DRUG CLASSES
Benzodiazepines
Nonbenzodiazepines
Anxiety is a feeling of apprehension, worry, or uneasiness that may or may not be based on reality. Anxiety may be seen in many types of situations, ranging from the “jitters” and excitement of a new job to the acute panic that may be seen during withdrawal from alcohol. Although a certain amount of anxiety is normal, excess anxiety interferes with day-to-day functioning and can cause undue stress in the lives of some individuals. Drugs used to treat anxiety are called antianxiety drugs. Anxiolytics is another term you may see referring to the antianxiety drugs.
Antianxiety drug classes include the benzodiazepines and the nonbenzodiazepines. Examples of the benzodiazepines include alprazolam (Xanax), chlordiazepoxide (Librium), diazepam (Valium), and lorazepam (Ativan). Long-term use of benzodiazepines can result in physical or psychological dependence, and as a result they are classified as schedule IV controlled substances (see Chapter 1). Due to the risk of dependence, benzodiazepines are used for short-term anxiety relief. Typically, long-term psychiatric anxiety disorders such as posttraumatic stress disorder (PTSD) are treated with antidepressant medications (Chapter 22). The nonbenzodiazepines useful in reducing anxiety include buspirone, doxepin, and hydroxyzine.
PHARMACOLOGY IN PRACTICE

Mr. Garcia, 55 years of age, is being seen in the clinic for an upper respiratory infection. Using an interpreter, he tells you that his shortness of breath makes him anxious. His respirations are 32 breaths/min, heart rate 98 beats/min, and blood pressure 161/92 mm Hg. The primary health care provider prescribes alprazolam (Xanax) 0.25 mg orally three times a day. As you read this chapter, determine if this is appropriate.
Actions
Anxiolytic drugs exert their tranquilizing effect by blocking certain neurotransmitter receptor sites. In turn, this prevents the neurotransmission of the anxious perception and the body’s physical reaction to the anxiety. Benzodiazepines exert their tranquilizing effect by potentiating the effects of gamma (γ)-aminobutyric acid (GABA), an inhibitory transmitter (Fig. 20.1). Nonbenzodiazepines exert their action in various ways. For example, buspirone is thought to act on the brain’s serotonin receptors. Hydroxyzine (Vistaril) produces its antianxiety effect by acting on the hypothalamus and brainstem reticular formation.
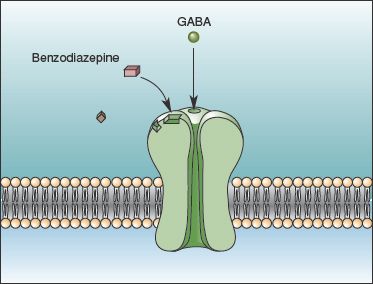
Figure 20.1 Benzodiazepine drugs bind to a site on the cell receptor, potentiating the effect of GABA (an inhibitory neurotransmitter) on the receptor. (Adapted from Bear, M. F., Connors, B. W., & Parasido, M. A. [2001]. Neuroscience—exploring the brain [2nd ed.]. Philadelphia: Lippincott Williams & Wilkins.)
Uses
Antianxiety drugs are used in the management of the following:
• Anxiety disorders and panic attacks
• Preanesthetic sedation and muscle relaxation
• Convulsions or seizures
• Alcohol withdrawal
Adverse Reactions
Frequent, early reactions include:
• Mild drowsiness or sedation
• Lightheadedness or dizziness
• Headache
Other adverse body system reactions include:
• Lethargy, apathy, fatigue
• Disorientation
• Anger
• Restlessness
• Nausea, constipation or diarrhea, dry mouth
• Visual disturbances
See the Summary Drug Table: Antianxiety Drugs for more information.
Dependence
Long-term use of benzodiazepines may result in physical dependence and tolerance (increasingly larger dosages required to obtain the desired effect). Withdrawal symptoms have occurred when the drug is stopped after as few as 4 to 6 weeks of therapy. When discontinuing a benzodiazepine a gradually decreasing dosage schedule (known as tapering) should be used.
