoparin. Bleeding can occur, but these drugs are less likely than heparin to cause thrombocytopenia.
Enoxaparin
You will come across this medicine under the trade name of Clexane. The medicine in the UK is indicated in six recognized situations, among them stopping thromboembolism post-operatively.
Enoxaparin binds to and accelerates the activity of antithrombin III. By activating antithrombin III, it speeds up the inhibition of coagulation factors Xa (Stuart-Prower) and IIa (prothrombin), where ‘a’ stands for ‘activated’. The anticoagulant effect of enoxaparin can be directly mirrored to its ability to inhibit factor Xa. Factor Xa initiates the conversion of prothrombin to thrombin, so enoxaparin’s inhibition of this process results in decreased thrombin and ultimately the prevention of fibrin clot formation.
The usual adult dose to prevent thromboembolism is 40mg subcutaneously once a day. The usual duration of administration is 6 to 11 days; up to 14 days administration has been well tolerated in clinical trials. As a student nurse you will expected to give this medicine and also teach the patient how to administer it to themselves. Enoxaparin should be injected under the skin (SC) usually once or twice a day in the abdomen (at least 50mm from the belly button). It should not be injected into a muscle or vein.
Mild irritation, pain, bruising, redness or swelling at the injection site may occur and the patient should be reassured that this is not unusual. Inform them that fatigue or fever may also occur and that if these effects persist or worsen they should notify their doctor or pharmacist promptly. Many people using this medication do not have serious side-effects. However it can cause bleeding if its effect on blood clotting proteins is too great. The patient should tell their doctor immediately if any of the following unlikely but serious signs occur: unusual pain, swelling, discomfort, unusual or prolonged bleeding, unusual or ‘easy’ bruising, dark urine, black stools, severe headache, confusion, vision changes, dizziness, fainting, seizures, weakness and numbness. A very serious allergic reaction to this drug is unlikely.
This anticoagulant is a naturally occurring protein found in the salivary glands of medicinal leeches. Rather than potentiating the effects of antithrombin III, hirudin is a specific inhibitor of thrombin. The problem with this product is the difficulty in extracting commercial amounts. However, it can now be produced by recombinant techniques – a genetically engineered production of the substance to satisfy demands. It is unclear whether this product will replace heparin or the low molecular weight heparins. However, the drug has the advantage of being less likely to trigger immune thrombocytopenia.
Warfarin
It would stand to reason that if vitamin K is so important to the clotting process, any interference with it would result in that process taking longer. This is the basis of the action of the vitamin K antagonist group of anticoagulants, for example, warfarin. The drug blocks the action of vitamin K and so reduces the manufacture of prothrombin and clotting factors VII, IX and X. The onset of action of warfarin takes several days as the plasma factors that have been manufactured prior to commencement of warfarin take time to be eliminated from the body.
Warfarin is given in tablet form as it is easily absorbed by the GI tract. One of the problems with warfarin is that it is strongly attracted to plasma proteins. These proteins normally help maintain the osmotic intravascular pressure. However, as warfarin is bound to these, potential problems occur with stabilizing the dose, treating elderly people and giving other drugs which compete for binding sites on the plasma proteins − for example, aspirin. The peak pharmacological concentration takes approximately 48 hours. The effectiveness of the drug is measured by a blood test known as the prothrombin time, now expressed as an international normalized ratio or INR. This laboratory test measures the time it takes for blood to clot and compares it to an average. The higher the INR value, the longer it takes for blood to clot.
Warfarin crosses the placenta and therefore should not be given in the first three months of pregnancy as foetal abnormalities may ensue. Intracranial bleeding in the baby may occur during delivery.
As with heparin, the most obvious side-effect is bleeding. This may be due to deliberate or accidental overdose or to the warfarin interacting with other drugs which leads to an increase in its anticoagulant effect. If bleeding does occur the drug may be withdrawn. The anticoagulant effects may be reversed by giving fresh frozen plasma or vitamin K (phytomenadione) intravenously.
A complication of warfarin is a condition referred to as warfarin necrosis, which occurs as a result of a tendency for the blood to clot. This may seem paradoxical as warfarin is given for its anticoagulant effect, however, this drug, by its vitamin K blocking action, not only affects the plasma coagulation previously outlined but also a naturally occurring blood anticoagulant called protein C. Protein C depends on vitamin K and because this is no longer available cannot be manufactured. The problem occurs because protein C initially decreases at a faster rate than the other coagulation factors. This means that at the commencement of therapy the blood has a tendency to coagulate for a short period.