 NURSING ALERT
NURSING ALERT
Withdrawal symptoms are more likely to occur when the benzodiazepine is taken for 3 months or more and is abruptly discontinued. Therefore, antianxiety drugs must never be discontinued abruptly.
Symptoms of benzodiazepine withdrawal include increased anxiety, concentration difficulties, tremor, and sensory disturbances, such as paresthesias, photophobia, hypersomnia, and metallic taste. The onset of withdrawal symptoms usually occurs within 1 to 10 days after discontinuing the drug, with the duration of withdrawal symptoms from 5 days to 1 month. Symptoms of withdrawal are identified in Display 20.1.
The nonbenzodiazepine antianxiety drug buspirone is associated with less physical dependence potential and less effect on motor ability and cognition.
Contraindications
Do not administer antianxiety drugs to patients with known hypersensitivity, psychoses, and acute narrow-angle glaucoma. The benzodiazepines are contraindicated during pregnancy (pregnancy category D drugs) and labor. Reports of floppy infant syndrome manifested by sucking difficulties, lethargy, and hypotonia have been seen in the newborn. Lactating women should also avoid the benzodiazepines because of the effect on the infant (lethargy and weight loss). Due to a specific enzyme reaction, grapefruit or its juice should not be taken if the patient is on buspirone and diazepam.
Buspirone is a pregnancy category B drug and hydroxyzine is a pregnancy category C drug. Their safety is still questionable because adequate studies have not been performed in pregnant women. All of these drugs are contraindicated when patients are in a coma or shock, and if the vital signs of the patient in acute alcoholic intoxication are low.
Display 20.1 Symptoms of Withdrawal
• Increased anxiety
• Fatigue
• Hypersomnia
• Metallic taste
• Concentration difficulties
• Headache
• Tremors
• Numbness in the extremities
• Nausea
• Sweating
• Muscle tension and cramps
• Psychoses
• Hallucinations
• Memory impairment
• Convulsions (possible)
Precautions
Antianxiety drugs are used cautiously in elderly patients and in patients with impaired liver function, impaired kidney function, or debilitation.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Recent studies link the chronic use of benzodiazepines by those older than 65 years of age to a greater chance of developing dementia (Billioti, 2012).
Interactions
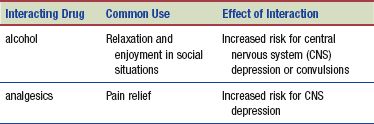
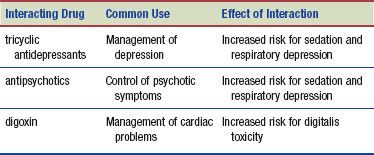
The following interactions may occur when an anxiolytic is administered with another agent:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Kava is a popular herbal remedy thought to relieve stress, anxiety, and tension; promote sleep; and provide relief from menstrual discomfort. Kava’s benefits are not supported by science, and the U.S. Food and Drug Administration (FDA) has issued an alert indicating that the use of kava may cause liver damage. Because kava-containing products have been associated with liver-related injuries (e.g., hepatitis, cirrhosis, and liver failure), the safest way to use kava is to take the herb occasionally for episodes of anxiety, rather than on a daily basis. It is important that individuals who use a kava-containing dietary supplement and experience signs of liver disease immediately consult their primary health care provider. Identifying kava-containing products can be difficult. Careful reading of the “Supplement Facts” information on the label may identify kava by any of the following names: kava, ava, ava pepper, awa, kava root, kava-kava, kew, Piper methysticum G. Forst, Piper methysticum, Sakau, tonga, or yanggona (FDA Consumer Advisory, 2009).
NURSING PROCESS
PATIENT TEACHING FOR MEDICATION INFORMATION
ASSESSMENT
Preadministration Assessment
Individuals with mild anxiety or depression do not necessarily require inpatient care. These patients are usually seen at periodic intervals in the primary health care provider’s office or in a mental health outpatient setting. Treatment for anyone in the hospital or in an outpatient setting may be anxiety provoking, especially if the individual has reduced health literacy (Fig. 20.2). Assessment of both patient groups is similar.