A variety of disease processes and drugs can modify the action of warfarin. Some potentiate the anticoagulant actions while others lessen the effect of the drug. Liver disease, thyrotoxicosis and fever may all interfere with the natural manufacture by the body of clotting factors. If warfarin is given in these cases an increase in anticoagulation occurs. Drugs can also lead to exaggerated anticoagulant effects if given in conjunction with warfarin. Drugs such as Cimetidine can reduce the breakdown of warfarin by liver enzymes. NSAIDs compete successfully with warfarin for a place on plasma proteins, therefore leaving more active drugs in the plasma. Antibiotics are another group of drugs that need careful attention before prescribing because broad spectrum antibiotics and some sulfonamides depress the body’s natural ability to manufacture vitamin K by intestinal flora.
Anticoagulant effects can also be lessened in certain situations. Hypothyroidism is associated with a slower breakdown of coagulation factors. Foods and commercially produced preparations containing high vitamin K content will reduce the warfarin effect. Also, drugs that cause the enzymes in the liver that break down warfarin to increase, such as Carbamazepine, will have the same effect.
Warfarin is a complex drug that needs to be monitored carefully, and good discharge advice is crucial.
Future anticoagulant therapy
Rivaroxaban is the first in a new class of drugs known as oral factor Xa (Stuart-Prower) inhibitors. By inhibiting factor Xa, thrombin production and the formation of clots are ultimately inhibited. Currently rivaroxaban is licensed for the prevention of venous thromboembolism (VTE) in adults undergoing elective hip or knee replacement surgery, at a fixed dose of 10mg daily. The obvious beauty of this drug is that it can be given orally.
Rivaroxaban has predictable pharmacokinetics, with little variation of plasma concentration with age, weight, or renal function following a fixed dose. With a fixed dose, a wide therapeutic window, few drug interactions and predictable pharmacodynamics, no routine monitoring of coagulation parameters is required. Rivaroxaban is well absorbed from the gut and maximum inhibition of factor Xa occurs four hours after a dose. The effects last 8–12 hours, but factor Xa activity does not return to normal within 24 hours so once-daily dosing is possible.
Dabigatran is an anticoagulant from the class of direct thrombin inhibitors. It is being studied for various clinical indications and in some cases offers an alternative to warfarin as the preferred orally administered anticoagulant since it does not require frequent blood tests for INR monitoring while offering similar results in terms of efficacy.
Dabigatran etexilate is a pro-drug with no anticoagulant activity; once absorbed, it is rapidly converted by enzymes in the GI tract, blood and liver into dabigatran, a thrombin inhibitor. Although costly, dabigatran etexilate has several potential advantages over warfarin. The pharmacokinetics are quite predictable, simplifying dosing and eliminating the need for frequent blood tests and monitoring. In addition, the drug requires no dietary restrictions and has relatively few drug interactions (at least that are known at this point). Known potential drug interactions are with quinidine, ketoconazole, amiodarone, rifampicin and verapamil. Peak anticoagulation effects occur between half an hour and two hours after ingestion and dabigatran is primarily eliminated by the kidneys.
Earlier in this chapter we discussed the importance of the formation of a platelet plug in haemostasis. Drugs that affect this important process have strong therapeutic value. Probably the most common and popular in this category is aspirin.
Aspirin
In the platelet plug discussion we highlighted two important substances that work in opposing ways on the stickiness of blood. These are thromboxane, which increases the stickiness, and prostacyclin which decreases the stickiness. Aspirin alters the fine balance between these two prostaglandins. It reduces both substances in the body but because prostacyclin can be made by endothelial cells and thromboxane levels have to wait between 7 and 10 days for new platelets to be made, prostacyclin levels are improved at the expense of thromboxane. Therefore, an anticoagulant effect is achieved. Aspirin does have a number of serious side-effects but these are limited as it is given at a low dose for its anticoagulant effect. A dose of 75mg daily is sufficient to achieve anticoagulation, in comparison to a dose of 300mg daily which would be prescribed in aspirin’s role as an analgesic. Aspirin may be given for a number of conditions, including coronary thrombosis, angina and following transient ischaemic attacks or stroke. A drug by the name of Dipyridamole also prevents platelets sticking together. This drug in combination with aspirin has been shown to be effective in reducing the risk of stroke.
Clopidogrel
This is a fairly new and powerful antiplatelet medicine. You may come across it in your placements, being used for a variety of conditions including coronary artery disease, peripheral vascular disease and cerebrovascular disease.
The drug works by blocking receptor sites on the platelets. This means that when fibrin is formed it cannot stick to the platelet so the plug to block bleeding does not occur as the platelets cannot clump together. It is sometimes used alongside aspirin.
Clopidogrel can be given orally and is normally prescribed at 75mg once per day. It is a pro-drug activated by the liver when it first passes through. Once the drug has been activated its elimination half life is eight hours. The drug reaches a peak level in the blood after one hour.
Abciximab
As described earlier the final part of the platelet plug formation is the depositing of substances on platelets that allows fibrin strands to anchor to them. Abciximab interferes with this process. It is given intravenously and usually only indicated in high risk patients undergoing certain invasive procedures such as coronary angioplasty. Because of its risk of causing an immune response its use is usually limited to one dose only.