When an antianxiety drug is ordered, obtain as complete of a medical history as possible, including mental status and anxiety level. Because anxiety is a subjective feeling, you may ask the patient to rate his or her anxiety on a 0 to 10 scale, just as you would when asking about pain. When in a state of mild to moderate anxiety, patients may be able to give a reliable history of their illness.
Yet, when severe anxiety is present, the patient may be unable to communicate effectively. Therefore, it is important to seek information from a family member or friend when possible. During the intake exam, observe for behavioral signs indicating anxiety (e.g., inability to focus, extreme restlessness, facial grimaces, tense posture).
Physical assessment should include the blood pressure, pulse, respiratory rate, and weight. Physiologic manifestations of anxiety can include increased blood pressure and pulse rate, increased rate and depth of respiration, and increased muscle tension. An anxious patient may have cool and pale skin.
Be sure to obtain a history of any past drug or alcohol use. This information can help establish what the patient has used in the past as coping mechanisms to deal with anxiety. More accurate intake information is obtained when using questions such as “How much alcohol do you drink daily?” or “Do you drink more or less than three alcohol beverages daily?”

Figure 20.2 Hospitalization can be an anxious experience for patients. Anxiolytic medications can help the patient focus on patient teaching and activities of daily living to improve patient outcomes.
Ongoing Assessment
An ongoing assessment is important for the patient taking an antianxiety drug. Ask the patient to rate the anxiety and compare this to the baseline rating. Check the patient’s blood pressure before drug administration. If systolic pressure has dropped 20 mm Hg, withhold the drug because the patient is at greater risk to fall, and notify the primary health care provider. Periodically monitor the patient’s mental status and anxiety level during therapy and assess for improvement or decline of behavioral and functional ability.
During follow-up in the ambulatory setting, ask the patient or a family member about adverse drug reactions or any other problems occurring during therapy. Flag these reactions or problems to be sure they come to the attention of the primary health care provider. Describe and document outward behavior and any complaints or problems in the patient’s record. Compare your new information with previous notations and observations.
NURSING DIAGNOSES
Drug-specific nursing diagnoses are the following:
 Risk for Injury related to dizziness or hypotension and gait problems
Risk for Injury related to dizziness or hypotension and gait problems
 Impaired Comfort related to dryness in gastrointestinal (GI) tract from medications
Impaired Comfort related to dryness in gastrointestinal (GI) tract from medications
 Ineffective Individual Coping related to situation causing anxiety
Ineffective Individual Coping related to situation causing anxiety
Nursing diagnoses related to drug administration are discussed in Chapter 4.
PLANNING
The expected patient outcomes may include an optimal response to drug therapy, support of patient needs related to the management of adverse drug reactions, and confidence in an understanding of the medication regimen.
IMPLEMENTATION
Promoting an Optimal Response to Therapy
During initial therapy, observe the patient closely for adverse drug reactions. Some adverse reactions, such as episodes of postural hypotension and drowsiness or dry mouth, may need to be tolerated because drug therapy must continue. The antianxiety drugs are not recommended for long-term use. When the antianxiety drugs are used for short periods (1 to 2 weeks), tolerance, dependence, or withdrawal symptoms usually do not develop. Should any signs of tolerance or dependence, such as the patient needing larger doses of drug or complaints of increased anxiety and agitation (see Display 20.1) develop, contact the primary health care provider.
Monitoring and Managing Patient Needs
RISK FOR INJURY. When these drugs are given in the outpatient setting, instruct both the patient and family about adverse reactions (dizziness, lightheadedness, or ataxia) that can cause a patient to fall and become injured. This is very important when the drugs are administered to older adults.
 LIFESPAN CONSIDERATIONS
LIFESPAN CONSIDERATIONS
Gerontology
Benzodiazepines are excreted more slowly in older adults, causing a prolonged drug effect. The drugs may accumulate in the blood, resulting in an increase in adverse reactions or toxicity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