Fibrinolytic drugs
These drugs mimic the body’s own ability to dissolve blood clots. A number of drugs are used in practice that dissolve clots in order to allow free passage of blood back to an area that has been starved of blood (i.e. that is ischaemic). The main use is in patients who have had acute myocardial infarction following blockages of the coronary artery.
Streptokinase
This drug is used to dissolve the fibrin of blood clots, especially those that occur in the heart and lungs. Acute myocardial infarction results from blockage of a coronary artery, which results in an area of heart muscle being deprived of blood. Streptokinase is used in breaking down such clots in the coronary vessels.
The drug triggers the plasma protein plasminogen to liberate plasmin, which breaks down fibrin, so dissolving the clot. The drug is extracted from bacteria called haemolytic streptococci. It has a short half life of less than 20 minutes and is therefore given by continuous IV infusion. Most people will have developed antibodies to streptococcal proteins, so often a large bolus dose is used to start therapy, followed by a maintenance infusion. As antibodies form against the streptococcal proteins it is usually best not to give another treatment with the drug until a year has elapsed. Also, due to the body’s immune response, other drugs, such as chlorphenamine or hydrocortisone, may be given to reduce any allergic response.
Alteplase
This drug is derived from human tissue plasminogen activator. Therefore, it directly converts plasminogen to plasmin. It binds strongly with fibrin and digests clots in coronary arteries at least as well if not better than streptokinase. It has the advantages of not causing immune responses and, having a greater attraction to fibrin-bound plasminogen rather than circulating plasma fibrinogen, is said to be ‘clot selective’. As with streptokinase, the drug has a short half life and is therefore given by IV infusion. Even though alteplase is less likely to cause bleeding, it is contraindicated in pregnancy, uncontrolled hypertension, haemorrhagic cerebrovascular disease and active internal bleeding. If bleeding occurs it can be treated with tranexamic acid. This stops plasminogen activation and therefore prevents clots dissolving. The patient may also be given fresh plasma or coagulation factors.
Recommended further reading
Beckwith, S. and Franklin, P. (2007) Oxford Handbook of Nurse Prescribing. Oxford: Oxford University Press.
Brenner, G.M. and Stevens, C.W. (2006) Pharmacology, 2nd edn. Philadelphia, PA: Saunders Elsevier.
Casey, G. (2003) Continuing professional development: haemostasis, anticoagulants and fibrinolysis, Nursing Standard, 18: 45–51.
Clayton, B.D. (2009) Basic Pharmacology for Nurses, 15th edn. St Louis, MO: Mosby Elsevier.
Coben, D. and Atere-Roberts, E. (2005) Calculations for Nursing and Healthcare, 2nd edn. Basingstoke: Palgrave Macmillan.
Downie, G., Mackenzie, J. and Williams, A. (2007) Pharmacology and Medicines Management for Nurses, 4th edn. Edinburgh: Churchill Livingstone.
Gallagher, D. and Rix, E. (2006) Understanding the implications of oral anticoagulation therapy, Nursing Times, 102: 30–2.
Gatford, J.D. and Phillips, N. (2006) Nursing Calculations, 7th edn. Edinburgh: Churchill Livingstone Elsevier.
Karch, A.M. (2008) Focus on Nursing Pharmacology, 4th edn. Philadelphia, PA: Lippincott Williams & Wilkins.
Lake, R. and Jordan, S. (2005) Prescription drugs: uses and effects, anticoagulants, Nursing Standard, 19(19).
Lapham, R. and Agar, H. (2003) Drug Calculations for Nurses: A Step-by-step Approach, 2nd edn. London: Arnold.
NICE (National Institute for Health and Clinical Excellence) (2006) Clinical Guideline 36: Atrial Fibrillation. London: NICE.
NICE (National Institute for Health and Clinical Excellence) (2007) Clinical Guideline 48: Secondary Prevention of Myocardial Infarction. London: NICE.
NICE (National Institute for Health and Clinical Excellence) (2008) Technology Appraisal TA 157: Dabigatran Etexilate for the Prevention of Venous Thromboembolism After Hip or Knee Replacement Surgery in Adults. London: NICE.
NICE (National Institute for Health and Clinical Excellence) (2009) Technology Appraisal TA 170: Rivaroxaban for the Prevention of Venous Thromboembolism. London: NICE.
Simonson, T., Aarbakke, J., Kay, I., Coleman, I., Sinnott, P. and Lyssa, R. (2006) Illustrated Pharmacology for Nurses. London: Hodder Arnold.
Trounce, J. (2000) Clinical Pharmacology for Nurses, 16th edn. New York: Churchill Livingstone.
< div class='tao-gold-member'>